Abstract
Summary
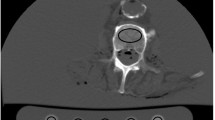
The patient’s position may affect the bone mineral density (BMD) measurements; however, the extent of this effect is undefined. This CT image-based simulation study quantified changes in BMD induced by hip flexion, adduction, and rotations to recommend appropriate patient positioning when acquiring dual-energy x-ray absorptiometry images.
Purpose
Several studies have analyzed the effect of hip rotation on the measurement of bone mineral density (BMD) of the proximal femur by dual-energy x-ray absorptiometry (DXA). However, as the effects of hip flexion and abduction on BMD measurements remain uncertain, a computational simulation study using CT images was performed in this study.
Methods
Hip CT images of 120 patients (33 men and 87 women; mean age, 82.1 ± 9.4 years) were used for analysis. Digitally reconstructed radiographs of the proximal femur region were generated from CT images to calculate the BMD of the proximal femur region. BMD at the neutral position was quantified, and the percent changes in BMD when hip internal rotation was altered from −30° to 15°, when hip flexion was altered from 0° to 30°, and when hip abduction was altered from –15° to 30° were quantified. Analyses were automatically performed with a 1° increment in each direction using computer programming.
Results
The alteration of hip angles in each direction affected BMD measurements, with the largest changes found for hip flexion (maximum change of 17.7% at 30° flexion) and the smallest changes found for hip rotation (maximum change of 2.2% at 15° internal rotation). The BMD measurements increased by 0.34% for each 1° of hip abduction, and the maximum change was 12.3% at 30° abduction.
Conclusion
This simulation study quantified the amount of BMD change induced by altering the hip position. Based on these results, we recommend that patients be positioned carefully when acquiring DXA images.





Similar content being viewed by others
Data availability
Data used for this study can be made available by submitting on reasonable request to the corresponding author. Codes and models used in this study are available at https://github.com/keisuke-uemura/proximal_femur_BMD_measurement.
References
Soen S, Fukunaga M, Sugimoto T et al (2013) Diagnostic criteria for primary osteoporosis: year 2012 revision. J Bone Miner Metab 31:247–257. https://doi.org/10.1007/s00774-013-0447-8
Jain RK, Vokes T (2017) Dual-energy X-ray absorptiometry. J Clin Densitom 20:291–303. https://doi.org/10.1016/j.jocd.2017.06.014
Kanis JA, Cooper C, Rizzoli R et al (2019) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 30:3–44. https://doi.org/10.1007/s00198-018-4704-5
Morgan SL, Prater GL (2017) Quality in dual-energy X-ray absorptiometry scans. Bone 104:13–28. https://doi.org/10.1016/j.bone.2017.01.033
Wong CP, Gani LU, Chong LR (2020) Dual-energy X-ray absorptiometry bone densitometry and pitfalls in the assessment of osteoporosis: a primer for the practicing clinician. Arch Osteoporos 15:135. https://doi.org/10.1007/s11657-020-00808-2
Albano D, Agnollitto PM, Petrini M et al (2021) Operator-related errors and pitfalls in dual energy X-ray absorptiometry: how to recognize and avoid them. Acad Radiol 28:1272–1286. https://doi.org/10.1016/j.acra.2020.07.028
Goh JCH, Low SL, Bose K (1995) Effect of femoral rotation on bone mineral density measurements with dual energy X-ray absorptiometry. Calcif Tissue Int 57:340–343. https://doi.org/10.1007/BF00302069
Lekamwasam S, Sumith R, Lenora J (2003) Effect of leg rotation on hip bone mineral density measurements. J Clin Densitom 6:331–336. https://doi.org/10.1385/JCD:6:4:331
Qutbi M, Salek A, Soltanshahi M et al (2019) The impact of nonstandard hip rotation on densitometric results of hip regions and potential misclassification of diagnosis. Arch Osteoporos 14:86. https://doi.org/10.1007/s11657-019-0635-9
Rosenthall L (2004) Range of change of measured BMD in the femoral neck and total hip with rotation in women. J Bone Miner Metab 22. https://doi.org/10.1007/s00774-004-0513-3
Faizan A, Gerges JJ, Asencio G et al (2016) Changes in femoral version during implantation of anatomic stems: implications on stem design. J Arthroplasty 31:512–516. https://doi.org/10.1016/j.arth.2015.09.008
Pierrepont JW, Marel E, Baré JV et al (2020) Variation in femoral anteversion in patients requiring total hip replacement. HIP Int 30:281–287. https://doi.org/10.1177/1120700019848088
Watt JR, Jackson K, Franz JR et al (2011) Effect of a supervised hip flexor stretching program on gait in frail elderly patients. PM&R 3:330–335. https://doi.org/10.1016/j.pmrj.2011.01.006
Tani T, Ando W, Hamada H et al (2021) Hip subluxation and osteophye morphology are related to coronal contracture of the hip. J Orthop Res 39:1691–1699. https://doi.org/10.1002/jor.24891
