Abstract
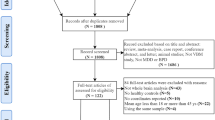
Although previous imaging studies in borderline personality disorder (BPD) have found brain abnormalities, the results have been inconsistent. This study aimed to investigate structural brain abnormalities using voxel-based morphometry (VBM) and cortical thickness (Cth) analyses in a large sample of patients with BPD. Additionally, we aimed to determine the correlation between structural abnormalities and clinical severity and to assess its potential value at predicting psychotherapeutic response. Sixty-one individuals with BPD and 19 healthy controls underwent magnetic resonance imaging. Participants with BPD completed several self-report clinical scales, received dialectical-behavioral therapy skills training and post-therapy changes in clinical scores were also recorded. Gray matter volume (GMV) and Cth differences between groups were compared. Within the BPD group, we further characterized the structural brain correlates of clinical severity and investigated the relationship between pre-therapy structural abnormalities and therapeutic response. As potential confounders we included age, sex, educational level, and total intracranial volume (the latter only in VBM analyses). Compared to controls, the BPD group showed a reduced GMV/Cth in prefrontal areas but increased GMV in the limbic structures (amygdala and parahippocampal regions). Prefrontal abnormalities correlated with higher baseline scores on impulsivity and general BPD severity. Increased GMV in the parahippocampal area correlated with a greater emotion dysregulation. Importantly, several baseline structural abnormalities correlated with worse response to psychotherapy. Patients with BPD showed a reduced GMV in the prefrontal areas but a greater GMV in the limbic structures. Several structural abnormalities (i.e. middle and inferior prefrontal areas, anterior insula, or parahippocampal area) correlated with clinical severity and could potentially be used as imaging biological correlates biomarkers to predict psychotherapy response.



Similar content being viewed by others
References
Aguilar-Ortiz, S., Salgado-Pineda, P., Marco-Pallarés, J., Pascual, J. C., Vega, D., Soler, J., … McKenna, P. J. (2018). Abnormalities in gray matter volume in patients with borderline personality disorder and their relation to lifetime depression: A VBM study. PLOS ONE, 13(2), e0191946-. Retrieved from https://doi.org/10.1371/journal.pone.0191946
American Psychiatric Association. (2018). DSM-5, manual diagnóstico y estadístico de los trastornos mentales. Editorial Médica Panamericana. Retrieved from https://www.medicapanamericana.com/Libros/Libro/6194/DSM5-Manual-Diagnostico-y-Estadistico-de-los-Trastornos-Mentales-Incluye-acceso-a-eBook.html
Arens, E. A., Stopsack, M., Spitzer, C., Appel, K., Dudeck, M., Völzke, H., et al. (2013). Borderline personality disorder in four different age groups: A cross-sectional study of community residents in Germany. Journal of Personality Disorders, 27(2), 196–207. https://doi.org/10.1521/pedi_2013_27_072.
Barrachina, J., Soler, J., Campins, M. J., Tejero, A., Pascual, J. C., Alvarez, E., & Pérez, V. (2004). Validación de la versión española de la Diagnostic Interview for Borderline Revised (DIB-R). Actas Esp Psiquiatr, 32(5), 293–298.
Barratt, E. S., Patton, J., & Stanford, M. (1975). Barratt Impulsiveness Scale. Barratt-Psychiatry Medical Branch: University of Texas Texas.
Barth, C., Jørgensen, K. N., Wortinger, L. A., Nerland, S., Jönsson, E. G., & Agartz, I. (2020). Trajectories of brain volume change over 13 years in chronic schizophrenia. Schizophrenia Research. https://doi.org/10.1016/j.schres.2020.05.01.
Berlin, H. A., Rolls, E. T., & Iversen, S. D. (2005). Borderline personality disorder, impulsivity, and the orbitofrontal cortex. American Journal of Psychiatry, 162(12), 2360–2373. https://doi.org/10.1176/appi.ajp.162.12.2360.
Blair, R. J. R. (2015). The neurobiology of impulsive aggression. Journal of Child and Adolescent Psychopharmacology, 26(1), 4–9. https://doi.org/10.1089/cap.2015.0088.
