Abstract
Background
Super-obesity (BMI > 50) is increasing rapidly. We use the biliopancreatic diversion with duodenal switch (BPD-DS) as one option in this patient category. The aim of the present study was to investigate the emptying of the gastric tube, PYY levels and dumping symptoms after BPD-DS.
Methods
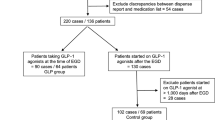
Emptying of the gastric tube was investigated with scintigraphy after an overnight fast. Twenty patients (median age 43 years, BMI 31.1 kg/m2) having undergone BPD-DS in median 3.5 years previously were included in the scintigraphic study. A technetium-labelled omelette was ingested and scintigraphic evaluation of gastric emptying was undertaken. Ten of the patients also underwent PYY measurements after a standardised meal and were compared to nine non-operated age-matched normal weight controls, both in the fasting state and after the test meal. Frequency of dumping symptoms was evaluated in all patients.
Results
The half-emptying time was 28 ± 16 min. Lag phase was present in 30% of the patients. PYY levels were significantly higher in BPD-DS patients as compared to controls both in the fasting state (p < 0.001) and after the test meal (p < 0.001). Dumping symptoms were scarce and occurred in 17 of the 20 patients only few times yearly or less.
Conclusions
Although the pylorus is preserved in BPD-DS, the stomach emptying is faster than in non-operated subjects. PYY levels are elevated in the fasting state after BPD-DS and a marked response to a test meal is seen, likely due to the rapid stimulation of intraluminal nutrients in the distal ileum. In spite of this, dumping symptoms are uncommon.




Similar content being viewed by others
References
Deitel M. Overweight and obesity worldwide now estimated to involve 1.7 billion people. Obes Surg. 2003;13:329–30.
Ogden CL, Yanovski SZ, Carroll MD, et al. The epidemiology of obesity. Gastroenterology. 2007;132:2087–102.
Olshansky SJ, Passaro DJ, Hershow RC, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352:1138–45.
Duval K, Marceau P, Lescelleur O, et al. Health-related quality of life in morbid obesity. Obes Surg. 2006;16:574–9.
Calle EE, Rodriguez C, Walker-Thurmond K, et al. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–38.
Field AE, Coakley EH, Must A, et al. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med. 2001;161:1581–6.
Must A, Spadano J, Coakley EH, et al. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–9.
Fontaine KR, Redden DT, Wang C, et al. Years of life lost due to obesity. JAMA. 2003;289:187–93.
Freedman DM, Ron E, Ballard-Barbash R, et al. Body mass index and all-cause mortality in a nationwide US cohort. Int J Obes (Lond). 2006;30:822–9.
Colquitt J, Clegg A, Loveman E, et al. Surgery for morbid obesity. Cochrane Database Syst Rev 2005:CD003641
Sundbom M, Karlson BM. Low mortality in bariatric surgery 1995 through 2005 in Sweden, in spite of a shift to more complex procedures. Obes Surg. 2009;19:1697–701.
MacLean LD, Rhode BM, Nohr CW. Late outcome of isolated gastric bypass. Ann Surg. 2000;231:524–8.
Hess DS, Hess DW. Biliopancreatic diversion with a duodenal switch. Obes Surg. 1998;8:267–82.
Marceau P, Hould FS, Simard S, et al. Biliopancreatic diversion with duodenal switch. World J Surg. 1998;22:947–54.
Hess DS, Hess DW, Oakley RS. The biliopancreatic diversion with the duodenal switch: results beyond 10 years. Obes Surg. 2005;15:408–16.
Scopinaro N, Gianetta E, Civalleri D, et al. Bilio-pancreatic bypass for obesity: II. Initial experience in man. Br J Surg. 1979;66:618–20.
Latarjet A. Section des rameaux gastriques du vague. Presse Méd. 1921;41:409.
McCrea ED. The abdominal distribution of the vagus. J Anat. 1924;59:18–40.
Holzer HH, Raybould HE. Vagal and splanchnic sensory pathways mediate inhibition of gastric motility induced by duodenal distension. Am J Physiol. 1992;262:G603–8.
Yung BC, Sostre S. Lag phase in solid gastric emptying: comparison of quantification by physiological and mathematical definitions. J Nucl Med. 1993;34:1701–5.
Collins PJ, Horowitz M, Cook DJ, et al. Gastric emptying in normal subjects—a reproducible technique using a single scintillation camera and computer system. Gut. 1983;24:1117–25.
Vazquez Roque MI, Camilleri M, Stephens DA, et al. Gastric sensorimotor functions and hormone profile in normal weight, overweight, and obese people. Gastroenterology. 2006;131:1717–24.
