Abstract
Summary
We explored how the severity of radiological osteoporotic vertebral fracture (OVF) can be converted to the equivalent T-score values.
Introduction
To perform a study to define what portion of older community women with what severity of radiographic OVF correspond to what low T-score status.
Methods
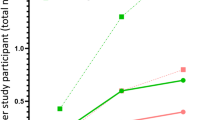
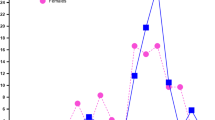
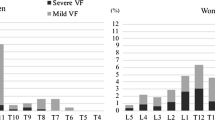
There were age-matched 301 Italian community women and 301 Chinese community women (sub-group A, age, 73.6 ± 6.1 years). In addition, Chinese sub-groups B and C included 110 community women (age, 68.9 ± 5.5 years) and 101 community women (age: 82.2 ± 4.3 years), respectively. For each vertebra in women, a score of 0, − 0.5, − 1, − 1.5, − 2, − 2.5, and − 3 was assigned for no OVF or OVF of < 20%, ≥ 20 ~ 25%, ≥ 25% ~ 1/3, ≥ 1/3 ~ 40%, ≥ 40%–2/3, and ≥ 2/3 vertebral height loss, respectively, OVFss was defined as the summed score of vertebrae T4 to L5. OVFss and T-scores were ranked from the smallest to the largest values.
Results
For the Chinese total group (sub-groups A, B, and C together), OVFss = − 1 corresponded to lowest T-score (lowest T-score of lumbar spine, femoral neck, and total hip) of − 3.4 ~ − 3.2. OVFss ≤ − 1.5 corresponded to femoral neck T-score ≤ − 2.5. OVFss = −1.5 corresponded to a mean femoral neck T-score of − 3.0, − 2.6, and − 2.4, among Chinese sub-groups B, A, and C subjects, respectively. For Italians, all cases with OVFss ≤ − 1 had lowest T-score ≤ − 2.5. For cases with femoral neck T-score = − 2.5, 41.7% had OVFss = − 1.5, and 58.3% had OVFss = − 1.
Conclusion
For older women, statistically OVFss ≤ − 1 suggests this subject is osteoporotic according to lowest T-score. If using femoral neck T-score, OVFss ≤ − 1.5 qualifies osteoporosis diagnosis.





Similar content being viewed by others
References
Siris ES, Genant HK, Laster AJ, Chen P, Misurski DA, Krege JH (2007) Enhanced prediction of fracture risk combining vertebral fracture status and BMD. Osteoporos Int 18:761–770
Johansson L, Sundh D, Magnusson P, Rukmangatharajan K, Mellström D, Nilsson AG, Lorentzon M (2020) Grade 1 vertebral fractures identified by densitometric lateral spine imaging predict incident major osteoporotic fracture independently of clinical risk factors and bone mineral density in older women. J Bone Miner Res 35:1942–1951
Wang YX, Xiao BH, Su Y, Leung JCS, Lam PMS, Kwok TCY (2022) Fine-tuning the cutpoint T-score as an epidemiological index with high specificity for osteoporosis: methodological considerations for the Chinese population. Quant Imaging Med Surg 12:882–885
Wang YX, Xiao BH (2022) Estimations of bone mineral density defined osteoporosis prevalence and cutpoint T-score for defining osteoporosis among older Chinese population: a framework based on relative fragility fracture risks. Quant Imaging Med Surg 12:4346–4360
Wáng YXJ (2022) An update of our understanding of radiographic diagnostics for prevalent osteoporotic vertebral fracture in elderly women. Quant Imaging Med Surg 12:3495–3514
Kadowaki E, Tamaki J, Iki M, Sato Y, Chiba Y, Kajita E, Kagamimori S, Kagawa Y, Yoneshima H (2010) Prevalent vertebral deformity independently increases incident vertebral fracture risk in middle-aged and elderly Japanese women: the Japanese Population-based Osteoporosis (JPOS) Cohort Study. Osteoporos Int 21:1513–1522