Blankstein, U., Chen, J. Y., Mincic, A. M., McGrath, P. A., & Davis, K. D. (2009). The complex minds of teenagers: neuroanatomy of personality differs between sexes. Neuropsychologia, 47(2), 599–603. https://doi.org/10.1016/j.neuropsychologia.2008.10.014.
Bohus, M., Kleindienst, N., Limberger, M. F., Stieglitz, R.-D., Domsalla, M., Chapman, A. L., et al. (2009). The short version of the borderline symptom list (BSL-23): Development and initial data on psychometric properties. Psychopathology, 42(1), 32–39.
Bruehl, H., Preißler, S., Heuser, I., Heekeren, H. R., Roepke, S., & Dziobek, I. (2013). Increased prefrontal cortical thickness is associated with enhanced abilities to regulate emotions in PTSD-free women with borderline personality disorder. PLoS ONE, 8(6), e65584. https://doi.org/10.1371/journal.pone.0065584.
Brunner, R., Henze, R., Parzer, P., Kramer, J., Feigl, N., Lutz, K., … Stieltjes, B. (2010). Reduced prefrontal and orbitofrontal gray matter in female adolescents with borderline personality disorder: Is it disorder specific? NeuroImage, 49(1), 114–120. https://doi.org/10.1016/J.NEUROIMAGE.2009.07.070
Cackowski, S., Reitz, A., Ende, G., Kleindienst, N., Bohus, M., Schmahl, C., & Krause-Utz, A. (2014). Impact of stress on different components of impulsivity in borderline personality disorder. Psychological Medicine, 44(15), 3329–3340. https://doi.org/10.1017/S0033291714000427.
Crowell, S. E., Beauchaine, T. P., & Linehan, M. M. (2009). A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin, 135(3), 495–510.
de Araujo Filho, G. M., Abdallah, C., Sato, J. R., de Araujo, T. B., Lisondo, C. M., de Faria, Á. A., … Jackowski, A. P. (2014). Morphometric hemispheric asymmetry of orbitofrontal cortex in women with borderline personality disorder: A multi-parameter approach. Psychiatry Research: Neuroimaging, 223(2), 61–66. https://doi.org/10.1016/J.PSCYCHRESNS.2014.05.001
Draganski, B., Gaser, C., Kempermann, G., Kuhn, H. G., Winkler, J., Büchel, C., & May, A. (2006). Temporal and spatial dynamics of brain structure changes during extensive learning. The Journal of Neuroscience, 26(23), 6314. https://doi.org/10.1523/JNEUROSCI.4628-05.2006
First, M. B., Gibbon, M., Spitzer, R. L., & Benjamin, L. S. (1997). User’s guide for the structured clinical interview for DSM-IV axis II personality disorders: SCID-II. American Psychiatric Pub.
Fischl, B., & Dale, A. M. (2000). Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proceedings of the National Academy of Sciences, 97(20), 11050. https://doi.org/10.1073/pnas.200033797.
Fjell, A. M., Westlye, L. T., Amlien, I., Espeseth, T., Reinvang, I., Raz, N., … Walhovd, K. B. (2009). High Consistency of Regional Cortical Thinning in Aging across Multiple Samples. Cerebral Cortex, 19(9), 2001–2012. https://doi.org/10.1093/cercor/bhn232
Giuliani, N. R., Calhoun, V. D., Pearlson, G. D., Francis, A., & Buchanan, R. W. (2005). Voxel-based morphometry versus region of interest: a comparison of two methods for analyzing gray matter differences in schizophrenia. Schizophrenia Research, 74(2–3), 135–147. https://doi.org/10.1016/J.SCHRES.2004.08.019.
Gómez-Beneyto, M., Villar, M., Renovell, M., Pérez, F., Hernandez, M., Leal, C., … Asencio, A. (1994). The diagnosis of personality disorder with a modified version of the SCID-II in a Spanish clinical sample. Journal of Personality Disorders, 8(2), 104–110.
