Abstract
Summary
In Spanish primary care (PC), the prevalence of fragility fractures (FF) in subjects ≥ 70 years old is high, especially in women. One-third of subjects with an FF lacked osteoporosis (OP) diagnosis and >50% were not currently receiving OP medication. An improvement of the FF management in this population is needed.
Purpose
In Spanish PC, the prevalence of FF is high, especially in women. One-third of subjects with a FF lacked an OP diagnosis and more than half were not currently receiving OP medication. Several studies reported underdiagnosis/undertreatment of OP in PC among elderly subjects with FF. To date, no such data exist for Spain. The purpose is to estimate the prevalence of FF in the elderly population (≥ 70 years old) and to describe the characteristics, risk factors, comorbidities, and OP diagnosis and treatment rates of subjects with FF in Spanish PC centers.
Methods
This is an observational, retrospective study in Spain consisting of two phases. Phase A included all subjects ≥ 70 years old listed in the center’s medical records from November 2018 to March 2020. Phase B included subjects with FF and prior consultation at the center for any reason. Subjects were excluded only if they had previously participated in another study. Primary outcomes were prevalence of FF (phase A) and characteristics of subjects with at least one FF (phase B).
Results
The overall prevalence of FF was 17.7% among subjects visiting medical centers for any reason (24.1% women vs. 8.0% men) (30 PC centers from 14 Spanish regions). Vertebral (5.1%) was the most prevalent fracture. Of 665 subjects in phase B, most (87%) were women and ≥ 80 years old (57%), suffered mainly major OP fracture (68%), and had multiple comorbidities (≥ 2, 89.2%). While two-thirds had OP diagnosis and 61.1% received OP medication anytime in the past, 56.8% were not currently receiving OP medication. Diagnosis and treatment rates were lower among men (43% and 38% vs. 70% and 65%, respectively).
Conclusion
Prevalence of FF was high, especially in women. One-third of subjects lacked OP diagnosis and ≥ 50% were not receiving OP treatment; diagnosis and treatment gaps were larger among men. This reinforces the need to improve the management of FF in the elderly population. However, as PC centers participating in this study had high OP experience that have the potential to do better in terms of diagnosis and treatment, caution in the generalization of these data should be taken.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The global incidence of osteoporosis (OP) was estimated to be over 200 million in 2020, increasing to 1.55 billion by 2050 [1]. Hence, OP has become a major problem with an enormous health and economic impact [2]. Furthermore, the probability of a fragility fracture increases with age, reaching 40% or more in subjects from Western Europe aged 50 years old [3]. While OP affects both genders, women are at higher risk of fragility fracture than men. In Spain, the probability of a fragility fracture is close to 10% in women with a fracture prior at 65 years old and increases considerably with age from 70 years old onwards [4].
Most of the elderly population with fragility fractures are undiagnosed with OP [5,6,7]. Furthermore, the majority of fragility fractures are not considered to be caused by bone fragility, leading to an underestimation of the true prevalence of fragility fractures [8, 9]. Additionally, the presence of bone fragility is often associated with the absence of symptoms and only one-third of vertebral fractures are symptomatic [10].
Recent studies in Spain indicate that diagnosis and treatment of OP remain suboptimal in subjects with a fragility fracture. In a retrospective study of 161 subjects with hip fracture, 14% of subjects (median age 87 years) were diagnosed with OP and only 7% received OP treatment [11]. Similarly, in a prospective, multicentric study of 487 subjects (mean age 83.1 years), 22% of subjects had a prior non-hip low-trauma fracture, 16% received osteoporotic treatment, and only 3% had densitometry performed [12].
Hence, improved identification and assessment by primary care (PC) is crucial for the management of OP [13, 14]. However, there is still a lack of knowledge when deciding whether to treat or not [15].
