Abstract
Aims
To compare non-fatal cardiovascular (CV) events and metabolic outcomes, among obese patients with insulin-treated type 2 diabetes who underwent bariatric surgery compared with a propensity-matched non-bariatric cohort.
Methods
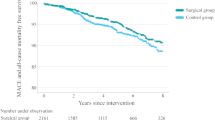
A retrospective cohort study was conducted among 11,125 active patients with type 2 diabetes from The Health Improvement Network (THIN) database. Propensity score matching (up to 1:6 ratio) was used to identify patients who underwent bariatric surgery (N = 131) with a non-bariatric cohort (N = 579). Follow-up was undertaken for 10 years (9686 person-years) to compare differences in metabolic outcomes and CV risk events that included the following: acute myocardial infarction (AMI), stroke, coronary heart disease (CHD), heart failure (HF) and peripheral artery disease (PAD). Cox proportional regression was used to compute the outcomes between groups.
Results
The mean age was 52 (SD 13) years (60% female); the baseline weight and BMI were 116 (SD 25) kg and 41 (SD 9) kg/m2, respectively. Significant reductions in weight and BMI were observed in bariatric group during 10 years of follow-up. Bariatric surgery had a significant cardioprotective effect by reducing the risk of non-fatal CHD (adjusted hazard ratio [aHR] 0.29, 95% CI 0.16–0.52, p < 0.001) and PAD events (aHR 0.31, 95% CI 0.11–0.89, p = 0.03). However, the surgery had no significant effect on AMI (aHR 0.98, p = 0.95), stroke (HR 0.87, p = 0.76) and HF (HR 0.89, p = 0.73) risks. Bariatric surgery had favourable effects on insulin independence, HbA1c and BP.
Conclusion
Among obese insulin-treated patients with type 2 diabetes, bariatric surgery is associated with significant reductions in non-fatal CHD and PAD events, lower body weight, HbA1c, BP and a greater likelihood of insulin independency during 10 years of follow-up.


Similar content being viewed by others
References
Finucane MM, Stevens GA, Cowan MJ, et al. Global burden of metabolic risk factors of chronic diseases collaborating group (body mass index) national, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557–67.
Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–78.
Bays HE. Adiposopathy is “sick fat” a cardiovascular disease? J Am Coll Cardiol. 2011;57:2461–73.
Vidal J. Updated review on the benefits of weight loss. Int J Obes Relat Metab Disord. 2002;26(Suppl 4):S25–8.
Dombrowski SU, Knittle K, Avenell A, et al. Long term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trials. BMJ. 2014;348:g2646.
Golzarand M, Toolabi K, Farid R. The bariatric surgery and weight losing: a meta-analysis in the long- and very long-term effects of laparoscopic adjustable gastric banding, laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy on weight loss in adults. Surg Endosc. 2017;31:4331–45.
Eliasson B, Liakopoulos V, Franzén S, et al. Cardiovascular disease and mortality in patients with type 2 diabetes after bariatric surgery in Sweden: a nationwide, matched, observational cohort study. Lancet Diabetes Endocrinol. 2015;3:847–54.
Romeo S, Maglio C, Burza MA, et al. Cardiovascular events after bariatric surgery in obese subjects with type 2 diabetes. Diabetes Care. 2012;35:2613–7.
Vest AR, Heneghan HM, Agarwal S, et al. Bariatric surgery and cardiovascular outcomes: a systematic review. Heart. 2012;98:1763–77.
Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–89.
Russell-Jones D, Khan R. Insulin-associated weight gain in diabetes – causes, effects and coping strategies. Diabetes Obes Metab. 2007;9(6):799–812.
Herman ME, O'Keefe JH, Bell DSH, et al. Insulin therapy increases cardiovascular risk in type 2 diabetes. Prog Cardiovasc Dis. 2017;60:422–34.
The Action to Control Cardiovascular risk in diabetes study Group. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545.
Holman RR, Sourij H, Califf RM. Cardiovascular outcome trials of glucose-lowering drugs or strategies in type 2 diabetes. Lancet. 2014;383(9933):2008–17.
Currie CJ, Poole CD, Evans M, et al. Mortality and other important diabetes-related outcomes with insulin vs other antihyperglycemic therapies in type 2 diabetes. J Clin Endocrinol Metab. 2013;98(2):668–77.
Roumie CL, Greevy RA, Grijalva CG, et al. Association between intensification of metformin treatment with insulin vs sulfonylureas and cardiovascular events and all-cause mortality among patients with diabetes. Jama. 2014;311(22):2288–96.