Gratz, K. L., & Roemer, L. (2008). The relationship between emotion dysregulation and deliberate self-harm among female undergraduate students at an urban commuter university. Cognitive Behaviour Therapy, 37(1), 14–25.
Gratz, K. L., Rosenthal, M. Z., Tull, M. T., Lejuez, C. W., & Gunderson, J. G. (2010). An experimental investigation of emotional reactivity and delayed emotional recovery in borderline personality disorder: the role of shame. Comprehensive Psychiatry, 51(3), 275–285.
Hervás, G., & Jódar, R. (2008). Adaptación al castellano de la Escala de Dificultades en la Regulación Emocional. Clínica y Salud, 19(2), 139–156.
Klein, A., Ghosh, S. S., Avants, B., Yeo, B. T. T., Fischl, B., Ardekani, B., … Parsey, R. V. (2010). Evaluation of volume-based and surface-based brain image registration methods. NeuroImage, 51(1), 214–220. https://doi.org/10.1016/J.NEUROIMAGE.2010.01.091
Krause-Utz, A., Winter, D., Niedtfeld, I., & Schmahl, C. (2014). The latest neuroimaging findings in borderline personality disorder. topical collection on personality disorders. o, 16(3). https://doi.org/10.1007/s11920-014-0438-z.
Lange, C., & Irle, E. (2004). Enlarged amygdala volume and reduced hippocampal volume in young women with major depression. Psychological Medicine, 34(6), 1059–1064. https://doi.org/10.1017/S0033291703001806.
Leichsenring, F., Leibing, E., Kruse, J., New, A. S., & Leweke, F. (2011). Borderline personality disorder. The Lancet, 377(9759), 74–84.
Linehan, M. (1993). Cognitive-behavioral treatment of borderline personality disorder. Guilford Press.
Mancke, F., Schmitt, R., Winter, D., Niedtfeld, I., Herpertz, S. C., & Schmahl, C. (2018). Assessing the marks of change: How psychotherapy alters the brain structure in women with borderline personality disorder. Journal of Psychiatry and Neuroscience. https://doi.org/10.1503/jpn.170132.
Martín-Blanco, A., Ancochea, A., Soler, J., Elices, M., Carmona, C., & Pascual, J. C. (2017). Changes over the last 15 years in the psychopharmacological management of persons with borderline personality disorder. Acta Psychiatrica Scandinavica, 136(3), 323–331. https://doi.org/10.1111/acps.12767.
Martinez-Horta, S., Sampedro, F., Pagonabarraga, J., Fernandez-Bobadilla, R., Marin-Lahoz, J., Riba, J., & Kulisevsky, J. (2017). Non-demented Parkinson’s disease patients with apathy show decreased grey matter volume in key executive and reward-related nodes. Brain Imaging and Behavior, 11(5), 1334–1342. https://doi.org/10.1007/s11682-016-9607-5.
McGarry, L. M., & Carter, A. G. (2017). Prefrontal cortex drives distinct projection neurons in the basolateral amygdala. Cell Rep, 21(6), 1426–1433.
Minzenberg, M. J., Fan, J., New, A. S., Tang, C. Y., & Siever, L. J. (2008). Frontolimbic structural changes in borderline personality disorder. Journal of Psychiatric Research, 42(9), 727–733. https://doi.org/10.1016/J.JPSYCHIRES.2007.07.015.
New, A., Hazlett, E., Buchsbaum, M., Goodman, M., Mitelman, S., Newmark, R., & …Siever L. (2007). Amygdala–prefrontal disconnection in borderline personality disorder. Neuropsychopharmacol., 32, 1629–1640. https://doi.org/10.1038/sj.npp.1301283.
Nunes, P. M., Wenzel, A., Borges, K. T., Porto, C. R., Caminha, R. M., & de Oliveira, I. R. (2009). Volumes of the hippocampus and amygdala in patients with borderline personality disorder: a meta-analysis. Journal of Personality Disorders, 23(4), 333–345. https://doi.org/10.1521/pedi.2009.23.4.333.
