Abstract
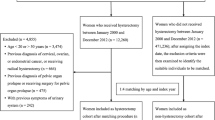
Approximately one million hysterectomies are performed each year in China. However, national data regarding the indications and the surgical approaches for hysterectomy are lacking. The aim of this study was to examine the surgical indications for hysterectomy in different age groups and the relative merits of different surgical approaches for hysterectomy in Chinese women. Clinical data from 4653 cases of hysterectomy performed in Tongji Hospital from 2004 to 2009 were analysed. Hysterectomy was most commonly performed among women aged 40–49 years (2299; 49.4%). Overall, colporrhagia and abdominal pain were the two most common indications for hysterectomy. The most common indications by age groups were as follows: malignant ovarian tumour, < 20 years; malignant uterine tumour, 20–29 and 30–39 years; uterine myoma, 40–49 and 50–59 years; and uterine prolapse, 60–69 and > 70 years. The proportion of malignant aetiology also varied by age, being the highest in women aged < 20 years (75.0%) and the lowest in those aged 40–49 years (19.9%). Approximately 35% women who had hysterectomies also had concomitant bilateral oophorectomy. The lowest rate of oophorectomy occurred in women aged 30–39 years (15.8%), whereas the highest rate was in those aged 50–59 years (75.9%). The abdominal surgical approach was used in 84% of all hysterectomies. Surgeries using the vaginal approach required a significantly shorter operating time (118 min average) than all other approaches (P < 0.05). Both the amount of bleeding and the blood transfusion volume required were smaller in vaginal approaches, with no significant differences between the others. The surgical approaches used were also related to the scope of surgery. Both the surgical indications and the rates of bilateral oophorectomy varied by age. In terms of both operating time and the amount of bleeding and blood transfusion volume required, the vaginal approach was superior to all other surgical approaches.
Similar content being viewed by others
References
Whiteman MK, Hillis SD, Jamieson DJ, Morrow B, Podgornik MN, Brett KM, Marchbanks PA. Inpatient hysterectomy surveillance in the United States, 2000–2004. Am J Obstet Gynecol 2008; 198: 34.e1–e7
Clarke-Pearson DL, Geller EJ. Complications of hysterectomy. Obstet Gynecol 2013;121(3): 654–673
Schaffer JI, Word A. Hysterectomy-still a useful operation. N Engl J Med 2002;347(17): 1360–1362
Kuppermann M, Learman LA, Schembri M, Gregorich SE, Jackson RA, Jacoby A, Lewis J, Washington AE. Contributions of hysterectomy and uterus-preserving surgery to health-related quality of life. Obstet Gynecol 2013;122(1): 15–25
Nieboer TE, Johnson N, Lethaby A, Tavender E, Curr E, Garry R, van Voorst S, Mol BW, Kluivers KB. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev 2009;(3): CD003677
Baskett TF. Hysterectomy: evolution and trends. Best Pract Res Clin Obstet Gynaecol 2005;19(3): 295–305
Shifren JL, Avis NE. Surgical menopause: effects on psychological well-being and sexuality. Menopause 2007; 14(3 Pt 2 Suppl. 1): 586–591
Lieng M, Lomo AB, Qvigstad E. Long-term outcomes following laparoscopic and abdominal supracervical hysterectomies. Obstet Gynecol Int 2010;2010: 989127
ACOG Committee Opinion No. 444: choosing the route of hysterectomy for benign disease. Obstet Gynecol 2009; 114(5): 1156–1158
Liu H, Lu D, Wang L, Shi G, Song H, Clarke J. Robotic surgery for benign gynaecological disease. Cochrane Database Syst Rev 2012;2: CD008978
O’Neill M, Moran PS, Teljeur C, O’Sullivan OE, O’Reilly BA, Hewitt M, Flattery M, Ryan M. Robot-assisted hysterectomy compared to open and laparoscopic approaches: systematic review and meta-analysis. Arch Gynecol Obstet 2013;287(5): 907–918
Wright JD, Ananth CV, Lewin SN, Burke WM, Lu YS, Neugut AI, Herzog TJ, Hershman DL. Robotically assisted vs laparoscopic hysterectomy among women with benign gynecologic disease. JAMA 2013;309(7): 689–698
Parker WH. Ovarian conservation versus bilateral oophorectomy at the time of hysterectomy for benign disease. Menopause 2014;21(2): 192–194
Borghese B, Chapron C. Treatment of symptomatic uterine fibroids. N Engl J Med 2007;356(21): 2218–2219, author reply 2219
Carlson KJ, Nichols DH, Schiff I. Indications for hysterectomy. N Engl J Med 1993;328(12): 856–860
Merrill RM. Hysterectomy surveillance in the United States, 1997 through 2005. Med Sci Monit 2008;14(1): CR24–CR31
Johnson N, Barlow D, Lethaby A, Tavender E, Curr L, Garry R. Methods of hysterectomy: systematic review and meta-analysis of randomised controlled trials. BMJ 2005;330(7506): 1478
Hanwright PJ, Mioton LM, Thomassee MS, Bilimoria KY, Van Arsdale J, Brill E, Kim JY. Risk profiles and outcomes of total laparoscopic hysterectomy compared with laparoscopically assisted vaginal hysterectomy. Obstet Gynecol 2013;121(4): 781–787
Hickey M, Ambekar M, Hammond I. Should the ovaries be removed or retained at the time of hysterectomy for benign disease? Hum Reprod Update 2010;16(2): 131–141
Perera HK, Ananth CV, Richards CA, Neugut AI, Lewin SN, Lu YS, Herzog TJ, Hershman DL, Wright JD. Variation in ovarian conservation in women undergoing hysterectomy for benign indications. Obstet Gynecol 2013;121(4): 717–726
Korbly NB, Kassis NC, Good MM, Richardson ML, Book NM, Yip S, Saguan D, Gross C, Evans J, Lopes VV, Harvie HS, Sung VW. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol 2013; 209: 470.e1–e6
Shuster LT, Gostout BS, Grossardt BR, Rocca WA. Prophylactic oophorectomy in premenopausal women and long-term health. Menopause Int 2008;14(3): 111–116
Özdemir S, Celik C, Görkemli H, Kiyici A, Kaya B. Compared effects of surgical and natural menopause on climacteric symptoms, osteoporosis, and metabolic syndrome. Int J Gynaecol Obstet 2009;106(1): 57–61
Henderson VW, Sherwin BB. Surgical versus natural menopause: cognitive issues. Menopause 2007; 14(3 Pt 2 Suppl.1): 572–579
Jacoby VL, Vittinghoff E, Nakagawa S, Jackson R, Richter HE, Chan J, Kuppermann M. Factors associated with undergoing bilateral salpingo-oophorectomy at the time of hysterectomy for benign conditions. Obstet Gynecol 2009;113(6): 1259–1267
Author information
Authors and Affiliations
Corresponding author
Additional information
Jingjing Jiang and Ting Ding contributed equally to this article.
Rights and permissions
About this article
Cite this article
Jiang, J., Ding, T., Luo, A. et al. Comparison of surgical indications for hysterectomy by age and approach in 4653 Chinese women. Front. Med. 8, 464–470 (2014). https://doi.org/10.1007/s11684-014-0338-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11684-014-0338-y