There are limited data regarding prevalence of fragility fractures among the elderly population (≥ 70 years) in the Spanish PC setting [16]. In a retrospective study of women indicated for densitometry, incidence of fragility fractures in women without prior fragility fractures ranged from 11/1000 person-years in those <55 years old to 55/1000 person-years in those ≥ 75 years old. The overall prevalence of fragility fractures after a median follow-up of 3.5 years was 7% [17]. Furthermore, there are few data regarding prevention, diagnosis, and treatment of OP in subjects with documented fragility fractures. According to the current National Osteoporosis Foundation [18] and SEIOMM [19] guidelines, all such subjects should be treated with at least one OP therapy. However, few data regarding the degree of compliance with these recommendations in clinical practice exist [14]. The sociodemographic and clinical profile of this population is also unknown.
Our retrospective, observational study aimed to estimate the prevalence of fragility fractures in the elderly population (≥ 70 years old) seen in Spanish PC centers, and to describe the characteristics, risk factors, comorbidities, and OP diagnosis and treatment rates of subjects with fragility fracture.
Methods
Study design
PREFRAOS (the PREvalence of FRAgility fractures and OSteoporosis treatment study) was an observational, retrospective, single-country chart review conducted in 30 Spanish PC centers distributed around Spain in 14 regions (Andalusia, Asturias, Canary Islands, Cantabria, Castilla la Mancha, Castile and Leon, Catalonia, Valencian Community, Estremadura, Galicia, Madrid, Murcia, Navarre, and Basque Country). Centers were chosen from those presenting a physician with a special interest in OP (such as physicians related to bone societies; or OP working groups in PC Societies or attending bone trainings). A previous feasibility study questionnaire was conducted that included information about how much easier the access to the medical records was, how many patients ≥ 70 years old were cared for by the physician, how many had fractures coded, and/or previous experience in observational studies.
The most relevant aspects included in the General Spanish Health Law of 1986 are specified in (1) universal health care. It covers 100% of the population, regardless of their economic situation and their social security affiliation; (2) public financing of assistance through taxes; (3) universal access for all citizens; (4) free benefits at the time of receiving them; and (5) primary health care is the basis of the overall health care system.
In Spain, primary health care services are organized in PC districts that make up territorial demarcations called basic health zones. Primary care centers are located in each basic health area, where PC health care is provided to citizens. Thus, they provide assistance to the entire assigned population. Primary health care in Spain is the gateway to the hospital system. In case of doubt, there is always the possibility to refer the subject to any other specialist (either in the same health center, if available, or to the referral hospital).
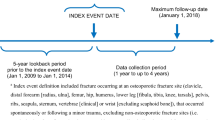
The study comprised two phases (A and B). The objective of phase A was to estimate the prevalence of fragility fractures in the population (women and men) ≥ 70 years old seen in Spanish PC. The objective of phase B was to describe the sociodemographic characteristics, comorbidities, risk factors for fracture, and OP diagnosis and treatment among subjects in phase A who had at least one fragility fracture, and to describe the locations and circumstances of these fractures (related to a fall). The only exclusion criterion was having previously participated in another study. This study was conducted according to the standards of the Declaration of Helsinki principles and its later amendments, and with Good Clinical Practice guidelines. All subjects provided informed consent written or oral before enrolment.
Study population
Phase A included all subjects ≥ 70 years old listed in the investigator’s medical records between November 2018 and March 2020. Phase B included subjects from phase A with a recorded fragility fracture and prior consultation at the center for any reason. Fragility fractures were identified using International Classification of Diseases (ICD) codes (ICD-9 and ICD-10) and/or open fields, according to the characteristics of each center’s database.
At the study level, all centers were included in the study between November 2018 and January 2020 (data collection period). All data were retrospectively collected from subjects’ medical charts. There was no limit for the retrospective index period (i.e., all lifespan data will be reviewed to be able to capture all fragility fractures).