Muniyappa R, Iantorno M, Quon MJ. An integrated view of insulin resistance and endothelial dysfunction. Endocrinol Metab Clin N Am. 2008;37:685–711.
Van Avendonk MWJ, Rutten GEH. Insulin therapy in type 2 diabetes: what is the evidence? Diabetes Obes Metab. 2009;11(5):415–32.
The Heath Improvement Network (THIN).15 Nov 2018. Available from: https://www.iqvia.com/locations/uk-and-ireland/thin. Accessed 15 Nov 2018
Garrido MM, Kelley AS, Paris J, et al. Methods for constructing and assessing propensity scores. Health Serv Res. 2014;49:1701–20.
Rassen JA, Shelat AA, Myers J, et al. One-to-many propensity score matching in cohort studies. Pharmacoepidemiol Drug Saf. 2012;21(S2):69–80.
Austin PC. Statistical criteria for selecting the optimal number of untreated subjects matched to each treated subject when using many-to-one matching on the propensity score. Am J Epidemiol. 2010;172:1092–7.
Morris TP, White IR, Royston P. Tuning multiple imputation by predictive mean matching and local residual draws. BMC Med Res Methodol. 2014;14:75.
Eulenburg C, Suling A, Neuser P, et al. Propensity scoring after multiple imputation in a retrospective study on adjuvant radiation therapy in lymph-node positive vulvar Cancer. PLoS One. 2016;11:e0165705.
Dhalwani NN, Zaccardi F, Waheed H, et al. Cardiovascular, cancer and mortality events after bariatric surgery in people with and without pre-existing diabetes: a nationwide study. J Diabetes. 2018. https://doi.org/10.1111/1753-0407.12851.
Huang Y, Xu M, Xie L, et al. Obesity and peripheral arterial disease: a Mendelian randomization analysis. Atherosclerosis. 2016;247:218–24.
Ekelund M, Filipsson K, Tengmark BO, et al. Liraglutide in people treated for type 2 diabetes with multiple daily insulin injections: randomised clinical trial (MDI Liraglutide trial). BMJ. 2015;351:h5364. https://doi.org/10.1136/bmj.h5364.
Mathieu C, Rodbard HW, Cariou B, et al. A comparison of adding liraglutide versus a single daily dose of insulin aspart to insulin degludec in subjects with type 2 diabetes (BEGIN: VICTOZA ADD-ON). Diabetes Obes Metab. 2014;16:636–44.
Anyanwagu U, Mamza J, Donnelly R, et al. Effect of adding GLP-1RA on mortality, cardiovascular events, and metabolic outcomes among insulin-treated patients with type 2 diabetes: a large retrospective UK cohort study. Am Heart J. 2018;196:18–27.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes–3-year outcomes. N Engl J Med. 2014;370:2002–13.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, singlecentre, randomised controlled trial. Lancet. 2015;386:964–73.
Ikramuddin S, Korner J, Lee W-J, et al. Rouxen-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA. 2013;309:2240–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval was provided by the NHS South East Multi-centre Research Ethics Committee (MREC).
Conflicts of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
What is already known about this subject?
- Obesity and type 2 diabetes are associated with a high risk of cardiovascular events.
- Obesity is causally associated with peripheral artery disease.
- Insulin-treated type 2 diabetes is associated with additional excess risk of cardiovascular events.
- Bariatric surgery in people with or without diabetes reduces cardiovascular events.
What does this study add?
- This study focuses on insulin-treated type 2 diabetes—recently recognised to be associated with higher risks of cardiovascular events.
- Among insulin-treated type 2 diabetes, bariatric surgery is associated with a significant reduction in non-fatal coronary heart disease and peripheral artery disease.
- Among insulin-treated type 2 diabetes, bariatric surgery is associated with significant reduction and maintenance of weight loss, a significant reduction in HbA1c, with relapse of HbA1c levels after 6 years of follow-up and with increased likelyhood of insulin independency.
How might this impact on clinical practice?
- Bariatric surgery should be considered as a genuine therapeutic option for the management of obese insulin-treated type 2 diabetes to reduce risk of coronary heart disease, and peripheral artery disease, reduce HbA1c levels and potentially reduce the long-term risk of microvascular complications of diabetes as well as inducing insulin independence.
Electronic supplementary material
ESM 1
(DOCX 687 kb)
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Alkharaiji, M., Anyanwagu, U., Donnelly, R. et al. Effect of Bariatric Surgery on Cardiovascular Events and Metabolic Outcomes in Obese Patients with Insulin-Treated Type 2 Diabetes: a Retrospective Cohort Study. OBES SURG 29, 3154–3164 (2019). https://doi.org/10.1007/s11695-019-03809-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03809-4