Black DM, Arden NK, Palermo L, Pearson J, Cummings SR (1999) Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. J Bone Miner Res 14:821–828
Kanis JA, Adachi JD, Cooper C, Clark P, Cummings SR, Diaz-Curiel M, Harvey N, Hiligsmann M, Papaioannou A, Pierroz DD, Silverman SL, Szulc P, Epidemiology and Quality of Life Working Group of IOF (2013) Standardising the descriptive epidemiology of osteoporosis: recommendations from the Epidemiology and Quality of Life Working Group of IOF. Osteoporos Int 24:2763–4
Kanis JA, Cooper C, Rizzoli R, Reginster JY, Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis (ESCEO) and the Committees of Scientific Advisors and National Societies of the International Osteoporosis Foundation (IOF) (2019) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 30:3–44
Eastell R, Rosen CJ, Black DM, Cheung AM, Murad MH, Shoback D (2019) Pharmacological management of osteoporosis in postmenopausal women: an Endocrine Society* Clinical Practice Guideline. J Clin Endocrinol Metab 104:1595–1622
Sanchez-Rodriguez D, Bergmann P, Body JJ, Cavalier E, Gielen E, Goemaere S, Lapauw B, Laurent MR, Rozenberg S, Honvo G, Beaudart C, Bruyère O (2020) The Belgian Bone Club 2020 guidelines for the management of osteoporosis in postmenopausal women. Maturitas 139:69–89
Nuti R, Brandi ML, Checchia G, Di Munno O, Dominguez L, Falaschi P, Fiore CE, Iolascon G, Maggi S, Michieli R, Migliaccio S, Minisola S, Rossini M, Sessa G, Tarantino U, Toselli A, Isaia GC (2019) Guidelines for the management of osteoporosis and fragility fractures. Intern Emerg Med 14:85–102
(1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser 843:1–129
Fink HA, Milavetz DL, Palermo L, Nevitt MC, Cauley JA, Genant HK, Black DM, Ensrud KE (2005) What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa? J Bone Miner Res 20:1216–1222
Cong E, Walker MD (2014) The Chinese skeleton: insights into microstructure that help to explain the epidemiology of fracture. Bone Res 2:14009
Wáng YXJ, Che-Nordin N, Deng M, Leung JCS, Kwok AWL, He LC, Griffith JF, Kwok TCY, Leung PC (2019) Osteoporotic vertebral deformity with endplate/cortex fracture is associated with higher further vertebral fracture risk: the Ms. OS (Hong Kong) study results. Osteoporos Int 30:897–905
Wáng YXJ, Che-Nordin N, Leung JCS, Man Yu BW, Griffith JF, Kwok TCY (2020) Elderly men have much lower vertebral fracture risk than elderly women even at advanced age: the MrOS and MsOS (Hong Kong) year 14 follow-up radiology results. Arch Osteoporos 15:176
Wáng YXJ, Diacinti D, Leung JCS, Iannacone A, Kripa E, Kwok TCY, Diacinti D (2021) Much lower prevalence and severity of radiographic osteoporotic vertebral fracture in elderly Hong Kong Chinese women than in age-matched Rome Caucasian women: a cross-sectional study. Arch Osteoporos 16:174
Wáng YXJ, Diacinti D, Leung JCS, Iannacone A, Kripa E, Kwok TCY, Diacinti D (2022) Further evidence supports a much lower prevalence of radiographic osteoporotic vertebral fracture in Hong Kong Chinese women than in Italian Caucasian women. Arch Osteoporos 17:13
Johnell O, Kanis JA, Oden A, Johansson H, De Laet C, Delmas P, Eisman JA, Fujiwara S, Kroger H, Mellstrom D, Meunier PJ, Melton LJ 3rd, O’Neill T, Pols H, Reeve J, Silman A, Tenenhouse A (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20:1185–1194
