Abstract
Background
Our group has reported a high incidence of reactive hypoglycemia following Roux-en-Y gastric bypass (RYGB) with specific interest in postprandial insulin and the ratio of 1- to 2-h serum glucose levels. The purpose of this study is to compare the 6-month response to oral glucose challenge in patients undergoing RYGB, duodenal switch (DS), and vertical sleeve gastrectomy (VSG).
Methods
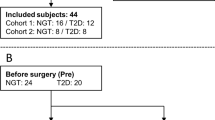
Thirty-eight patients meeting the NIH criteria for bariatric surgery who have reached the 6-month postoperative mark are the basis of this report. Preoperatively and at 6 months follow-up, patients underwent blood draw to determine levels of fasting glucose, fasting insulin, HbA1c, C peptide, and 2 h oral liquid glucose challenge test (OGTT). HOMA-IR and 1 to 2 h ratios of glucose and fasting to 1 h ratio of insulin were calculated.
Results
All patients underwent a successful laparoscopic bariatric procedure (VSG =13, DS =13, and RYGB = 12). All operations reduced BMI, HgbA1c, fasting glucose, and fasting insulin. HOMA IR and glucose tolerance improved with all procedures. In response to OGTT at 6 months, there was a 20-fold increase in insulin at 1 h in RYGB, which was not seen in DS. At 6 months, 1-h insulin was markedly lower in DS (p < .05), yet HbA1C was also lower in DS (p < .05). This resulted in 1- to 2-h glucose ratio of 1.9 for RYGB, 1.8 for VSG, and 1.3 for DS (p < .05).
Conclusions
All operations improve insulin sensitivity and decrease HgbA1c. Six-month weight loss was substantial in all groups between 22–29% excess body weight. RYGB results in marked rise in glucose following challenge with corresponding rise in 1-h insulin. VSG has a similar response to RYGB. In comparison, at 6 months following surgery, DS causes a much lower rise in 1-h insulin, with this difference being statistically significant at p < .05. As a result, DS results in a less abrupt reduction in blood glucose. Although 1-h insulin is lower, DS patients had the lowest HbA1C at 6 months (p < .05). We believe that these findings have important implications for the choice of bariatric procedure for both diabetic and non-diabetic patients.



Similar content being viewed by others
References
Cummings DE, Shannon MH. Roles for ghrelin in the regulation of appetite and body weight. Arch Surg. 2003;138:389–96.
Stylopoulos N, Hoppin AG, Kaplan LM. Roux-en-Y gastric bypass enhances energy expenditure and extends lifespan in diet-induced obese rats. Obesity (Silver Spring). 2009;17:1839–47.
Roslin M, Damani T, Oren J, et al. Abnormal glucose tolerance testing following gastric bypass demonstrates reactive hypoglycemia. Surg Endosc. 2010;25:1926–32.
Goldfine AB, Mun EC, Devine E, et al. Patients with neuroglycopenia after gastric bypass surgery have exaggerated incretin and insulin secretory responses to a mixed meal. J Clin Endocrinol Metab. 2007;92:4678–85.
Patti ME, McMahon G, Mun EC, et al. Severe hypoglycaemia post-gastric bypass requiring partial pancreatectomy: evidence for inappropriate insulin secretion and pancreatic islet hyperplasia. Diabetologia. 2005;48:2236–40.
Service GJ, Thompson GB, Service FJ, Andrews JC, Collazo-Clavell ML, Lloyd RV. Hyperinsulinemic hypoglycemia with nesidioblastosis after gastric-bypass surgery. N Engl J Med. 2005;353:249–54.
Clancy TE, Moore Jr FD, Zinner MJ. Post-gastric bypass hyperinsulinism with nesidioblastosis: subtotal or total pancreatectomy may be needed to prevent recurrent hypoglycemia. J Gastrointest Surg. 2006;10:1116–9.
Geloneze B, Geloneze SR, Fiori C, et al. Surgery for nonobese type 2 diabetic patients: an interventional study with duodenal–jejunal exclusion. Obes Surg. 2009;19:1077–83.
Ramos AC, Galvao Neto MP, de Souza YM, et al. Laparoscopic duodenal–jejunal exclusion in the treatment of type 2 diabetes mellitus in patients with BMI<30 kg/m2 (LBMI). Obes Surg. 2009;19:307–12.
Abbatini F, Rizzello M, Casella G, et al. Long-term effects of laparoscopic sleeve gastrectomy, gastric bypass, and adjustable gastric banding on type 2 diabetes. Surg Endosc. 2010;24:1005–10.
Woelnerhanssen B, Peterli R, Steinert RE, et al. Effects of postbariatric surgery weight loss on adipokines and metabolic parameters: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy—a prospective randomized trial. Surg Obes Relat Dis. 2011;7:561–8.
Johansson HE, Haenni A, Karlsson FA, et al. Biliopancreatic diversion with duodenal switch lowers both early and late phases of glucose, insulin and proinsulin response after meal. Obes Surg. 2010;20(5):549–58.
Buchwald H, Estok R, Fahrback K, et al. Weight and type 2 diabetes after bariatric surgery: systemic review and meta-analysis. Am J Med. 2009;122(3):248–56.
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366(17):1567–76.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366(17):1577–85.
Frenken M, Cho EY, Karcz, et al. Improvement of type 2 diabetes mellitus in obese and non-obese patients after the duodenal switch operation. J Obes. 2011;860–69.
Tsuchida T, Shiraishi M, Ohta T, et al. Ursodeoxycholic acid improves insulin sensitivity and hepatic steatosis by inducing the excretion of hepatic lipids in high-fat diet fed KK-A(y) mice. Metab. 2011.
Conflict of Interest
Dr. Roslin is on the SAB of ValenTX, Surgiquest, and Scientific Intake and consultant for J&J EES, Covidien. Research grant for this study is from Covidien. Patents are assigned to J&J and CR Bard. Dr. Dudiy has no conflict of interest. Joanne Weiskopf has no conflict of interest. Dr. Tanuja Damani has no conflict of interest. Dr. Shah is on SAB of Stryker and Transenterix and consultant for J&J EES and Olympus.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roslin, M.S., Dudiy, Y., Weiskopf, J. et al. Comparison Between RYGB, DS, and VSG Effect on Glucose Homeostasis. OBES SURG 22, 1281–1286 (2012). https://doi.org/10.1007/s11695-012-0686-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-012-0686-0