Abstract
Background
Associations between race/ethnicity and medications to treat OUD (MOUD), buprenorphine and methadone, in reproductive-age women have not been thoroughly studied in multi-state samples.
Objective
To evaluate racial/ethnic variation in buprenorphine and methadone receipt and retention in a multi-state U.S. sample of Medicaid-enrolled, reproductive-age women with opioid use disorder (OUD) at the beginning of OUD treatment.
Design
Retrospective cohort study.
Subjects
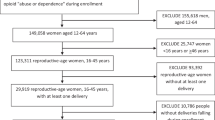
Reproductive-age (18–45 years) women with OUD, in the Merative™ MarketScan® Multi-State Medicaid Database (2011–2016).
Main Measures
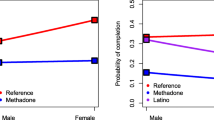
Differences by race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, “other” race/ethnicity) in the likelihood of receiving buprenorphine and methadone during the start of OUD treatment (yes/no) were estimated using multivariable logistic regression. Differences in time to medication discontinuation (days) by race/ethnicity were evaluated using multivariable Cox regression.
Results
Of 66,550 reproductive-age Medicaid enrollees with OUD (84.1% non-Hispanic White, 5.9% non-Hispanic Black, 1.0% Hispanic, 5.3% “other”), 15,313 (23.0%) received buprenorphine and 6290 (9.5%) methadone. Non-Hispanic Black enrollees were less likely to receive buprenorphine (adjusted odds ratio, aOR = 0.76 [0.68–0.84]) and more likely to be referred to methadone clinics (aOR = 1.78 [1.60–2.00]) compared to non-Hispanic White participants. Across both buprenorphine and methadone in unadjusted analyses, the median discontinuation time for non-Hispanic Black enrollees was 123 days compared to 132 days and 141 days for non-Hispanic White and Hispanic enrollees respectively (χ2 = 10.6; P = .01). In adjusted analyses, non-Hispanic Black enrollees experienced greater discontinuation for buprenorphine and methadone (adjusted hazard ratio, aHR = 1.16 [1.08–1.24] and aHR = 1.16 [1.07–1.30] respectively) compared to non-Hispanic White peers. We did not observe differences in buprenorphine or methadone receipt or retention for Hispanic enrollees compared to the non-Hispanic White enrollees.
Conclusions
Our data illustrate inequities between non-Hispanic Black and non-Hispanic White Medicaid enrollees with regard to buprenorphine and methadone utilization in the USA, consistent with literature on the racialized origins of methadone and buprenorphine treatment.



Similar content being viewed by others
References
McLemore MR, Altman MR, Cooper N, Williams S, Rand L, Franck L. Health care experiences of pregnant, birthing and postnatal women of color at risk for preterm birth. Soc Sci Med. 2018;201:127-35. doi:https://doi.org/10.1016/j.socscimed.2018.02.013
Crear-Perry J, Correa-de-Araujo R, Johnson TL, McLemore MR, Neilson E, Wallace M. Social and Structural Determinants of Health Inequities in Maternal Health. J Womens Health. 2021;30(2):230-5. doi:https://doi.org/10.1089/jwh.2020.8882
Schiff DMW EC, Foley B, Applewhite R, Diop H, Goulland L, Gupta M, Hoeppner BB, Peacock-Chambers E, Vilsaint CL, Bernstein JA, Bryant AS. Perinatal Opioid Use Disorder Research, Race, and Racism: A Scoping Review Pediatrics. 2022;149(3). doi:https://doi.org/10.1542/peds.2021-052368
Petersen EE, Davis NL, Goodman D, Cox S, Syverson C, Seed K, et al. Racial/Ethnic Disparities in Pregnancy-Related Deaths - United States, 2007-2016. Mmwr-Morbid Mortal W. 2019;68(35):762-5. doi:DOI https://doi.org/10.15585/mmwr.mm6835a3
Bruzelius E, Martins SS. US Trends in Drug Overdose Mortality Among Pregnant and Postpartum Persons, 2017-2020. JAMA. 2022;328(21):2159-61. doi:https://doi.org/10.1001/jama.2022.17045
American College of Obstetricians and Gynecologists. Committee opinion no.711 summary: opioid use and opioid use disorder in pregnancy. Obstet Gynecol. 2017;130(2):488-9.
