Abstract
Background
Smoking cessation had been typically associated with weight gain. So far, there are no reports documenting the relationship between weight loss after bariatric surgery and smoking habit. The objective of the study was to establish the relationship between weight loss and smoking habit in patients undergoing bariatric surgery and to analyze weight loss on severe smokers and on those patients who stopped smoking during the postoperative period.
Methods
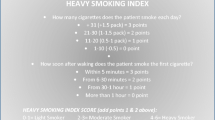
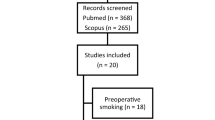
All patients undergoing laparoscopic sleeve gastrectomy (LSG) with at least 2-year follow-up were included. Patients were divided into three groups: (A) smokers, (B) ex-smokers, and (C) non-smokers. Demographics and weight loss at 6, 12, and 24 months were analyzed. Smokers were subdivided for further analysis into the following: group A1: heavy smokers, group A2: non-heavy smokers, group A3: active smokers after surgery, and group A4: quitters after surgery. Chi-square test was used for statistics.
Results
One hundred eighty-four patients were included; group A: 62 patients, group B: 57 patients, and group C: 65 patients. Mean BMI was 34 ± 6, 31 ± 6, and 31 ± 6 kg/m2; mean %EWL was 63 ± 18, 76 ± 21, and 74 ± 22 % at 6, 12, and 24 months, respectively. The subgroup analysis showed the following composition: group A1: 19 patients, group A2: 43 patients, group A3: 42 patients, and group A4: 20 patients. Weight loss difference among groups and subgroups was statistically non-significant.
Conclusions
Our study shows that weight loss evolution was independent from smoking habit. Neither smoking cessation during the postoperative period nor smoking severity could be related to weight loss after LSG.



Similar content being viewed by others
References
de Sereday MS, Gonzalez C, Giorgini D, et al. Prevalence of diabetes, obesity, hypertension and hyperlipidemia in the central area of Argentina. Diabetes Metab. 2004;30(4):335–9.
Vishwa Deep D. Adipose-immune interactions during obesity and caloric restriction: reciprocal mechanisms regulating immunity and health span. J Leukoc Biol. 2008;84(4):882–92.
Dan E, Anna B, Nina B. Sleeve gastrectomy as a stand-alone bariatric operation for severe, morbid, and super obesity. Health Technol Assess. 2009;13(41):1–190. 215–357, iii-iv.
Picot J, Jones J, Colquitt JL, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13(41):1–190.
Livhits M, Mercado C, Yermilov I, et al. Preoperative predictors of weight loss following bariatric surgery: systematic review. Obes Surg. 2012;22(1):70–89. doi:10.1007/s11695-011-0472-4.
6) Trastulli S, Desiderio J, Guarino S, Cirocchi R, Scalercio V, Noya G, Parisi A. Laparoscopic sleeve gastrectomy compared with other bariatric surgical procedures: a systematic review of randomized trials. Surg Obes Relat Dis. 2013 Jun 12.
Terra X, Auguet T, Guiu-Jurado E, et al. Long-term changes in leptin, chemerin and ghrelin levels following different bariatric surgery procedures: Roux-en-Y gastric bypass and sleeve gastrectomy. Obes Surg. 2013;23(11):1790–8.
Yousseif A, Emmanuel J, Karra E, et al. Differential effects of laparoscopic sleeve gastrectomy and laparoscopic gastric bypass on appetite, circulating acyl-ghrelin, peptide YY3-36 and active GLP-1 levels in non-diabetic humans. Obes Surg. 2013;24(2):241–52.
Chabrol H, Niezborala M, Chastan E, et al. Comparison of the heavy smoking index and of the Fagerstrom test for nicotine dependence in a sample of 749 cigarette smokers. Addict Behav. 2005;30:1474–7.
Kazdin AE. Symptom substitution, generalization, and response covariation: implications for psychotherapy outcome. Psychol Bull. 1982;91(2):349–65.
Ferguson S, Al-Rehany L, Tang C, et al. Self-reported causes of weight gain: among prebariatric surgery patients. Can J Diet Pract Res. 2013;74(4):189–92.
Arterburn D, Livingston EH, Olsen MK, et al. Predictors of initial weight loss after gastric bypass surgery in twelve Veterans Affairs Medical Centers. Obes Res Clin Pract. 2013;7(5):e367–76.
Heinberg LJ, Ashton K. History of substance abuse relates to improved postbariatric body mass index outcomes. Surg Obes Relat Dis. 2010;6(4):417–21.
Lent MR, Hayes SM, Wood GC, et al. Smoking and alcohol use in gastric bypass patients. Eat Behav. 2013;14(4):460–3.
Lores Obradors L, Monsó Molas E, Rosell Gratacós A, et al. Do patients lie about smoking during follow-up in the respiratory medicine clinic? Arch Bronconeumol. 1999;35(5):219–22.
Conason A, Teixeira J, Hsu CH, et al. Substance use following bariatric weight loss surgery. JAMA Surg. 2013;148(2):145–50.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
For this type of study, formal consent is not required.
Conflict of Interest
The authors declare that they have no competing interests.
Informed Consent
Does not apply.
Rights and permissions
About this article
Cite this article
Moser, F., Signorini, F.J., Maldonado, P.S. et al. Relationship Between Tobacco Use and Weight Loss After Bariatric Surgery. OBES SURG 26, 1777–1781 (2016). https://doi.org/10.1007/s11695-015-2000-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-2000-4