Abstract
Background
The worldwide prevalence of obesity nearly tripled between 1975 and 2016. There are limited data quantifying national trends. The aim of this study is to evaluate and summarize current trends in bariatric surgery in Israel.
Methods
Data for all bariatric surgeries (BS) performed between January 2014 and December 2018 was collected from the Israel National Bariatric Surgery Registry (INBSR) and analyzed.
Results
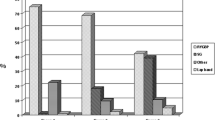
During the study period, 42,296 BS were included in the INBSR. Females accounted for 68% and the mean age and body mass index were 41.6 ± 12.6 years and 42.0 ± 5.4 kg/m2, respectively. Most of the patients were Jewish, but there was a significant rise in number of Arabs undergoing BS during the study period. There was a gradual decline in the annual numbers of BS, except for a small rise in 2015. There was a significant rise in the rate of One Anastomosis-Mini Gastric Bypass (OAGB-MGB), from 0.1% in 2014 to 46.1% in 2018, making it the most prevalent BS in that year. Laparoscopic sleeve gastrectomy (SG) surgeries decreased steadily, from 80% in 2014 to 37% in 2018. The annual rate of Roux-en-Y gastric bypass (RYGB) remained essentially constant at 10%. The annual rates of gastric banding decreased sharply and the annual rates of duodenal switch, single anastomosis duodenal switch and biliopancreatic diversion were negligible. Bariatric surgery was distributed evenly between private (50.4%) and public (49.6%) hospitals.
Conclusions
The numbers of BS are decreasing in Israel. There is a gradual but noticeable shift from SG to OAGB-MGB.

Similar content being viewed by others
References
WHO: World Health Organiztion [Internet]. [Place unknown]: Obesity and overweight. World Health Organization; 2018 Feb 16 [cited 2019 Oct. 10]. Available from: www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight.
Sjostrom L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93.
Samuel I, Mason EE, Renquist KE, et al. Bariatric surgery trends: an 18-year report from the International Bariatric Surgery Registry. Am J Surg. 2006;192(5):657–62.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Marsk R, Freedman J, Tynelius P, et al. Antiobesity surgery in Sweden from 1980 to 2005: a population-based study with a focus on mortality. Ann Surg. 2008;248(5):777–81.
Nguyen NT, Masoomi H, Magno CP, et al. Trends in use of bariatric surgery, 2003-2008. J Am Coll Surg. 2011;213(2):261–6.
ICDC: Israel Center for Disease Control [ Internet]. Israel National Health Interview Survey INHIS-1, 2003–2004 – selected findings. Israel Center for Disease Control, Ministry of Health. Publication. 249, 2006 [cited 2019 Oct. 10]. Available from: https://www.health.gov.il/publicationsfiles/inhis_1.pdf .
ICDC: Israel Center for Disease Control [ Internet]. Israel National Health Interview Survey INHIS-3, 2013–2015 – selected findings. Israel Center for Disease Control, Ministry of Health. Publication. 374, Sept. 2017 [cited 2019 Oct. 10]. Available from : https://www.health.gov.il/PublicationsFiles/INHIS_3.pdf. Hebrew.
Eisenman Y. Israel central Bureau of Statistics [internet]. Selected data on health and way of life, from the 2017 social survey: weight, dieting, nutrition and eating habits. Central Bureau of Statistics, 2018 Sepy. 3 [cited 2019 Oct. 10]. Available from : https://www.cbs.gov.il/he/mediarelease/DocLib/2018/262/19_18_262b.pdf. Hebrew.
Himpens J, Ramons A, Welbourn R, et al. Fourth IFSO global registry report. Reading: Dendrite Clinical Systems Ltd.; 2018.
BOMSS: British Obesity & Metabolic Surgery Society [Internet]. Bariatric Surgery Clinical Outcomes Publication 2017–18. The United Kingdom National Bariatric Surgery Registry. 2019 Aug. 1 [cited 2019 Oct. 10]. Available from : https://www.bomss.org.uk/clinical-outcomes-2017-18/.
Sakran N, Goitein D, Raziel A, et al. Gastric leaks after sleeve gastrectomy: a multicenter experience with 2,834 patients. Surg Endosc. 2013;27(1):240–5.
Al-Kurd A, Grinbaum R, Abubeih A, et al. Not all leaks are created equal: a comparison between leaks after sleeve gastrectomy and Roux-en-Y gastric bypass. Obes Surg. 2018;28(12):3775–82.
Sakran N, Sherf-Dagan S, Blumenfeld O, et al. Incidence and risk factors for mortality following bariatric surgery: a nationwide registry study. Obes Surg. 2018;28(9):2661–9.
