Abstract
Background
The concept of metabolic obesity phenotypes has been proposed, but its relevance to metabolic features is unclear.
Purpose
To determine a new definition of metabolic obesity phenotype, investigate the characteristics of expressing clustered normal and abnormal metabolic parameters, and analyze factors associated with metabolic abnormalities.
Materials and Methods
Characteristics of 600 patients were analyzed. The definition of metabolic obesity phenotype includes elevated blood pressure, glucose, lipid, and uric acid levels and abnormal lipoprotein levels. Independent sample t test and a general linear model with repeated measures were applied to investigate the differences in metabolic parameters.
Results
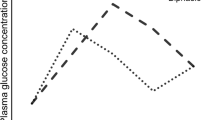
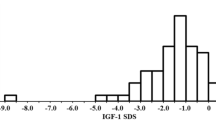
A total of 108 (18.0%) participants were obese yet metabolically healthy, whereas 492 (82.0%) were obese and metabolically unhealthy. Body weight at baseline was significantly higher in metabolically unhealthy phenotype (P < 0.001). For non-phasic oral glucose tolerance test (OGTT) curve shape, 100% glucose, 100% C-peptide, and 95.8% insulin curves were found in the metabolically unhealthy group. Men had an increased risk for elevated lipid level than women (OR = 1.83, 1.21–2.77). Individuals with class II/III obesity had an increased risk for elevated blood pressure, glucose, and UA levels than did those with class I obesity (OR = 2.22, 1.43–3.44; OR = 1.73, 1.11–2.68; OR = 3.61, 2.29–5.69, respectively).
Conclusions
Approximately one-fifth of individuals with obesity had a metabolically healthy phenotype, and nearly one-third of individuals with class III obesity had this phenotype. Non-phasic OGTT curve shape is a meaningful predictive factor of metabolically unhealthy phenotype before bariatric surgery. Male sex and class II/III obesity are risk factors associated with specific metabolic abnormalities.



Similar content being viewed by others
Change history
18 May 2020
In the original articles there are data errors in some of the Figure 2 tables. The corrected Figure 2 tables follow.
References
Collaboration, N.C.D.R.F. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387(10026):1377–96.
Bray GA, Heisel WE, Afshin A, et al. The science of obesity management: an Endocrine Society scientific statement. Endocr Rev. 2018;39(2):79–132.
Arterburn D, Courcoulas A. Bariatric surgery for obesity and metabolic conditions in adults. BMJ. 2014;349:g3961.
Christ JP, Falcone T. Bariatric surgery improves Hyperandrogenism, menstrual irregularities, and metabolic dysfunction among women with polycystic ovary syndrome (PCOS). Obes Surg. 2018;28:2171–7.
Sung H, et al. Global patterns in excess body weight and the associated cancer burden.CA Cancer J Clin, 2018.
Garvey WT et al. American association of clinical endocrinologists and american college of endocrinology position statement on the 2014 advanced framework for a new diagnosis of obesity as a chronic disease. Endocr Pract. 2014;20(9):977–89.
Garvey WT, Mechanick JI, Brett EM, et al. American Association of Clinical Endocrinologists and American College of endocrinology comprehensive clinical practice guidelines for medical Care of Patients with obesity. Endocr Pract. 2016;22(Suppl 3):1–203.
Roberson LL, Aneni EC, Maziak W, et al. Beyond BMI: the "metabolically healthy obese" phenotype & its association with clinical/subclinical cardiovascular disease and all-cause mortality -- a systematic review. BMC Public Health. 2014;14:14.
Wildman RP, Muntner P, Reynolds K, et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999-2004). Arch Intern Med. 2008;168(15):1617–24.
Appleton SL, Seaborn CJ, Visvanathan R, et al. Diabetes and cardiovascular disease outcomes in the metabolically healthy obese phenotype: a cohort study. Diabetes Care. 2013;36(8):2388–94.
Kramer CK, Zinman B, Retnakaran R. Are metabolically healthy overweight and obesity benign conditions?: a systematic review and meta-analysis. Ann Intern Med. 2013;159(11):758–69.
Mathew H, Farr OM, Mantzoros CS. Metabolic health and weight: understanding metabolically unhealthy normal weight or metabolically healthy obese patients. Metabolism. 2016;65(1):73–80.
Lotta LA, Abbasi A, Sharp SJ, et al. Definitions of metabolic health and risk of future type 2 diabetes in BMI categories: asystematic review and network meta-analysis. Diabetes Care. 2015;38(11):2177–87.
Karelis AD, Rabasa-Lhoret R. Inclusion of C-reactive protein in the identification of metabolically healthy but obese (MHO) individuals. Diabetes Metab. 2008;34(2):183–4.
Stefan N, Häring HU, Hu FB, et al. Metabolically healthy obesity: epidemiology, mechanisms, and clinical implications. Lancet Diabetes Endocrinol. 2013;1(2):152–62.
Stefan N, Haring HU, Schulze MB. Metabolically healthy obesity: the low-hanging fruit in obesity treatment? Lancet Diabetes Endocrinol. 2018;6(3):249–58.
Hinnouho GM, Czernichow S, Dugravot A, et al. Metabolically healthy obesity and the risk of cardiovascular disease and type 2 diabetes: the Whitehall II cohort study. Eur Heart J. 2015;36(9):551–9.