Uemura K, Otake Y, Takao M et al (2022) Development of an open-source measurement system to assess the areal bone mineral density of the proximal femur from clinical CT images. Arch Osteoporos 17:17. https://doi.org/10.1007/s11657-022-01063-3
Karahan AY, Kaya B, Kuran B et al (2016) Common mistakes in the dual-energy X-ray absorptiometry (DXA) in Turkey. A retrospective descriptive multicenter study. Acta Med (Hradec Kralove, Czech Repub) 59:117–123. https://doi.org/10.14712/18059694.2017.38
Maldonado G, Intriago M, Larroude M et al (2020) Common errors in dual-energy X-ray absorptiometry scans in imaging centers in Ecuador. Arch Osteoporos 15:6. https://doi.org/10.1007/s11657-019-0673-3
Kamihata S, Ando W, Takao M et al (2022) Effect of hip flexion contracture on the pelvic sagittal tilt in the supine position: a retrospective case-series study. Modern Rheumatology roac110. https://doi.org/10.1093/mr/roac110 (in press)
Otake Y, Armand M, Armiger RS et al (2012) Intraoperative image-based multiview 2D/3D registration for image-guided orthopaedic surgery: incorporation of fiducial-based C-Arm tracking and GPU-acceleration. IEEE Trans Med Imaging 31:948–962. https://doi.org/10.1109/TMI.2011.2176555
Uemura K, Otake Y, Takao M et al (2021) Automated segmentation of an intensity calibration phantom in clinical CT images using a convolutional neural network. Int J CARS 16:1855–1864. https://doi.org/10.1007/s11548-021-02345-w
Engelke K, Lang T, Khosla S et al (2015) Clinical use of quantitative computed tomography (QCT) of the hip in the management of osteoporosis in adults: the 2015 ISCD Official Positions-Part I. J Clin Densitom 18:338–358. https://doi.org/10.1016/j.jocd.2015.06.012
Lewiecki EM, Binkley N, Morgan SL et al (2016) Best practices for dual-energy X-ray absorptiometry measurement and reporting: International Society for Clinical Densitometry Guidance. J Clin Densitom 19:127–140. https://doi.org/10.1016/j.jocd.2016.03.003
Fan B, Lu Y, Genant H et al (2010) Does standardized BMD still remove differences between Hologic and GE-Lunar state-of-the-art DXA systems? Osteoporos Int 21:1227–1236. https://doi.org/10.1007/s00198-009-1062-3
Feit A, Levin N, McNamara EA et al (2020) Effect of positioning of the region of interest on bone density of the hip. J Clin Densitom 23:426–431. https://doi.org/10.1016/j.jocd.2019.04.002
Uemura K, Takao M, Otake Y et al (2022) The effect of region of interest on measurement of bone mineral density of the proximal femur: simulation analysis using CT images. Calcif Tissue Int 111:475–484. https://doi.org/10.1007/s00223-022-01012-9
Abe H, Sakai T, Takao M et al (2015) Difference in stem alignment between the direct anterior approach and the posterolateral approach in total hip arthroplasty. J Arthroplasty 30:1761–1766. https://doi.org/10.1016/j.arth.2015.04.026
Shimosawa H, Nagura T, Harato K et al (2019) Variation of three-dimensional femoral bowing and its relation to physical status and bone mineral density: a study with CT. Surg Radiol Anat 41:1489–1495. https://doi.org/10.1007/s00276-019-02323-7
Zhang J-Z, Zhao K, Li J-Y et al (2020) Age-related dynamic deformation of the femoral shaft and associated osteoporotic factors: a retrospective study in Chinese adults. Arch Osteoporos 15:157. https://doi.org/10.1007/s11657-020-00834-0
Acknowledgements
We thank Dr. Tatsuya Kitaura for his help in the acquisition of data.
Funding
This study was supported by the Japan Osteoporosis Foundation Grant for Bone Research and the Japan Society for the Promotion of Science Grants-in-Aid for Scientific Research (KAKENHI) (grant numbers 19H01176, 20H04550, and 21K16655).
Author information
Authors and Affiliations
Contributions
Keisuke Uemura: conceptualization, methodology, code writing, validation, formal analysis, data curation, writing–original draft and review and editing, visualization, funding acquisition. Masaki Takao: writing–review and editing, supervision. Yoshito Otake: resources, methodology, writing–review and editing, supervision, funding acquisition. Kazuma Takashima: writing–review and editing. Hidetoshi Hamada: writing–review and editing. Wataru Ando: writing–review and editing. Yoshinobu Sato: resources, writing–review and editing, supervision, funding acquisition. Nobuhiko Sugano: writing–review and editing, supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in this study were performed according to the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to participate
This study was approved by the Institutional Review Board of each participating institution, and informed consent was obtained from all patients in the form of opt-out.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Uemura, K., Takao, M., Otake, Y. et al. The effect of patient positioning on measurements of bone mineral density of the proximal femur: a simulation study using computed tomographic images. Arch Osteoporos 18, 35 (2023). https://doi.org/10.1007/s11657-023-01225-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-023-01225-x