Antoniewicz A, Kalinowski P, Kotulecka KJ, et al. Nutritional deficiencies in patients after Roux-en-Y gastric bypass and sleeve gastrectomy during 12-month follow-up. Obes Surg. 2019;29(10):3277–84.
Lupoli R, Lembo E, Saldalamacchia G, et al. Bariatric surgery and long-term nutritional issues. World J Diabetes. 2017;8(11):464–74.
Borbely Y, Schaffner E, Zimmermann L, et al. De novo gastroesophageal reflux disease after sleeve gastrectomy: role of preoperative silent reflux. Surg Endosc. 2019;33(3):789–93.
Yeung KTD, Penney N, Ashrafian L, Darzi A, Ashrafian H. Does sleeve gastrectomy expose the distal esophagus to severe reflux?: a systematic review and meta-analysis. Ann Surg. 2020;271(2):257–265.
Genco A, Soricelli E, Casella G, et al. Gastroesophageal reflux disease and Barrett's esophagus after laparoscopic sleeve gastrectomy: a possible, underestimated long-term complication. Surg Obes Relat Dis. 2017;13(4):568–74.
Golomb I, Ben David M, Glass A, et al. Long-term metabolic effects of laparoscopic sleeve gastrectomy. JAMA Surg. 2015;150(11):1051–7.
Carbajo MA, Luque-de-Leon E, Jimenez JM, et al. Laparoscopic one-anastomosis gastric bypass: technique, results, and long-term follow-up in 1200 patients. Obes Surg. 2017;27(5):1153–67.
Georgiadou D, Sergentanis TN, Nixon A, et al. Efficacy and safety of laparoscopic mini gastric bypass. A systematic review. Surg Obes Relat Dis. 2014;10(5):984–91.
Robert M, Espalieu P, Pelascini E, et al. Efficacy and safety of one anastomosis gastric bypass versus Roux-en-Y gastric bypass for obesity (YOMEGA): a multicentre, randomised, open-label, non-inferiority trial. Lancet. 2019;393(10178):1299–309.
Sanchez-Santos R, Estevez S, Tome C, et al. Training programs influence in the learning curve of laparoscopic gastric bypass for morbid obesity: a systematic review. Obes Surg. 2012;22(1):34–41.
Doumouras AG, Saleh F, Anvari S, et al. Mastery in bariatric surgery: the long-term surgeon learning curve of Roux-en-Y gastric bypass. Ann Surg. 2018;267(3):489–94.
Lazzati A, Guy-Lachuer R, Delaunay V, et al. Bariatric surgery trends in France: 2005-2011. Surg Obes Relat Dis. 2014;10(2):328–34.
Abraham A, Ikramuddin S, Jahansouz C, et al. Trends in bariatric surgery: procedure selection, revisional surgeries, and readmissions. Obes Surg. 2016;26(7):1371–7.
English WJ, DeMaria EJ, Brethauer SA, et al. American Society for Metabolic and Bariatric Surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis. 2018;14(3):259–63.
Welbourn R, Hollyman M, Kinsman R, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the fourth IFSO global registry report 2018. Obes Surg. 2019;29(3):782–95.
Welbourn R, Pournaras DJ, Dixon J, et al. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the second IFSO global registry report 2013-2015. Obes Surg. 2018;28(2):313–22.
Longitudinal Assessment of Bariatric Surgery (LABS) Consortium. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009;361(5):445–54.
Lecube A, de Hollanda A, Calanas A, et al. Trends in bariatric surgery in Spain in the twenty-first century: baseline results and 1-month follow up of the RICIBA, a National Registry. Obes Surg. 2016;26(8):1836–42.
Bockelman C, Hahl T, Victorzon M. Mortality following bariatric surgery compared to other common operations in Finland during a 5-year period (2009-2013). A Nationwide Registry Study. Obes Surg. 2017;27(9):2444–51.
Kelles SM, Barreto SM, Guerra HL. Mortality and hospital stay after bariatric surgery in 2,167 patients: influence of the surgeon expertise. Obes Surg. 2009;19(9):1228–35.
Martin II RC, Brennan MF, Jaques DP. Quality of complication reporting in the surgical literature. Ann Surg. 2002;235(6):803–13.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Human Rights
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kaplan, U., Romano-Zelekha, O., Goitein, D. et al. Trends in Bariatric Surgery: a 5-Year Analysis of the Israel National Bariatric Surgery Registry. OBES SURG 30, 1761–1767 (2020). https://doi.org/10.1007/s11695-020-04426-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04426-2