Data collection
For phase A, each center reported the total number of subjects (overall, men, and women) and the total number of subjects ≥ 70 years old (overall, men, and women) listed in the center’s electronic medical records at the time of data collection. For subjects ≥ 70 years old, the center then retrospectively collected the total number with at least one fragility fracture—hip fracture, vertebral fracture, wrist/forearm fracture, and humerus fracture—documented. This allowed calculation of the prevalence of fragility fractures in the PC setting.
For phase B, the following variables were obtained retrospectively from subjects’ medical records: (1) sociodemographic variables: age, gender, education, marital status; (2) risk factors for fracture at the time of data collection (or last information available in the medical records): body mass index (BMI), history of falls, history of parental hip fracture, current smoking, alcohol intake ≥ 3 units/day, rheumatoid arthritis, secondary OP (all diseases considered in the FRAX© tool), and associated medications (oral glucocorticoids, aromatase inhibitors, GnRH analogs, anticonvulsants, proton-pump inhibitors, antihypertensive drugs, and statins); (3) other comorbidities; (4) OP diagnosis; (5) bone mineral density (BMD): if T-score available and last T-score, location; and (6) OP treatments (previous and current). Height measurements were not collected in the subject’s follow-up, so the estimation of putative asymptomatic vertebral fracture occurrence could not be performed. Moreover, information about morphometric vertebral fractures through X-rays at fracture occurrence was also not collected.
All data were retrospectively collected from subjects’ medical charts. There was no limit for the retrospective index period (i.e., all lifespan data will be reviewed to be able to capture all fragility fractures). Subjects lost during the follow-up were not collected as there were no limits for the retrospective index period.
Statistical analysis
All analyses were descriptive. For categorical variables, the frequency and percentage with 95% confidence interval (CI) are presented. For continuous variables, summary statistics included the number of subjects, mean, median, standard deviation (SD) or standard error (SE), 25th percentile (Q1), 75th percentile (Q3), minimum, and maximum. All data analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
In phase A, prevalence of fragility fractures was calculated using the mean number of subjects registered at each PC center in Spain as the denominator. Specifically, we estimated 476 subjects ≥ 70 years old per center (total of 19,040 subjects). This sample size offered a maximum margin of error (minimum precision) of 0.7 with maximum indetermination (p=q=50) for a 95% CI.
In phase B, a sample size of 720 subjects were chosen to offer a maximum margin of error (minimum precision) of 7.3% for categorical variables summarized as percentages. Assuming missing/incomplete data in 10% of subjects, the total sample was estimated to be 800 subjects. Finally, a total of 665 subjects were included in phase B. This sample size did not affect the intended power of the study.
Results
Prevalence of fragility fractures
A total of 30 PC centers from 14 Spanish regions participated in the study. From 44,062 medical records dated between November 2018 and March 2020, 8904 (20.2%) subjects were ≥ 70 years old and eligible for phase A. Of these, 17.7% had a recorded fragility fracture, with prevalence approximately 3-fold higher in women compared with that in men (24.1% vs. 8.0%, respectively) (Fig. 1). Overall, vertebral fracture was the most common OP fracture reported (5.1%) (all vertebral fractures reported in the subject file were collected) (Fig. 2).
Demographic characteristics
Baseline characteristics of subjects included in phase B are described in Table 1. Of the 665 subjects eligible for phase B, most were women (87%) and the majority were aged ≥ 80 years old (56.7%). Mean (SD) BMI was 27.9 (4.8) kg/m2 (normal weight range, 25.0–29.9 kg/m2) [20]. The majority of subjects (70.4%) reported ≥ 4 risk factors for fracture, with history of falls (57.3%) and age ≥ 80 years (56.7%) the most common. Of the most recently reported fragility fractures, major OP fracture (hip, spine, wrist/forearm, or proximal humerus; 68.1%) was the most common.
