Abstract
Background
Uncontrolled studies looking at the discontinuation of obstructive sleep apnea (OSA) treatment after bariatric surgery (BS) have suggested that surgery improves OSA. However, this discontinuation of OSA treatment by BS patients has never been compared to a matched population without BS. The objectives of this study are to evaluate whether BS increases OSA treatment discontinuation compared to that in matched patients without BS and to identify predictive factors of OSA treatment discontinuation in BS patients. The study took place in an ambulatory, tertiary hospital.
Methods
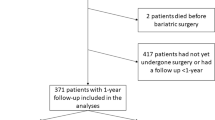
We included 61 OSA patients who underwent BS in a retrospective controlled cohort study. The computerized matching procedure included age, sex, body mass index, year of starting OSA treatment, treatment type, and duration selected 59 controls matched to 28 patients with BS. The main outcome was OSA treatment discontinuation within 2 years after BS.
Results
Patients with BS stopped OSA treatment more often than controls, usually between 6 months and 1 year after BS: hazards ratio (HR (95 %, CI)) 15.93 (3.29, 77.00). Before 6 months or beyond 1 year after BS, treatment discontinuation was not different between BS patients and controls. In univariate analyses, female gender, absence of co-morbidities, greater weight loss, and lower baseline OSA severity were associated with stopping OSA treatment after BS. No factor remained independently associated in multivariate analysis.
Conclusions
Apneic patients having BS stop OSA treatment more than matched controls. Treatment discontinuation may be attributed to recovery or to abandonment. The effect of BS on OSA may have been overestimated in uncontrolled BS studies that ignored basal OSA treatment discontinuation in routine clinical practice.


Similar content being viewed by others
References
Young T, Peppard PE, Taheri S. Excess weight and sleep-disordered breathing. J Appl Physiol. 2005;99:1592–9.
Peppard PE, Young T, Palta M, et al. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000;284:3015–21.
Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:136–43.
Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet. 2014;383:736–47.
Baguet JP, Barone-Rochette G, Tamisier R, Levy P, Pepin JL. Mechanisms of cardiac dysfunction in obstructive sleep apnea. Nat Rev Cardiol. 2012.
Pepin JL, Tamisier R, Levy P. Obstructive sleep apnoea and metabolic syndrome: put CPAP efficacy in a more realistic perspective. Thorax. 2012;67:1025–7.
Meurice JC, Dore P, Paquereau J, et al. Predictive factors of long-term compliance with nasal continuous positive airway pressure treatment in sleep apnea syndrome. Chest. 1994;105:429–33.
Kribbs NB, Pack AI, Kline LR, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis. 1993;147:887–95.
Furukawa T, Suzuki M, Ochiai M, et al. Long-term adherence to nasal continuous positive airway pressure therapy by hypertensive patients with preexisting sleep apnea. J Cardiol. 2014;63:281–5.
Pepin JL, Krieger J, Rodenstein D, et al. Effective compliance during the first 3 months of continuous positive airway pressure. A European prospective study of 121 patients. Am J Respir Crit Care Med. 1999;160:1124–9.
Carneiro G, Florio RT, Zanella MT, et al. Is mandatory screening for obstructive sleep apnea with polysomnography in all severely obese patients indicated? Sleep Breath. 2012;16:163–8.
Khan A, King WC, Patterson EJ, et al. Assessment of obstructive sleep apnea in adults undergoing bariatric surgery in the longitudinal assessment of bariatric surgery-2 (LABS-2) study. J Clin Sleep Med. 2013;9:21–9.
Rao A, Tey BH, Ramalingam G, et al. Obstructive sleep apnoea (OSA) patterns in bariatric surgical practice and response of OSA to weight loss after laparoscopic adjustable gastric banding (LAGB). Ann Acad Med Singap. 2009;38:587–7.
Rasmussen JJ, Fuller WD, Ali MR. Sleep apnea syndrome is significantly underdiagnosed in bariatric surgical patients. Surg Obes Relat Dis. 2012;8:569–73.
