Abstract
Background
The medium-term impact of gastric bypass (GB) surgery on the inflammatory state and endothelial function of patients has yet to be confirmed.
Objective
This study aims to elucidate the inflammatory profile and endothelial dysfunction response of adults with obesity 6 and 24 months after undergoing GB surgery.
Methods
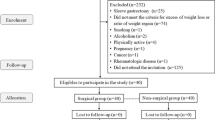
The anthropometric and biochemical markers of 32 adults with obesity (two men and 30 females) were collected preoperatively, and 6 and 24 months postoperatively.
Results
Body mass index (BMI) and excess weight had decreased by 15.79 ± 1.21 kg/m2 (p < 0.01) and 83.80 ± 24.50% respectively at 24 months. Leptin, C-reactive protein (CRP), plasminogen activator inhibitor-1 (PAI-1) levels, and the leptin/adiponectin ratio decreased significantly at both postoperative follow-up points compared with preoperative values (p < 0.01). IL-6 and ICAM-1 levels decreased between 6 and 24 months post-GB (p < 0.01). IL-6 and ICAM-1 levels decreased between 6- and 24-months post-GB (p < 0.01). Resistin levels were significantly decreased (p < 0.01) at 6-month follow-up. The levels of the anti-inflammatory biomarkers IL-10, adiponectin, and the adiponectin/leptin ratio significantly increased postoperatively. There was an improvement in metabolic disorders after surgery.
Conclusion
Our results demonstrated that after GB there was an improvement in the inflammatory profile, identified by a reduction in pro-inflammatory markers (CRP, IL-6, leptin) and an increase in anti-inflammatory markers (adiponectin, IL-10). The decrease in PAI-1 and ICAM-1 levels may suggest improvement in endothelial function. These findings provide clear evidence of the medium-term impact of GB on inflammation state and a number of endothelial markers, and a consequent reduction in the risk of cardiovascular diseases.



Similar content being viewed by others
References
Vilahur G, Ben-Aicha S, Badimon L. New insights into the role of adipose tissue in thrombosis. Cardiovasc Res. 2017;113(9):1046–54.
Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde, Secretaria de Gestão Estratégica e Participativa. Vigitel Brasil 2018: vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico. Brasília: Ministério da Saúde, 2019. Disponível em: < https://portalarquivos2.saude.gov.br/images/pdf/2019/julho/25/vigitel-brasil-2018.pdf > Acesso em: 15 set. 2019.
WHO (World Health Organization). Obesity and overweight. Key facts. Fact sheet no. 311; February, 2018. Disponível em: <http://www.who.int/mediacentre/factsheets/fs311/en/index.html> Acesso em: 02 jul. 2019.
RakotoArivelo V et al. Inflammatory cytokine profiles in visceral and subcutaneous adipose tissues of obese patients undergoing bariatric surgery reveal lack of correlation with obesity or diabetes. EBioMedicine. 2018;30:237–47.
Unamuno X et al. Adipokine dysregulation and adipose tissue inflammation in human obesity. Eur J Clin Investig. 2018;48:e12997–3008.
Villarroya F et al. Inflammation of brown/beige adipose tissues in obesity and metabolic disease. J Intern Med. 2018;2018:1–13.
Illán-Gomez F et al. Obesity, endothelial function and inflammation: the effects of weight loss after bariatric surgery. Nutr Hosp. 2016;33(6):1340–6.
Chiapetta S et al. The impact of obesity and metabolic surgery on chronic inflammation. Obes Surg. 2018;28:3028–40.
Angrisani L et al. IFSO Worldwide Survey 2016: primary, endoluminal, and revisional procedures. Obes Surg. 2018;28:3783–94.
Yadav R et al. Effect of Roux-en-Y bariatric surgery on lipoproteins, insulin resistance, and systemic and vascular inflammation in obesity and diabetes. Front Immunol. 2017;8:1–7.
Stolberg CR et al. Effects of gastric bypass surgery followed by supervised physical training on inflammation and endothelial function: a randomized controlled trial. Atherosclerosis. 2018;273:37–44.
Khosravi-Largani M et al. Evaluation of all types of metabolic bariatric surgery and its consequences: a systematic review and meta-analysis. Obes Surg. 2019;29:651–90.
Adami GF, Scopinaro N, Cordera R. Adipokine pattern after bariatric surgery: beyond the weight loss. Obes Surg. 2016;26:2793–801.
Bachmayer C et al. Healthy obese and post bariatric patients – metabolic and vascular patterns. Exp Clin Endocrinol Diabetes. 2013;121:483–7.
Auguet T et al. Clinical and adipocytokine changes after bariatric surgery in morbidly obese women. Obesity (Silver Spring). 2014;22:188–94.
Deitel M, Gawdat K, Melissas J. Reporting weight loss 2007. Obes Surg. 2007;17:565–8.
Matthews DR et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Katz A et al. Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab. 2000;85:2402–10.
Netto BDM et al. Roux-en-Y gastric bypass decreases pro-inflammatory and thrombotic biomarkers in individuals with extreme obesity. Obes Surg. 2015;25(6):1010–8.
Farias G et al. Neuroendocrine regulation of energy balance: implications on the development and surgical treatment of obesity. Nutr Health. 2017;23:131–46.
Askarpour M, Khani D, Sheikhi A, et al. Effect of bariatric surgery on serum inflammatory factors of obese patients: a systematic review and meta-analysis. Obes Surg. 2019;29:2631–47.
Unamuno X et al. Increase of the adiponectin/leptin ratio in patients with obesity and type 2 diabetes after Roux-en-Y gastric bypass. Nutrients. 2019;11:2069.
Fruhbeck G et al. Adiponectin-leptin ratio: a promising index to estimate adipose tissue dysfunction. Relation with obesity-associated cardiometabolic risk. Adipocyte. 2018;7:57–62.
Frikke-Schmidt H et al. Does bariatric surgery improve adipose tissue function? Obes Rev. 2016;17(9):795–809.
Malden D et al. Body fat distribution and systolic blood pressure in 10,000 adults with whole-body imaging: UK Biobank and Oxford BioBank. Obesity. 2019;27:1200–6.
Vest AR et al. Bariatric surgery and cardiovascular outcomes: a systematic review. Heart. 2012;98:1763–77.
Wilhelm SM, Young J, Kale-Pradhan PB. Effect of bariatric surgery on hypertension: a meta-analysis. Ann Pharmacother. 2014;48:674–82.
Lager CJ et al. Metabolic parameters, weight loss, and comorbidities 4 years after Roux-en-Y gastric bypass and sleeve gastrectomy. Obes Surg. 2018;28:3415–23.
Lira NS et al. Análise do perfil lipídico de pacientes submetidos à gastrectomia vertical e à derivação gástrica em Y de Roux. Rev Col Bras Cir. 2018;45:e1967.
Schiavon CA et al. Effects of bariatric surgery in obese patients with hypertension. Circulation. 2018;137:1132–42.
Pareek M et al. Metabolic surgery for hypertension in patients with obesity. Circ Res. 2019;124:1009–24.
Funding
Grant No. 2013/04136-4 São Paulo Research Foundation (FAPESP) and CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior) supported the Hospital de Clínicas/Federal University of Paraná (UFPR).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Farias, G., Netto, B.D.M., Boritza, K. et al. Impact of Weight Loss on Inflammation State and Endothelial Markers Among Individuals with Extreme Obesity After Gastric Bypass Surgery: a 2-Year Follow-up Study. OBES SURG 30, 1881–1890 (2020). https://doi.org/10.1007/s11695-020-04411-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04411-9