Other characteristics
Most subjects (90%) had two or more comorbidities, the most common (occurring in ≥ 20% of subjects) being arthrosis (73.7%), hypertension (70.5%), anxiety (33.8%), sleep disorders (31.1%), depression (29.9%), and diabetes (20.8%). Furthermore, 14% of subjects had chronic kidney disease (CKD), of which 44.1% had stage 3A and 31.2% stage 3B (Table 2).
OP diagnosis and treatment
Overall, two-thirds (65.7%) of subjects included in phase B had an OP diagnosis; compared with women, men had lower diagnosis rates (69.7% vs. 42.9%). While 61.1% of all subjects had received OP medication at any time, with the majority (62.1%; Table S1) having received only one OP treatment, more than half of all subjects (56.8%) were not receiving OP treatment at inclusion into phase B (Table 3). This treatment gap was higher among men than that in women (71.4% vs. 54.3%; Table 3). Compared with subjects with an OP diagnosis, the treatment gap was twofold higher in subjects without an OP diagnosis (86.8% vs. 41.2%; Table S2). T-score was available in 41.5% of all subjects, and twice as likely to be available in women than that in men (44.8% [254/567] vs. 22.4% [22/98], respectively).
Fracture characteristics
Among the 665 subjects included in part B, 928 fractures (800 fractures in women and 128 in men) were reported. Overall, the most common fracture type was vertebral (32.9%), with similar incidence among men and women (32% and 33%, respectively), followed by hip/femur (18.8%) and humerus (12.3%). The most common fracture type among women was vertebral (33%) compared with hip/femur among men (36.7%) (Table S3). In most subjects, their fracture was reported to be related to a “fall” (women, 603/800 [75.4%]; men, 98/128 [76.6%)]); mean (SD) age at fracture was comparable for men and women (79.0 [9.6] vs. 76.1 [8.4] years). Mean age of subjects when fragility fractures occurred by type of fracture is shown in Table S4 (the earliest mean age of subjects by type of fracture was observed in forearm and the latest mean age in hip/femur, 69.8 vs. 81.0 years).
Most subjects had a single fracture event recorded (women, 70.2% [398/567]; men, 75.5% [74/98]). Two fractures (independently of the location) were observed in 21.0% (119/567) of women and 19.4% (19/98) of men, three fractures in 6.9% (36/567) and 4.1% (4/98), respectively, and four or more fractures in 1.9% (11/567) and 1.0% (1/98) respectively. In few subjects, two femur fractures were reported.
In 175 subjects with fractures in two or more occasions, the time between the first and the second fracture was longer in women than that in men (median [95% CI]: 3.8 [2.9–4.9] vs. 2.3 [0.4–2.9] years, respectively). The survival curve in subjects aged ≥ 70 years with fractures in two or more occasions (phase B) is shown in Fig. S1.
Pharmacological treatments
Of 661 individual prescriptions for OP medications recorded in phase B, the majority (608/661) were recorded in women. Alendronate was the most commonly prescribed OP medication for both women and men (34.9% and 28.3%), followed by denosumab (26.2% and 28.3%, respectively) (Table 4). Almost half (45.1% [298/661]) of the prescribed OP medication were discontinued, most commonly at the decision of the treating physician (31.9% [95/298]) or the subject (20.8% [62/298]), or due to tolerability issues (19.1% [57/298]).
Hospitalizations due to fragility fractures
Hospital admissions due to fragility fractures were reported in 29.6% (197/665) of subjects, with one hospitalization being the most frequent number (87.8% [173/197]). The most common hospitalization was due to hip/femur fracture (62.9%: 83.8% men vs. 58.8% women) (Table S5). A total of 16 patients had one hospitalization due to vertebral fracture among 230 patients with previous vertebral fracture (7.0%) (data not shown).
Discussion
To our knowledge, this is the first study to report the prevalence of fragility fractures in individuals ≥ 70 years old seen in PC centers across different Spanish regions. We found a high prevalence of fragility fractures, with prevalence 2–3-fold higher in women than that in men and vertebral fracture the most prevalent fracture type.
