Abstract
Background
Laparoscopic Roux-en-Y gastric bypass (LRYGB) surgery is a safe and effective procedure for patients with severe obesity. One potential complication of LRYGB is the development of marginal ulcers (MUs). Nonsteroidal anti-inflammatory drugs (NSAIDs) are known to significantly increase the likelihood of developing marginal ulcers after surgery. However, the risk associated with low-dose aspirin consumption is not well defined. We examined the impact of daily low-dose aspirin (81 mg) on the development of marginal ulcers following LRYGB.
Methods
A retrospective cohort design studied patients undergoing LRYGB surgery, between January 2009 and January 2013, at a single, high-volume bariatric center in Ontario, Canada. The marginal ulcer rate of patients taking low-dose aspirin after surgery was compared to that of the control patients who did not take any NSAID. Diagnosis of MU was confirmed by upper endoscopy in patients presenting with symptoms and a history indicative of marginal ulceration. A chi-square test of independence was performed to examine the difference in marginal ulcer rates.
Results
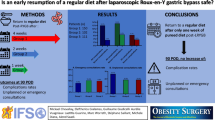
A total of 1016 patients underwent LRYGB. Patients taking aspirin were more likely to be male, older, and have diabetes than patients not taking NSAIDs. Of the 1016 patients, 145 (14.3%) took low-dose aspirin following LRYGB and the rest did not (n = 871, 85.7%). The incidence of marginal ulceration was not significantly different between the two treatment groups (12/145, 8.3% versus 90/871, 10.3%; p = 0.45).
Conclusions
Patients treated with LRYGB at our institution were not at increased risk of marginal ulcer formation when taking low-dose aspirin after surgery.


Similar content being viewed by others
References
Sapala JA, Wood MH, Sapala MA, et al. Marginal ulcer after gastric bypass: a prospective 3-year study of 173 patients. Obes Surg. 1998;8:505–16.
MacLean LD, Rhode BM, Nohr C, et al. Stomal ulcer after gastric bypass. J Am Coll Surg. 1997;185(1):1–7.
Dallal RM, Bailey LA. Ulcer disease after gastric bypass surgery. Surg Obes Relat Dis. 2006;2:455–9.
Gumbs AA, Duffy AJ, Bell R. Incidence and management of marginal ulceration after laparoscopic Roux-Y gastric bypass. Surg Obes Relat Dis. 2006;2(4):460–3.
Coblijn UK, Goucham AB, Lagarde SM, et al. Development of ulcer disease after Roux-en-Y gastric bypass, incidence, risk factors, and patient presentation: a systematic review. Obes Surg. 2014;24:299–309.
Ying VWC, Kim SHH, Khan KJ, et al. Prophylactic PPI help reduce marginal ulcers after gastric bypass surgery: a systematic review and meta-analysis of cohort studies. Surg Endosc. 2014;29:1018–23.
Wilson JA, Romagnuolo J, Byrne TK, et al. Predictors of endoscopic findings after Roux-en-Y gastric bypass. Am J Gastroenterol. 2006;101(10):2194–9.
Vandvik PO, Lincoff AM, Gore JM, et al. Primary and secondary prevention of cardiovascular disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e637s.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update. Surg Obe Relat Dis. 2013;9:159–91.
Gastrointestinal surgery for severe obesity. Consensus development conference panel, National Institutes of Health. NIH publication 2011; No 08–4006.
Higa KD, Boone KB, Ho T. Complications of the laparoscopic Roux-en-Y gastric bypass: 1,040 patients: what have we learned? Obes Surg. 2000;6:509–13.
Sverden E, Mattsson F, Sonden A et al. Risk factors for marginal ulcer after gastric bypass surgery for obesity. Annals of Surgery 2015; Nov 00:1–5.
Azagury DE, Dayyeh BK, Greenwalt LT, et al. Marginal ulceration after Roux-en-Y gastric bypass surgery: characteristics, risk factors, treatment, and outcomes. Endoscopy. 2011;43:950–4.
Acknowledgements
The authors thank Liam Crummey and Susan Haley from McMaster University for their data management assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Institutional review board approval for this study was obtained from the Hamilton Integrated Research Ethics Board.
Conflict of Interest
The authors declare they have no conflict of interest.
A Statement of Informed Consent (When Reporting Studies that Involve Human Participants)
Informed consent was not required to be obtained for this retrospective study.
A Statement of Human and Animal Rights
This study has been approved by the appropriate institutional review board.
Grant Support
None.
Rights and permissions
About this article
Cite this article
Kang, X., Hong, D., Anvari, M. et al. Is Daily Low-Dose Aspirin Safe to Take Following Laparoscopic Roux-en-Y Gastric Bypass for Obesity Surgery?. OBES SURG 27, 1261–1265 (2017). https://doi.org/10.1007/s11695-016-2462-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2462-z