Heianza Y, Arase Y, Tsuji H, et al. Metabolically healthy obesity, presence or absence of fatty liver, and risk of type 2 diabetes in Japanese individuals: Toranomon hospital health management center study 20 (TOPICS 20). J Clin Endocrinol Metab. 2014;99(8):2952–60.
Heianza Y, Kato K, Kodama S, et al. Stability and changes in metabolically healthy overweight or obesity and risk of future diabetes: Niigata wellness study. Obesity (Silver Spring). 2014;22(11):2420–5.
Jung CH et al. Association of metabolically healthy obesity with subclinical coronary atherosclerosis in a Korean population. Obesity (Silver Spring). 2014;22(12):2613–20.
Twig G, Afek A, Derazne E, et al. Diabetes risk among overweight and obese metabolically healthy young adults. Diabetes Care. 2014;37(11):2989–95.
Meigs JB, Wilson PWF, Fox CS, et al. Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. J Clin Endocrinol Metab. 2006;91(8):2906–12.
Arnlov J, Sundstrom J, Ingelsson E, et al. Impact of BMI and the metabolic syndrome on the risk of diabetes in middle-aged men. Diabetes Care. 2011;34(1):61–5.
Bo S, Musso G, Gambino R, et al. Prognostic implications for insulin-sensitive and insulin-resistant normal-weight and obese individuals from a population-based cohort. Am J Clin Nutr. 2012;96(5):962–9.
Soriguer F, Gutiérrez-Repiso C, Rubio-Martín E, et al. Metabolically healthy but obese, a matter of time? Findings from the prospective Pizarra study. J Clin Endocrinol Metab. 2013;98(6):2318–25.
Aung K, Lorenzo C, Hinojosa MA, et al. Risk of developing diabetes and cardiovascular disease in metabolically unhealthy normal-weight and metabolically healthy obese individuals. J Clin Endocrinol Metab. 2014;99(2):462–8.
Bell JA, Kivimaki M, Hamer M. Metabolically healthy obesity and risk of incident type 2 diabetes: a meta-analysis of prospective cohort studies. Obes Rev. 2014;15(6):504–15.
Hamer M, Stamatakis E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol Metab. 2012;97(7):2482–8.
Consultation, W.H.O.E. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63.
Williams B et al. ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953–2041.
Expert Committee on the, D. and M. Classification of Diabetes. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26(Suppl 1):S5–20.
Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Phillips DI et al. Understanding oral glucose tolerance: comparison of glucose or insulin measurements during the oral glucose tolerance test with specific measurements of insulin resistance and insulin secretion. Diabet Med. 1994;11(3):286–92.
Tschritter O, Fritsche A, Shirkavand F, et al. Assessing the shape of the glucose curve during an oral glucose tolerance test. Diabetes Care. 2003;26(4):1026–33.
Kanauchi M, Kimura K, Kanauchi K, et al. Beta-cell function and insulin sensitivity contribute to the shape of plasma glucose curve during an oral glucose tolerance test in non-diabetic individuals. Int J Clin Pract. 2005;59(4):427–32.
Abdul-Ghani MA, Lyssenko V, Tuomi T, et al. The shape of plasma glucose concentration curve during OGTT predicts future risk of type 2 diabetes. Diabetes Metab Res Rev. 2010;26(4):280–6.
Trujillo-Arriaga HM, Roman-Ramos R. Fitting and evaluating the glucose curve during a quasi continuous sampled oral glucose tolerance test. Comput Biol Med. 2008;38(2):185–95.
Tura A, Morbiducci U, Sbrignadello S, et al. Shape of glucose, insulin, C-peptide curves during a 3-h oral glucose tolerance test: any relationship with the degree of glucose tolerance? Am J Physiol Regul Integr Comp Physiol. 2011;300(4):R941–8.
Stone NJ et al. ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2013;63(25 Pt B):2889–934.
Garvey WT et al. American association of clinical endocrinologists and american college of endocrinology consensus conference on obesity: building an evidence base for comprehensive action. Endocr Pract. 2014;20(9):956–76.
Elahi D. In praise of the hyperglycemic clamp. A method for assessment of beta-cell sensitivity and insulin resistance. Diabetes Care. 1996;19(3):278–86.
Pacini G, Mari A. Methods for clinical assessment of insulin sensitivity and beta-cell function. Best Pract Res Clin Endocrinol Metab. 2003;17(3):305–22.
Kim JY, Coletta DK, Mandarino LJ, et al. Glucose response curve and type 2 diabetes risk in Latino adolescents. Diabetes Care. 2012;35(9):1925–30.
Acknowledgments
The authors would like to thank all of the involved study investigators, staffs, clinicians, nurses, and technicians for dedicating their time and skills to the completion of this study.
Funding
This study was supported by National Key Technologies R&D Program (Grant No. 2015BAI13B09), Research Foundation of Beijing Friendship Hospital, Capital Medical University (Grant No. yyqdkt 2017-31), Wu Jieping Medical Foundation (Grant No. 320.2710.1813), and Beijing Municipal Administration of Hospitals Incubating Program (Grant No. PX2018001).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
Statement of Human and Animal Rights
This study was performed in accordance with the principles of the Declaration of Helsinki and was approved by the Ethics Committees of Beijing Friendship Hospital, Capital Medical University.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, M., Liu, Y., Jin, L. et al. Metabolic Features of Individuals with Obesity Referred for Bariatric and Metabolic Surgery: a Cohort Study. OBES SURG 29, 3966–3977 (2019). https://doi.org/10.1007/s11695-019-04067-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04067-0