Among subjects aged ≥ 70 years seen in Spanish PC centers, overall prevalence of fragility fractures was 18%. Few studies have previously reported these data, making direct comparisons with our data challenging. Using radiologic criteria, Díaz-López et al. reported prevalence of vertebral fracture between 17 and 25% in subjects ≥ 50 years from a single Spanish region [21]. In postmenopausal Spanish women aged 50–65 years, Rentero et al. reported a prevalence of 23% [22]. Prevalence of vertebral fracture (5%) in our study was much lower, most likely due to the different methods used to identify fragility fracture. In fact, unlike the study by Díaz-López et al., where the subjects were invited to participate and informed of the performance of X-rays, our study was based on the registry of vertebral fractures, probably related to some type of symptomatology. Besides, our study included other types of fractures. Furthermore, unlike previous studies, our study included both genders and it is well established that fragility fractures are more common in women than in men [23,24,25], mainly due to the sudden estrogen drop at menopause, lower BMD, and bone size [24] and also underdiagnosis of OP in men, who rarely undergo diagnostic tests for OP [26]. When looking at women only, the prevalence of fragility fractures (24%) observed in our study is consistent with that of previous studies from single Spanish regions [21, 27]. Using subjects’ medical records, we found vertebral fracture to be the most common fracture type, with aging and history of falls being important risk factors. These findings are to be expected, as age and history of falls are established risk factors for fragility fractures [17, 18, 28, 29]. Indeed, Díaz-López et al. reported age to be significantly associated with the presence of fracture, with fracture risk doubling with every 10-year increase in age, regardless of gender [21].
Phase B of our study found that one-third of subjects with a fragility fracture did not have a diagnosis of OP, whereas 61.1% received OP treatment at any time and more than half were not receiving any OP treatment at the time of study inclusion. These data confirm the poor management of fragility fractures in the PC setting. Several studies have reported underdiagnosis and undertreatment of OP in subjects with a previous fragility fracture in Spain [9, 13, 30, 31]. Furthermore, in a study of women aged ≥ 70 years at high risk of fragility fracture, seen in PC settings across 8 European countries, McCloskey et al. reported that most of the subjects were not receiving OP treatment and 80% did not have an OP diagnosis [13]. National and international clinical practice guidelines [18, 19] recommend treatment in subjects with fragility fractures (major fractures), regardless of BMD, or a fragility fracture if bone mass is low (osteopenia), and subjects with osteoporotic BMD without fractures. The outcomes of our study reflect the ineffective diagnosis and treatment of fragility fractures in PC. At study inclusion, approximately two-thirds of subjects had established OP; however, more than half were not receiving OP treatment, despite being elderly with high comorbidity burden and a history of previous fractures. Moreover, we found a large discrepancy between subjects who had received OP treatment and subjects who were receiving OP medication at study inclusion, suggesting there is still a high rate of discontinuation of OP medication in the PC setting. Despite differences in the age ranges evaluated, our results are consistent with previous studies. Caeiro et al. reported only 16% of subjects ≥ 65 years old hospitalized for a first hip fracture received treatment for OP at the time of the fracture [30]. Prieto-Alhambra et al. reported only 21% of subjects >50 years old with a fragility hip fracture were prescribed OP treatment at discharge [32]. Moreover, in subjects ≥ 65 years old, treatment rates fell from 29% in 2009 to 16% in 2015 [31]. In a cohort study including data from Catalonia (Spain) from 2005 to 2015, the treatment gap in subjects ≥ 50 years old was 80–88% [14]. Based on the database for pharmaco-epidemiological research in PC 2011, León Vásquez et al. reported 39% of subjects ≥ 60 years old received OP treatment after the fracture [33]. Collectively, these data indicate that management of OP among high-risk subjects seen in PC can be improved.