Ravesloot MJ, van Maanen JP, Hilgevoord AA, et al. Obstructive sleep apnea is underrecognized and underdiagnosed in patients undergoing bariatric surgery. Eur Arch Otorhinolaryngol. 2012;269:1865–71.
Lopes Neto JM, Brandao LO, Loli A, et al. Evaluation of obstructive sleep apnea in obese patients scheduled for bariactric surgery. Acta Cir Bras. 2013;28:317–22.
Karason K, Lindroos AK, Stenlof K, et al. Relief of cardiorespiratory symptoms and increased physical activity after surgically induced weight loss: results from the Swedish Obese Subjects study. Arch Intern Med. 2000;160:1797–802.
Romero-Corral A, Caples SM, Lopez-Jimenez F, et al. Interactions between obesity and obstructive sleep apnea: implications for treatment. Chest. 2010;137:711–9.
Schachter L. Respiratory assessment and management in bariatric surgery. Respirology. 2012;17:1039–47.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Sarkhosh K, Switzer NJ, El-Hadi M, et al. The impact of bariatric surgery on obstructive sleep apnea: a systematic review. Obes Surg. 2013;23:414–23.
Greenburg DL, Lettieri CJ, Eliasson AH. Effects of surgical weight loss on measures of obstructive sleep apnea: a meta-analysis. Am J Med. 2009;122:535–42.
Ashrafian H, le Roux CW, Rowland SP, et al. Metabolic surgery and obstructive sleep apnoea: the protective effects of bariatric procedures. Thorax. 2012;67:442–9.
Borel JC, Tamisier R, Dias-Domingos S, et al. Type of mask may impact on continuous positive airway pressure adherence in apneic patients. PLoS One. 2013;8:e64382.
Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5:173–8.
Gagnadoux F, Le Vaillant M, Goupil F, et al. Influence of marital status and employment status on long-term adherence with continuous positive airway pressure in sleep apnea patients. PLoS One. 2011;6, e22503.
Wozniak DR, Lasserson TJ, Smith I. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev. 2014;1:CD007736.
Collen J, Lettieri CJ, Eliasson A. Postoperative CPAP use impacts long-term weight loss following bariatric surgery. J Clin Sleep Med. 2015;11:213–7.
Alfa Wali M, Ashrafian H, Schofield KL, Harling L, Alkandari A, Darzi A et al. Is social deprivation associated with weight loss outcomes following bariatric surgery? A 10-year single institutional experience. Obes Surg. 2014;24:2126–32.
Kennedy-Dalby A, Adam S, Ammori BJ, et al. Weight loss and metabolic outcomes of bariatric surgery in men versus women—a matched comparative observational cohort study. Eur J Intern Med. 2014;25:922–5.
Acknowledgments
We thank Nathalie Arnol who performed statistical analyses, Matthieu Lesgoirres who was involved in collecting retrospective data and Dr. Alison Foote (Grenoble Clinical Research Center) for critically reading and editing the manuscript with respect to English language.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Grants
“Fonds Agir pour les maladies chroniques”
Funding
The present study was supported by “Fond Agir pour les maladies chroniques.”
Disclosure Summary
CA: has no relevant conflict of interest to disclose
JCB: is employed by “Agiràdom”, a non-profit home care provider
FR: has nothing to declare regarding this study.
CA: has nothing to declare regarding this study.
NW: has nothing to declare regarding this study.
SJ: has nothing to declare regarding this study.
DJ: has nothing to declare regarding this study.
JLP: has nothing to declare regarding this study.
ALB: received grant support from “Agiràdom”, a non-profit home care provider in 2009, 2011, 2012, 2013 and 2014
According to French law, this database study using data from routine clinical practice records, did not require informed consent. The study was approved by the institutional ethics committee and has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Agosta, C., Borel, JC., Reche, F. et al. Treatment Discontinuation Following Bariatric Surgery in Obstructive Sleep Apnea: a Controlled Cohort Study. OBES SURG 26, 2082–2088 (2016). https://doi.org/10.1007/s11695-016-2048-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2048-9