Oquendo, M. A., Baca-García, E., Graver, R., Morales, M., Montalban, V., & Mann, J. J. (2001). Spanish adaptation of Barratt Impulsiveness Scale (BIS). European Journal of Psychiatry, 15, 147–155.
Osborne, T. L., Michonski, J., Sayrs, J., Welch, S. S., & Anderson, L. K. (2017). Factor structure of the difficulties in emotion regulation scale (DERS) in adult outpatients receiving dialectical behavior therapy (DBT). Journal of Psychopathology and Behavioral Assessment, 39(2), 355–371. https://doi.org/10.1007/s10862-017-9586-x.
Penadés, R., Pujol, N., Catalán, R., Massana, G., Rametti, G., García-Rizo, C., … Junqué, C. (2013). Brain Effects of Cognitive Remediation Therapy in Schizophrenia: A Structural and Functional Neuroimaging Study. Biological Psychiatry, 73(10), 1015–1023. https://doi.org/10.1016/J.BIOPSYCH.2013.01.017
Poldrack, R. A., Baker, C. I., Durnez, J., Gorgolewski, K. J., Matthews, P. M., Munafò, M. R., et al. (2017). Scanning the horizon: towards transparent and reproducible neuroimaging research. Nat Rev Neurosci., 18(2), 115–126. https://doi.org/10.1038/nrn.2016.167.
Rajagopalan, V., & Pioro, E. P. (2015). Disparate voxel based morphometry (VBM) results between SPM and FSL softwares in ALS patients with frontotemporal dementia: which VBM results to consider? BMC Neurol, 15, 32. https://doi.org/10.1186/s12883-015-0274-8.
Righart, R., Schmidt, P., Dahnke, R., Biberacher, V., Beer, A., Buck, D., et al. (2017). Volume versus surface-based cortical thickness measurements: A comparative study with healthy controls and multiple sclerosis patients. PLoS ONE, 12(7), e0179590. https://doi.org/10.1371/journal.pone.0179590.
Rossi, R., Lanfredi, M., Pievani, M., Boccardi, M., Rasser, P. E., Thompson, P. M., … Frisoni, G. B. (2015). Abnormalities in cortical gray matter density in borderline personality disorder. European Psychiatry : The Journal of the Association of European Psychiatrists, 30(2), 221–227 https://doi.org/10.1016/j.eurpsy.2014.11.009
Ruocco, A. C., Amirthavasagam, S., Choi-Kain, L. W., & McMain, S. F. (2013). Neural correlates of negative emotionality in borderline personality disorder: An activation-likelihood-estimation meta-analysis. Biological Psychiatry. https://doi.org/10.1016/j.biopsych.2012.07.014.
Rüsch, N., Elst, L. T. van, Ludaescher, P., Wilke, M., Huppertz, H.-J., Thiel, T., … Ebert, D. (2003). A voxel-based morphometric MRI study in female patients with borderline personality disorder. NeuroImage, 20(1), 385–392. https://doi.org/10.1016/S1053-8119(03)00297-0
Salavert, J., Gasol, M., Vieta, E., Cervantes, A., Trampal, C., & Gispert, J. D. (2011). Fronto-limbic dysfunction in borderline personality disorder: A 18F-FDG positron emission tomography study. Journal of Affective Disorders, 131(1–3), 260–267. https://doi.org/10.1016/J.JAD.2011.01.001.
Salvador, R., Vega, D., Pascual, J. C., Marco, J., Canales-Rodríguez, E. J., Aguilar, S., … Pomarol-Clotet, E. (2016). Converging medial frontal resting state and diffusion-based abnormalities in borderline personality disorder. Biological Psychiatry. https://doi.org/10.1016/j.biopsych.2014.08.026
Schulze, L., Schmahl, C., & Niedtfeld, I. (2016). Neural correlates of disturbed emotion processing in borderline personality disorder: A multimodal meta-analysis. Biological Psychiatry, 79(2), 97–106. https://doi.org/10.1016/J.BIOPSYCH.2015.03.027.