Our study has some limitations. Due to the observational and retrospective design, there were missing data. Moreover, 2.2–10-fold differences in the prevalence of vertebral fracture have been reported, depending on the radiological criteria [21, 34,35,36]. The ICD codes used in our study could add variability in the observed prevalence. Also, fractures can be asymptomatic [10] and the reported prevalence could be underestimated. Conversely, some fractures may have been incorrectly identified as fragility fractures; however, a recent study of more than 300 fractures coded in subjects aged >50 years old reported that >90% of hip fractures, >87% of vertebral fractures, and >80% of major fractures were fragility/osteoporotic (i.e., not related to high-impact trauma) [29]. Finally, among all PC centers invited to participate in the study, PC centers that accepted to participate were those with interest and/or experience in OP. This is a study bias of the medical center selection that could overestimate the OP diagnosis and biased the characteristic of the subjects including treatment rates compared to PC centers without OP experience. This fact shows that the participating PC centers have the potential to do better in terms of diagnosis and treatment. Moreover, our study included centers from different Spanish regions (specifically, 73.7% of the Spanish regions), providing a representative sample of most of the Spanish regions of subjects ≥ 70 years old (at the time of data collection).
Conclusion
We observed a high prevalence of fragility fractures among the elderly (≥ 70 years) subjects seen in Spanish PC, and a large diagnosis and treatment gap among subjects with a fragility fracture. Compared to women, these gaps were larger in men. Our data highlight the urgent need to improve the management of fragility fractures in PC. As PC centers participating in this study had high OP experience that have the potential to do better in terms of diagnosis and treatment, caution in the generalization of these data should be taken.
Data availability
All data relevant to the study are included in the article or uploaded as supplemental information.
References
Neustadt J (2013) Osteoporosis: beyond bone mineral density to maximize fracture reduction. Anti-Aging Therapeutics - 2012 Conference Year 121–38
Harvey NCW, McCloskey EV, Mitchell PJ, Dawson-Hughes B, Pierroz DD, Reginster J-Y et al (2017 May) Mind the (treatment) gap: a global perspective on current and future strategies for prevention of fragility fractures. Osteoporos Int 28(5):1507–1529
Kanis JA, Johnell O, Oden A, Sembo I, Redlund-Johnell I, Dawson A et al (2000) Long-term risk of osteoporotic fracture in Malmö. Osteoporos Int 11(8):669–674
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster J-Y et al (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24(1):23–57
Bougioukli S, Κollia P, Koromila T, Varitimidis S, Hantes M, Karachalios T et al (2018) Failure in diagnosis and under-treatment of osteoporosis in elderly patients with fragility fractures. J Bone Miner Metab 17:37
Elliot-Gibson V, Bogoch E, Jamal SA, Beaton D (2004) Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: a systematic review. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA 1(15):767–778
Sun M, Zhang Y, Shen H, Sun K, Qi B, Yu C, et al (2020) Prevalence of and risk factors for community-based osteoporosis and associated fractures in Beijing: study protocol for a cross-sectional and prospective study. Front Med [Internet]. 2020 [cited 2021 May 10];7. Available from: https://www.frontiersin.org/articles/https://doi.org/10.3389/fmed.2020.544697/full
Azagra R, Zwart M, Encabo G, Aguyé A, Martin-Sánchez JC, Puchol-Ruiz N et al (2016) Rationale of the Spanish FRAX model in decision-making for predicting osteoporotic fractures: an update of FRIDEX cohort of Spanish women. BMC Musculoskelet Disord 17(17):262
Miller PD (2016) Underdiagnosis and undertreatment of osteoporosis: the battle to be won. J Clin Endocrinol Metab 101(3):852–859
Bottai V, Giannotti S, Raffaetà G, Mazzantini M, Casella F, De Paola G et al (2016) Underdiagnosis of osteoporotic vertebral fractures in patients with fragility fractures: retrospective analysis of over 300 patients. Clin Cases Miner Bone Metab 13(2):119–122
Gómez Navarro R, González García P, Martín Hernández C, Castro Sauras Á, Valdearcos ES (2017) Primary and secondary prevention of hip fragility fracture in Teruel Health Sector, Aragon. Spain. Rev Esp Salud Publica. 2:91
Etxebarria-Foronda I (2016) Cost of hip fracture in Spain: analysis by region of a prospective, observational study (PROA). WCO-IOF-ESCEO. P221.
