Abstract
Background
Obesity increases the risk of laparotomy dehiscence and incisional hernia. The aim of this study was to measure the biological effect of obesity on laparotomy wound healing and the formation of incisional hernias.
Methods
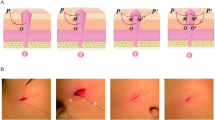
Normal-weight Sprague–Dawley (SD) and obese Zucker rats were used in an established laparotomy wound healing and incisional ventral hernia model. Mechanical testing was performed on abdominal wall strips collected from laparotomy wounds. Hernia size was measured by digital imaging. Picrosirius staining for collagen isoforms was observed with polarized microscopy. Abdominal wall fibroblasts were cultured to measure collagen matrix remodeling and proliferation.
Results
Laparotomy wound healing was significantly impaired in obese rats. Mechanical strength was lower than in normal-weight rats. Yield load was reduced in the obese group at all time points. Picrosirius red staining showed increased immature type III collagen content and disorganized type I collagen fibers within laparotomy wounds of obese rats. Wound size was significantly larger in the obese group. Collagen matrix remodeling was impaired with fibroblasts from obese rats, but there was no difference in fibroblast proliferation between the obese and normal-weight groups.
Conclusions
We observed for the first time that laparotomy wound healing is impaired in obese rats. The recovery of laparotomy wound strength is delayed due to abnormal collagen maturation and remodeling, possibly due to a defect in fibroblast function. Strategies to improve outcomes for laparotomy wound healing in obese patients should include correcting the wound healing defect, possibly with growth factor or cell therapy.





Similar content being viewed by others
References
Franz MG. The biology of hernia formation. Surg Clin North Am. 2008;88(1):1–15. vii.
Pollock AV, Evans M. Early prediction of late incisional hernias. Br J Surg. 1989;76:953–4.
Burger JW et al. Incisional hernia: early complication of abdominal surgery. World J Surg. 2005;29(12):1608–13.
Hoer J et al. Factors influencing the development of incisional hernia. A retrospective study of 2, 983 laparotomy patients over a period of 10 years. Chirurg. 2002;73(5):474–80.
Sugerman HJ et al. Greater risk of incisional hernia with morbidly obese than steroid-dependent patients and low recurrence with prefascial polypropylene mesh. Am J Surg. 1996;171(1):80–4.
Riou JP, Cohen JR, Johnson Jr H. Factors influencing wound dehiscence. Am J Surg. 1992;163(3):324–30.
Regnard JF et al. Ventral incisional hernias: incidence, date of recurrence, localization and risk factors. Ital J Surg Sci. 1988;18(3):259–65.
Merkow RP et al. Effect of body mass indes on short-term outcomes after colectomy for cancer. J Am Coll Surg. 2009;208:53–61.
Grace RH, Cox SJ. Incidence of incisional hernia following dehiscence of the abdominal wound. Proc R Soc Med. 1973;66(11):1091–2.
Keill RH et al. Abdominal wound dehiscence. Arch Surg. 1973;106(4):573–7.
Alexander HC, Prudden JF. The causes of abdominal wound disruption. Surg Gynecol Obstet. 1966;122(6):1223–9.
Baggish MS, Lee WK. Abdominal wound disruption. Obstet Gynecol. 1975;46(5):530–4.
Pitkin RM. Abdominal hysterectomy in obese women. Surg Gynecol Obstet. 1976;142(4):532–6.
Bucknall TE, Cox PJ, Ellis H. Burst abdomen and incisional hernia: a prospective study of 1129 major laparotomies. Br Med J (Clin Res Ed). 1982;284(6320):931–3.
Lamont PM, Ellis H. Incisional hernia in re-opened abdominal incisions: an overlooked risk factor. Br J Surg. 1988;75(4):374–6.
Kupczyk-Joeris D et al. Incisional hernia. Causes and principles of repair. Zentralbl Chir. 1990;115(18):1161–7.
Hesselink VJ et al. An evaluation of risk factors in incisional hernia recurrence. Surg Gynecol Obstet. 1993;176(3):228–34.
da Silva AL, Petroianu A. Incisional hernias: factors influencing development. South Med J. 1991;84(12):1500. 1504.
Cleveland RD, Zitsch 3rd RP, Laws HL. Incisional closure in morbidly obese patients. Am Surg. 1989;55(1):61–3.
Luijendijk RW et al. A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med. 2000;343(6):392–8.
Carlson MA. Acute wound failure. Surg Clin North Am. 1997;77(3):607–36.
Burger JW et al. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg. 2004;240(4):578–83.
Sauerland S et al. Obesity is a risk factor for recurrence after incisional hernia repair. Hernia. 2004;8(1):42–6.
Nascimento AP, Costa AM. Overweight induced by high-fat diet delays rat cutaneous wound healing. Br J Nutr. 2006;96(6):1069–77.
Goodson 3rd WH, Hunt TK. Wound collagen accumulation in obese hyperglycemic mice. Diabetes. 1986;35(4):491–5.
Biondo-Simoes Mde L, et al. Obesity and abdominal wound healing in rats. Acta Cir Bras. 25(1):86–92.
DuBay DA et al. Progressive fascial wound failure impairs subsequent abdominal wall repairs: a new animal model of incisional hernia formation. Surgery. 2005;137(4):463–71.
DuBay DA et al. Incisional herniation induces decreased abdominal wall compliance via oblique muscle atrophy and fibrosis. Ann Surg. 2007;245(1):140–6.
Franz MG et al. Fascial incisions heal faster than skin: a new model of abdominal wall repair. Surgery. 2001;129(2):203–8.
Puchtler H, Waldrop FS, Valentine LS. Polarization microscopic studies of connective tissue stained with picro-sirius red FBA. Beitr Pathol. 1973;150(2):174–87.
Junqueira LC et al. Differential histologic diagnosis of osteoid. A study on human osteosarcoma collagen by the histochemical picrosirius-polarization method. J Pathol. 1986;148(2):189–96.
Montes GS et al. Histochemical and morphological characterization of reticular fibers. Histochemistry. 1980;65(2):131–41.
Dubay DA et al. Fascial fibroblast kinetic activity is increased during abdominal wall repair compared to dermal fibroblasts. Wound Repair Regen. 2004;12(5):539–45.
Baum CL, Arpey CJ. Normal cutaneous wound healing: clinical correlation with cellular and molecular events. Dermatol Surg. 2005;31(6):674–86. discussion 686.
Goodson 3rd WH, Hunt TK. Deficient collagen formation by obese mice in a standard wound model. Am J Surg. 1979;138(5):692–4.
Vrabec JT. Tympanic membrane perforations in the diabetic rat: a model of impaired wound healing. Otolaryngol Head Neck Surg. 1998;118(3 Pt 1):304–8.
Kurtz TW, Morris RC, Pershadsingh HA. The Zucker fatty rat as a genetic model of obesity and hypertension. Hypertension. 1989;13(6 Pt 2):896–901.
Bray GA. The Zucker-fatty rat: a review. Fed Proc. 1977;36(2):148–53.
Metz CN. Fibrocytes: a unique cell population implicated in wound healing. Cell Mol Life Sci. 2003;60(7):1342–50.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
This project was supported by the Rapid Wound Healing Technology Development Project grant from the US Department of Defense and Stemnion, Inc.
Rights and permissions
About this article
Cite this article
Xing, L., Culbertson, E.J., Wen, Y. et al. Impaired Laparotomy Wound Healing in Obese Rats. OBES SURG 21, 1937–1946 (2011). https://doi.org/10.1007/s11695-011-0377-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-011-0377-2