Wáng YXJ, Diacinti D, Yu W, Cheng XG, Nogueira-Barbosa MH, Che-Nordin N, Guglielmi G, Ruiz Santiago F (2020) Semi-quantitative grading and extended semiquantitative grading for osteoporotic vertebral deformity: a radiographic image database for education and calibration. Ann Transl Med 8:398
Wáng YXJ, Santiago FR, Deng M, Nogueira-Barbosa MH (2017) Identifying osteoporotic vertebral endplate and cortex fractures. Quant Imaging Med Surg 7:555–591
Wáng YXJ, Deng M, He LC, Che-Nordin N, Santiago FR (2018) Osteoporotic vertebral endplate and cortex fractures: a pictorial review. J Orthop Translat 15:35–49
Lynn HS, Lau EM, Au B, Leung PC (2005) Bone mineral density reference norms for Hong Kong Chinese. Osteoporos Int 16:1663–1668
Looker AC, Borrud LG, Hughes JP, Fan B, Shepherd JA, Melton LJ 3rd (2012) Lumbar spine and proximal femur bone mineral density, bone mineral content, and bone area: United States, 2005–2008. National Center for Health Statistics. Vital Health Stat 11(251)
Lewiecki EM (2005) Update on bone density testing. Curr Osteoporos Rep 3:136–42
Miller PD, Njeh CF, Jankowski LG, Lenchik L (2002) International Society for Clinical Densitometry Position Development Panel and Scientific Advisory Committee (2002) What are the standards by which bone mass measurement at peripheral skeletal sites should be used in the diagnosis of osteoporosis? J Clin Densitom 5(Suppl):S39-45
Alarkawi D, Bliuc D, Nguyen TV, Eisman JA, Center JR (2016) Contribution of Lumbar Spine BMD to Fracture Risk in Individuals With T-Score Discordance. J Bone Miner Res 31:274–280
Finkelstein JS, Lee ML, Sowers M, Ettinger B, Neer RM, Kelsey JL, Cauley JA, Huang MH, Greendale GA (2002) Ethnic variation in bone density in premenopausal and early perimenopausal women: effects of anthropometric and lifestyle factors. J Clin Endocrinol Metab 87:3057–3067
Walker MD, Liu XS, Zhou B, Agarwal S, Liu G, McMahon DJ, Bilezikian JP, Guo XE (2013) Premenopausal and postmenopausal differences in bone microstructure and mechanical competence in Chinese-American and white women. J Bone Miner Res 28:1308–1318
Wang YXJ, Diacinti D, Griffith JF, Yeung DKW, Iannacone A, Kripa E, Leung JCS, Kwok TCY (2022) Diacinti D (2022) Lumbar L3 marrow fat content in older Italian women is not apparently higher than in older Chinese women. Ann Transl Med 10:648
Zhang X, Dai Z, Lau EHY, Cui C, Lin H, Qi J, Ni W, Zhao L, Lv Q, Gu J, Lin Z (2020) Prevalence of bone mineral density loss and potential risk factors for osteopenia and osteoporosis in rheumatic patients in China: logistic regression and random forest analysis. Ann Transl Med 8:226
Tao Y, Tang S, Huang X, Wang H, Zhou A, Zhang J (2021) Prevalence and risk factors of osteoporosis in Chinese postmenopausal women awaiting total knee arthroplasty. Clin Interv Aging 16:379–387
Wang YXJ (2022) Estimation of osteoporosis prevalence among a population is reasonable only after the concerned reference bone mineral density database and cutpoint T-score have been validated. Osteoporos Int (in press). https://doi.org/10.1007/s00198-022-06538-0
Wu XP, Liao EY, Huang G, Dai RC, Zhang H (2003) A comparison study of the reference curves of bone mineral density at different skeletal sites in native Chinese, Japanese, and American Caucasian women. Calcif Tissue Int 73:122–132
Wáng YXJ, Deng M, Griffith JF, Kwok AWL, Leung JCS, Lam PMS, Yu BWM, Leung PC, Kwok TCY (2022) “Healthier Chinese spine”: an update of osteoporotic fractures in men (MrOS) and in women (MsOS) Hong Kong spine radiograph studies. Quant Imaging Med Surg 12:2090–2105
