Abstract
Background
The presence of disturbed eating patterns can affect the short- and long-term outcomes after bariatric surgery. Data about the influence of preoperative eating patterns on outcomes after biliopancreatic diversion (BPD) are lacking. The aim of the present study was to assess the role of preoperative eating behavior in patients’ selection for biliopancreatic diversion.
Methods
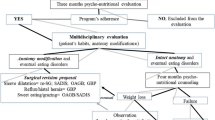
Sixty-one consecutive patients who underwent BPD were evaluated for the present study. For each patient, the following preoperative eating patterns were evaluated: sweet eating, snacking, hyperphagia, and gorging. The primary outcome measure was the percentage of excess weight loss (%EWL) at 3, 6, and 12 months in the groups of patients with different eating patterns at the preoperative evaluation.
Results
At the preoperative evaluation, snacking was found in 31 patients (50.8 %), sweet eating in 15 patients (24.6 %), hyperphagia in 48 patients (78.7 %), and gorging in 45 patients (73.8 %). For each eating behavior, there was no significant difference in mean preoperative BMI and weight loss at 3, 6, and 12 months between the group of patients with and the group of patients without the eating pattern considered. At the analysis of variance in the four groups of patients presenting the eating patterns considered, there was no difference in mean preoperative BMI (P = 0.66), %EWL at 3 months (P = 0.62), %EWL at 6 months (P = 0.94), and %EWL at 12 months (P = 0.95).
Conclusions
Preoperative eating behaviors do not represent reliable outcome predictors for BPD, and they should not be used as a selection criterion for patients who are candidates to this operation.
Similar content being viewed by others
References
Flegal KM. Epidemiologic aspects of overweight and obesity in the United States. Physiol Behav. 2005;86(5):599–602.
Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Ayyad C, Andersen T. Long-term efficacy of dietary treatment of obesity: a systematic review of studies published between 1931 and 1999. Obes Rev. 2000;1(2):113–9.
Herpertz S, Kielmann R, Wolf AM, et al. Do psychosocial variables predict weight loss or mental health after obesity surgery? A systematic review. Obes Res. 2004;12(10):1554–69.
Chevallier JM, Paita M, Rodde-Dunet MH, et al. Predictive factors of outcome after gastric banding: a nationwide survey on the role of center activity and patients’ behavior. Ann Surg. 2007;246(6):1034–9.
Msika S, Castel B. Present indications for surgical treatment of morbid obesity: how to choose the best operation? J Visc Surg. 2010;147(5 Suppl):e47–51.
Burgmer R, Grigutsch K, Zipfel S, et al. The influence of eating behavior and eating pathology on weight loss after gastric restriction operations. Obes Surg. 2005;15(5):684–91.
Busetto L, Valente P, Pisent C, et al. Eating pattern in the first year following adjustable silicone gastric banding (ASGB) for morbid obesity. Int J Obes Relat Metab Disord. 1996;20(6):539–46.
Hudson SM, Dixon JB, O'Brien PE. Sweet eating is not a predictor of outcome after Lap-Band placement. Can we finally bury the myth? Obes Surg. 2002;12(6):789–94.
Lindroos AK, Lissner L, Sjostrom L. Weight change in relation to intake of sugar and sweet foods before and after weight reducing gastric surgery. Int J Obes Relat Metab Disord. 1996;20(7):634–43.
Sugerman HJ, Londrey GL, Kellum JM, et al. Weight loss with vertical banded gastroplasty and Roux-Y gastric bypass for morbid obesity with selective versus random assignment. Am J Surg. 1989;157(1):93–102.
Sugerman HJ, Starkey JV, Birkenhauer R. A randomized prospective trial of gastric bypass versus vertical banded gastroplasty for morbid obesity and their effects on sweets versus non-sweets eaters. Ann Surg. 1987;205(6):613–24.
Cornicelli M, Noli G, Marinari GM, et al. Dietary habits and body weight at long-term following biliopancreatic diversion. Obes Surg. 2010;20(9):1278–80.
Rowston W, McCluskey S, Gazet JC, et al. Eating behavior, physical symptoms and psychological factors associated with weight reduction following the Scopinaro operation as modified by Gazet. Obes Surg. 1992;2(4):355–60.
Scopinaro N, Adami GF, Marinari GM, et al. Biliopancreatic diversion. World J Surg. 1998;22(9):936–46.
Greenberg I, Sogg S, Perna FM. Behavioral and psychological care in weight loss surgery: best practice update. Obesity (Silver Spring). 2009;17(5):880–4.
Conference NIH. Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med. 1991;115(12):956–61.
Bray GA. Lipogenesis in human adipose tissue: some effects of nibbling and gorging. J Clin Invest. 1972;51(3):537–48.
Scopinaro N. Thirty-five years of biliopancreatic diversion: notes on gastrointestinal physiology to complete the published information useful for a better understanding and clinical use of the operation. Obes Surg. 2012;22(3):427–32.
Kinzl JF, Schrattenecker M, Traweger C, et al. Psychosocial predictors of weight loss after bariatric surgery. Obes Surg. 2006;16(12):1609–14.
Scopinaro N, Gianetta E, Civalleri D, et al. Bilio-pancreatic bypass for obesity: II. Initial experience in man Br J Surg. 1979;66(9):618–20.
Scopinaro N, Gianetta E, Civalleri D, et al. Bilio-pancreatic bypass for obesity: 1. An experimental study in dogs Br J Surg. 1979;66(9):613–7.
West JA, de Looy AE. Weight loss in overweight subjects following low-sucrose or sucrose-containing diets. Int J Obes Relat Metab Disord. 2001;25(8):1122–8.
Heitmann BL, Lissner L. Dietary underreporting by obese individuals—is it specific or non-specific? BMJ. 1995;311(7011):986–9.
Hill RJ, Davies PS. The validity of self-reported energy intake as determined using the doubly labelled water technique. Br J Nutr. 2001;85(4):415–30.
Conflict of Interest
The authors declare that they have no proprietary, financial, professional, or other personal interest of any nature or kind in any product or service that may influence the position presented.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Facchiano, E., Scaringi, S., Quartararo, G. et al. Do Preoperative Eating Behaviors Influence Weight Loss After Biliopancreatic Diversion?. OBES SURG 23, 2080–2085 (2013). https://doi.org/10.1007/s11695-013-0940-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-013-0940-0