Braghetto I, Davanzo C, Korn O, et al. Scintigraphic evaluation of gastric emptying in obese patients submitted to sleeve gastrectomy compared to normal subjects. Obes Surg. 2009;19:1515–21.
Bernstine H, Tzioni-Yehoshua R, Groshar D, et al. Gastric emptying is not affected by sleeve gastrectomy—scintigraphic evaluation of gastric emptying after sleeve gastrectomy without removal of the gastric antrum. Obes Surg. 2009;19:293–8.
Michiura T, Nakane Y, Kanbara T, et al. Assessment of the preserved function of the remnant stomach in pylorus-preserving gastrectomy by gastric emptying scintigraphy. World J Surg. 2006;30:1277–83.
Nishikawa K, Kawahara H, Yumiba T, et al. Functional characteristics of the pylorus in patients undergoing pylorus—preserving gastrectomy for early gastric cancer. Surgery. 2002;131:613–24.
Lundberg JM, Tatemoto K, Terenius L, et al. Localization of peptide YY (PYY) in gastrointestinal endocrine cells and effects on intestinal blood flow and motility. Proc Natl Acad Sci USA. 1982;79:4471–5.
Savage AP, Adrian TE, Carolan G, et al. Effects of peptide YY (PYY) on mouth to caecum intestinal transit time and on the rate of gastric emptying in healthy volunteers. Gut. 1987;28:166–70.
Imamura M. Effects of surgical manipulation of the intestine on peptide YY and its physiology. Peptides. 2002;23:403–7.
Van Citters GW, Lin HC. The ileal brake: a 15-year progress report. Curr Gastroenterol Rep. 1999;1:404–9.
Adrian TE, Long RG, Fuessl HS, et al. Plasma peptide YY (PYY) in dumping syndrome. Dig Dis Sci. 1985;30:1145–8.
Allen JM, Fitzpatrick ML, Yeats JC, et al. Effects of peptide YY and neuropeptide Y on gastric emptying in man. Digestion. 1984;30:255–62.
Ukleja A. Dumping syndrome: pathophysiology and treatment. Nutr Clin Pract. 2005;20:517–25.
Holdstock C, Zethelius B, Sundbom M, et al. Postprandial changes in gut regulatory peptides in gastric bypass patients. Int J Obes (Lond). 2008;32:1640–6.
Gryback P, Hermansson G, Lyrenas E, et al. Nationwide standardisation and evaluation of scintigraphic gastric emptying: reference values and comparisons between subgroups in a multicentre trial. Eur J Nucl Med. 2000;27:647–55.
Gryback P, Bajc M, Granerus G, et al. [Examination of gastric emptying with gamma camera. Clinically useful, uniform method now established]. Lakartidningen. 2000;97:1811–6.
Sanchez-Pernaute A, Rodriguez R, Rubio MA, et al. Gastric tube volume after duodenal switch and its correlation to short-term weight loss. Obes Surg. 2007;17:1178–82.
Moore JG, Christian PE, Coleman RE. Gastric emptying of varying meal weight and composition in man. Evaluation by dual liquid- and solid-phase isotopic method. Dig Dis Sci. 1981;26:16–22.
Naslund E, Gryback P, Hellstrom PM, et al. Gastrointestinal hormones and gastric emptying 20 years after jejunoileal bypass for massive obesity. Int J Obes Relat Metab Disord. 1997;21:387–92.
Batterham RL, Cohen MA, Ellis SM, et al. Inhibition of food intake in obese subjects by peptide YY3-36. N Engl J Med. 2003;349:941–8.
Stock S, Leichner P, Wong AC, et al. Ghrelin, peptide YY, glucose-dependent insulinotropic polypeptide, and hunger responses to a mixed meal in anorexic, obese, and control female adolescents. J Clin Endocrinol Metab. 2005;90:2161–8.
Kim BJ, Carlson OD, Jang HJ, et al. Peptide YY is secreted after oral glucose administration in a gender-specific manner. J Clin Endocrinol Metab. 2005;90:6665–71.
Boggiano MM, Chandler PC, Oswald KD, et al. PYY3-36 as an anti-obesity drug target. Obes Rev. 2005;6:307–22.
Johansson HE, Haenni A, Karlsson FA, et al. Bileopancreatic diversion with duodenal switch lowers both early and late phases of glucose, insulin and proinsulin responses after meal. Obes Surg. 2010;20:549–58.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hedberg, J., Hedenström, H., Karlsson, F.A. et al. Gastric Emptying and Postprandial PYY Response After Biliopancreatic Diversion with Duodenal Switch. OBES SURG 21, 609–615 (2011). https://doi.org/10.1007/s11695-010-0288-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-010-0288-7