Masud T, Langley S, Wiltshire P, Doyle DV, Spector TD (1993) Effect of spinal osteophytosis on bone mineral density measurements in vertebral osteoporosis. BMJ 307:172–173
Muraki S, Yamamoto S, Ishibashi H, Horiuchi T, Hosoi T, Orimo H, Nakamura K (2004) Impact of degenerative spinal diseases on bone mineral density of the lumbar spine in elderly women. Osteoporos Int 15:724–728
Pham T, Azulay-Parrado J, Champsaur P, Chagnaud C, Legré V, Lafforgue P (2005) “Occult” osteoporotic vertebral fractures: vertebral body fractures without radiologic collapse. Spine (Phila Pa 1976) 30:2430–5
Kim YJ, Chae SU, Kim GD, Park KH, Lee YS, Lee HY (2013) Radiographic detection of osteoporotic vertebral fracture without collapse. J Bone Metab 20:89–94
Du EZ (2022) Wang YXJ (2002) CT detects more osteoporotic endplate depressions than radiograph: a descriptive comparison of 76 vertebrae. Osteoporos Int 33:1569–1577
Deng M, Kwok TCY, Leung JCS, Leung PC, Wáng YXJ (2018) All osteoporotically deformed vertebrae with >34% height loss have radiographically identifiable endplate/cortex fracture. J Orthop Translat 14:63–66
Wáng YXJ, Liu WH, Diacinti D, Yang DW, Iannacone A, Wang XR, Kripa E, Che-Nordin N, Diacinti D (2020) Diagnosis and grading of radiographic osteoporotic vertebral deformity by general radiologists after a brief self-learning period. J Thorac Dis 12:4702–4710
Lentle BC, Prior JC (2022) Osteoporotic vertebral fracture (OVF): diagnosis requires an informed observer. Osteoporos Int 33:1409–1410
Diacinti D, Vitali C, Gussoni G, Pisani D, Sinigaglia L, Bianchi G, Nuti R, Gennari L, Pederzoli S, Grazzini M, Valerio A, Mazzone A, Nozzoli C, Campanini M, Albanese CV, Research Department of FADOI (2017) Misdiagnosis of vertebral fractures on local radiographic readings of the multicentre POINT (Prevalence of Osteoporosis in INTernal medicine) study. Bone 101:230–235
Kerkeni S, Kolta S, Fechtenbaum J, Roux C (2019) Spinal deformity index (SDI) is a good predictor of incident vertebral fractures. Osteoporos Int 20:1547–1552
Delmas PD, Genant HK, Crans GG, Stock JL, Wong M, Siris E, Adachi JD (2003) Severity of prevalent vertebral fractures and the risk of subsequent vertebral and nonvertebral fractures: results from the MORE trial. Bone 33:522–532
Lunt M, O’Neill TW, Felsenberg D, Reeve J, Kanis JA, Cooper C, Silman AJ, European Prospective Osteoporosis Study Group (2003) Characteristics of a prevalent vertebral deformity predict subsequent vertebral fracture: results From the European Prospective Osteoporosis Study (EPOS). Bone 33:505–13
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
Author YXJ Wáng is the founder of Yingran Medicals Ltd, which develops medical image-based diagnostics software. Authors Davide Diacinti, JCS Leung, A Iannacone, E Kripa, TCY Kwok, and Daniele Diacinti, all declare no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wáng, Y.X.J., Diacinti, D., Leung, J.C.S. et al. Conversion of osteoporotic vertebral fracture severity score to osteoporosis T-score equivalent status: a framework and a comparative study of Hong Kong Chinese and Rome Caucasian older women. Arch Osteoporos 18, 1 (2023). https://doi.org/10.1007/s11657-022-01178-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-022-01178-7