McCloskey E, Rathi J, Heijmans S, Blagden M, Cortet B, Czerwinski E et al (2021) The osteoporosis treatment gap in patients at risk of fracture in European primary care: a multi-country cross-sectional observational study. Osteoporos Int 32(2):251–259
Skjødt MK, Khalid S, Ernst M, Rubin KH, Martinez-Laguna D, Delmestri A et al (2020) Secular trends in the initiation of therapy in secondary fracture prevention in Europe: a multi-national cohort study including data from Denmark, Catalonia, and the United Kingdom. Osteoporos Int 31(8):1535–1544
Mendis AS, Ganda K, Seibel MJ (2017) Barriers to secondary fracture prevention in primary care. Osteoporos Int 28(10):2913–2919
Pagès-Castellà A, Carbonell-Abella C, Avilés FF, Alzamora M, Baena-Díez JM, Laguna DM et al (2012) Burden of osteoporotic fractures in primary health care in Catalonia (Spain): a population-based study. BMC Musculoskelet Disord 28(13):79
Tebé C, del Río LM, Casas L, Estrada M-D, Kotzeva A, Di Gregorio S et al (2011) Risk factors for fragility fractures in a cohort of Spanish women. Gac Sanit 25(6):507–512
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381
González-Macías J, Del Pino-Montes J, Olmos JM, Nogués X, ennombre de la Comisión de Redacción de las Guías de Osteoporosis de la SEIOMM (2014) Clinical practice guidelines for posmenopausal, glucocorticoid-induced and male osteoporosis. Spanish Society for Research on Bone and Mineral Metabolism (3rd updated version 2014). Rev Clin Esp 215(9):515–26
WHO (2021) Body mass index - BMI [Internet]. [cited 2021 Mar 2]. Available from: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi
Bernardino DíazLópez J, Naves Díaz M, Gómez Alonso C, Luis Fernández Martín J, Rodríguez Rebollar A, CannataAndía JB (2000) Prevalencia de fractura vertebral en población asturiana mayor de 50 años de acuerdo con diferentes criterios radiológicos. Medicina Clínica 115(9):326–31
Luz Rentero M, Carbonell C, Casillas M, González Béjar M, Berenguer R (2008) Risk factors for osteoporosis and fractures in postmenopausal women between 50 and 65 years of age in a primary care setting in Spain: a questionnaire. Open Rheumatol J. 14(2):58–63
Borgström F, Karlsson L, Ortsäter G, Norton N, Halbout P, Cooper C et al (2020) Fragility fractures in Europe: burden, management and opportunities. Arch Osteoporos 15(1):59
Cawthon PM (2011) Gender differences in osteoporosis and fractures. Clin Orthop Relat Res 469(7):1900–1905
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury 37(8):691–697
De Martinis M, Sirufo MM, Polsinelli M, Placidi G, Di Silvestre D, Ginaldi L (2020) Gender differences in osteoporosis: a single-center observational study. World J Mens Health
Sanfélix-Genovés J, Reig-Molla B, Sanfélix-Gimeno G, Peiró S, Graells-Ferrer M, Vega-Martínez M et al (2010) The population-based prevalence of osteoporotic vertebral fracture and densitometric osteoporosis in postmenopausal women over 50 in Valencia, Spain (the FRAVO study). Bone 47(3):610–616
Pisani P, Renna MD, Conversano F, Casciaro E, Di Paola M, Quarta E et al (2016) Major osteoporotic fragility fractures: risk factor updates and societal impact. World J Orthop. 7(3):171–181
Martinez-Laguna D, Soria-Castro A, Carbonell-Abella C, Orozco-López P, Estrada-Laza P, Nogues X et al (2019) Validation of fragility fractures in primary care electronic medical records: a population-based study. Reumatol Clin 15(5):e1-4