Soler, J., Vega, D., Feliu-Soler, A., Trujols, J., Soto, Á., Elices, M., … Pascual, J. C. (2013). Validation of the spanish version of the borderline symptom list, short form (BSL-23). BMC Psychiatry, 13(1), 1317.
Soloff, P. H., Meltzer, C. C., Becker, C., Greer, P. J., Kelly, T. M., & Constantine, D. (2003). Impulsivity and prefrontal hypometabolism in borderline personality disorder. Psychiatry Research, 123(3), 153–63. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12928103
Soloff, P., Nutche, J., Goradia, D., & Diwadkar, V. (2008). Structural brain ies in borderline personality disorder: A voxel-based morphometry study. Psychiatry Research: Neuroimaging, 164(3), 223–236. https://doi.org/10.1016/J.PSCYCHRESNS.2008.02.003.
Tebartz van Elst, L., Hesslinger, B., Thiel, T., Geiger, E., Haegele, K., Lemieux, L., … Ebert, D. (2003). Frontolimbic brain abnormalities in patients with borderline personality disorder: a volumetric magnetic resonance imaging study. Biological Psychiatry, 54(2), 163–71. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12873806
Visintin, E., De Panfilis, C., Amore, M., Balestrieri, M., Wolf, R. C., & Sambataro, F. (2016). Mapping the brain correlates of borderline personality disorder: A functional neuroimaging meta-analysis of resting state studies. Journal of Affective Disorders. https://doi.org/10.1016/j.jad.2016.07.025
Wolf, R. C., Thomann, P. A., Sambataro, F., Vasic, N., Schmid, M., & Wolf, N. D. (2012). Orbitofrontal cortex and impulsivity in borderline personality disorder: An MRI study of baseline brain perfusion. European Archives of Psychiatry and Clinical Neuroscience, 262(8), 677–685. https://doi.org/10.1007/s00406-012-0303-1.
Zetzsche, T., Frodl, T., Preuss, U. W., Schmitt, G., Seifert, D., Leinsinger, G., … Meisenzahl, E. M. (2006). Amygdala volume and depressive symptoms in patients with borderline personality disorder. Biological Psychiatry, 60(3), 302–310. https://doi.org/10.1016/J.BIOPSYCH.2005.11.020
Zhao, K., Liu, H., Yan, R., Hua, L., Chen, Y., Shi, J., … Yao, Z. (2017). Cortical thickness and subcortical structure volume abnormalities in patients with major depression with and without anxious symptoms. Brain and Behavior, 7(8), e00754. https://doi.org/10.1002/brb3.754
Zhou, Q., Zhong, M., Yao, S., Jin, X., Liu, Y., Tan, C., … Yi, J. (2017). Hemispheric asymmetry of the frontolimbic cortex in young adults with borderline personality disorder. Acta Psychiatrica Scandinavica, 136(6), 637–647. https://doi.org/10.1111/acps.12823
Acknowledgments
This study was supported by Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM) and by a grant from Instituto de Salud Carlos III (PI13/00134) and co-financed by the European Regional Development Fund (ERDF). ME has a Juan de la Cierva research contract awarded by the ISCIII (FJCI-2017-31738). ME wants to thank unrestricted research funding from “Secretaria d′Universitats i Recerca del Departament d′Economia i Coneixement (2017 SGR 134 to “Mental Health Research Group”), Generalitat de Catalunya (Government of Catalonia). The contribution of CS is also supported by CONICYT PFCHA/BCH 72190624 scholarship. We thank Bradley Londres for professional English language editing.
Author information
Authors and Affiliations
Contributions
JS, JCP, IC and EPC conceived the study. FS and RS performed the neuroimaging procedures and statistical analyses. CCF and CS drafted the first version of the manuscript. JS and ME performed the psychotherapeutic intervention. All authors contributed to the writing and reviewing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sampedro, F., Farrés, C.C.i., Soler, J. et al. Structural brain abnormalities in borderline personality disorder correlate with clinical severity and predict psychotherapy response. Brain Imaging and Behavior 15, 2502–2512 (2021). https://doi.org/10.1007/s11682-021-00451-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-021-00451-6