Caeiro JR, Bartra A, Mesa-Ramos M, Etxebarría Í, Montejo J, Carpintero P et al (2017) Burden of first osteoporotic hip fracture in Spain: a prospective, 12-month, observational study. Calcif Tissue Int 100(1):29–39
Hurtado I, García-Sempere A, Peiró S, Rodríguez-Bernal C, Sanfélix-Genovés J, Sanfélix-Gimeno G (2020) Trends and geographical variability in osteoporosis treatment after hip fracture: a multilevel analysis of 30,965 patients in the Region of Valencia. Spain. J Bone Miner Res. 35(9):1660–1667
Prieto-Alhambra D, Reyes C, Sainz MS, González-Macías J, Delgado LG, Bouzón CA et al (2018) In-hospital care, complications, and 4-month mortality following a hip or proximal femur fracture: the Spanish registry of osteoporotic femur fractures prospective cohort study. Arch Osteoporos 13(1):96
León Vázquez F, Bonis J, Bryant Cerezo V, Herrero Hernández S, Jamart Sánchez L, Díaz HA (2015) Prevención de fractura osteoporótica en España: uso de fármacos antes y después de una fractura de cadera. Revista de Osteoporosis y Metabolismo Mineral. 7(2):54–62
Smith-Bindman R, Cummings SR, Steiger P, Genant HK (1991) A comparison of morphometric definitions of vertebral fracture. J Bone Miner Res 6(1):25–34
Mann T, Oviatt SK, Wilson D, Nelson D, Orwoll ES (1992) Vertebral deformity in men. J Bone Miner Res 7(11):1259–1265
Adami S, Gatti D, Rossini M, Adamoli A, James G, Girardello S et al (1992) The radiological assessment of vertebral osteoporosis. Bone 13(Suppl 2):S33-36
Acknowledgements
Writing support was provided by Lisa Cadavez, TFS HealthScience S.L., funded by Amgen S.A, and Claire Desborough Amgen (Europe) GmbH.
Funding
This study was sponsored by Amgen S.A.
Author information
Authors and Affiliations
Consortia
Contributions
DML conceived and designed the study and contributed to the quality control and interpretation of the data, to the data collection, and to the drafting and revision of the manuscript. The remaining authors participated in data collection and manuscript review. All the authors have read and agreed to the final published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by each ethics committee assigned to each center.
Consent to participate
Written or oral informed consent was obtained from all subjects before participating in this study.
Conflicts of interest
DML: personal fees from Amgen, Lilly, Rubió, Gedeon Richter, Pierre Fabre, Grünenthal, Theramex, and Italfarmaco; JCB: personal fees from AstraZeneca, Esteve, Boehringer Ingelheim, Bayer, Abbott, Almirall, Amgen, Chiessi, FAES, Grunenthal, GSK, Lilly, Menarini, MSD, Pfizer, Recordatti, Rovi, and Servier; MG: personal fees from Amgen, Stada, Rubió, and Grünenthal; RMP: fees from Amgen, UCB, Stada, Angelini, and Gebro; FV: personal fees from Pfizer, Grünenthal, MSD, Amgen, GSK, Lilly, Bristol-Myers Squibb, Servier, P&G Pharmaceuticals, Novartis, Almirall, Sanofi, and Mundipharma; MB and LC: Amgen employees.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Martínez-Laguna, D., Carbonell, C., Bastida, JC. et al. Prevalence and treatment of fragility fractures in Spanish primary care: PREFRAOS study. Arch Osteoporos 17, 93 (2022). https://doi.org/10.1007/s11657-022-01124-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-022-01124-7