Phillippi JC, Schulte R, Bonnet K, Schlundt DD, Cooper WO, Martin PR, et al. Reproductive-Age Women's Experience of Accessing Treatment for Opioid Use Disorder: "We Don't Do That Here". Women Health Iss. 2021;31(5):455-61. doi:https://doi.org/10.1016/j.whi.2021.03.010
Tiako MJN, Friedman A, Culhane J, South E, Meisel ZF. Predictors of Initiation of Medication for Opioid Use Disorder and Retention in Treatment Among US Pregnant Women, 2013-2017. Obstet Gynecol. 2021;137(4):687-94. doi:https://doi.org/10.1097/Aog.0000000000004307
Peeler M, Gupta M, Melvin P, Bryant AS, Diop H, Iverson R, et al. Racial and Ethnic Disparities in Maternal and Infant Outcomes Among Opioid-Exposed Mother Infant Dyads in Massachusetts (2017-2019). Am J Public Health. 2020;110(12):1828-36. doi:https://doi.org/10.2105/Ajph.2020.305888
Schiff DM, Nielsen T, Hoeppner BB, Terplan M, Hansen H, Bernson D, et al. Assessment of Racial and Ethnic Disparities in the Use of Medication to Treat Opioid Use Disorder Among Pregnant Women in Massachusetts. JAMA Netw Open. 2020;3(5):e205734.
Gao YA, Drake C, Krans EE, Chen Q, Jarlenski MP. Explaining Racial-ethnic Disparities in the Receipt of Medication for Opioid Use Disorder During Pregnancy. J Addict Med. 2022. doi:https://doi.org/10.1097/ADM.0000000000000979
Xu KY, Borodovsky JT, Presnall N, Mintz CM, Hartz SM, Bierut LJ, et al. Association Between Benzodiazepine or Z-Drug Prescriptions and Drug-Related Poisonings Among Patients Receiving Buprenorphine Maintenance: A Case-Crossover Analysis. Am J Psychiat. 2021;178(7):651-9. doi:https://doi.org/10.1176/appi.ajp.2020.20081174
Meinhofer A, Williams AR, Johnson P, Schackman BR, Bao Y. Prescribing decisions at buprenorphine treatment initiation: Do they matter for treatment discontinuation and adverse opioid-related events? J Subst Abuse Treat. 2019;105:37-43. doi:https://doi.org/10.1016/j.jsat.2019.07.010
Williams AR, Samples H, Crystal S, Olfson M. Acute Care, Prescription Opioid Use, and Overdose Following Discontinuation of Long-Term Buprenorphine Treatment for Opioid Use Disorder. Am J Psychiat. 2020;177(2):117-24. doi:https://doi.org/10.1176/appi.ajp.2019.19060612
Dong HR, Stringfellow EJ, Russell WA, Bearnot B, Jalali MS. Impact of Alternative Ways to Operationalize Buprenorphine Treatment Duration on Understanding Continuity of Care for Opioid Use Disorder. Int J Mental Health Addict. 2022. doi:https://doi.org/10.1007/s11469-022-00985-w
Brunelli SM, Gagne JJ, Huybrechts KF, Wang SV, Patrick AR, Rothman KJ, et al. Estimation using all available covariate information versus a fixed look-back window for dichotomous covariates. Pharmacoepidem Dr S. 2013;22(5):542-50. doi:https://doi.org/10.1002/pds.3434
Jones HE, Chisolm MS, Jansson LM, Terplan M. Naltrexone in the treatment of opioid-dependent pregnant women: common ground. Addiction. 2013;108(2):255-6. doi:https://doi.org/10.1111/add.12071
Xu KY, Jones HE, Schiff DM, Martin CE, Kelly JC, Carter EB, et al. Initiation and Treatment Discontinuation of Medications for Opioid Use Disorder in Pregnant Compared With Nonpregnant People. Obstet Gynecol. 2023;141(4):845–853. https://doi.org/10.1097/AOG.0000000000005117
Bello JK, Salas J, Grucza R. Preconception health service provision among women with and without substance use disorders. Drug Alcohol Depend. 2022;230:109194. https://doi.org/10.1016/j.drugalcdep.2021.109194
Nead KT, Hinkston CL, Wehner MR. Cautions When Using Race and Ethnicity in Administrative Claims Data Sets. JAMA Health Forum. 2022;3(7):e221812. https://doi.org/10.1001/jamahealthforum.2022.1812
Huang F. Analyzing group level effects with clustered data using Taylor series linearization. Pract Assess Res Eval. 2014;19(13):1–9.
Krawczyk N, Feder KA, Fingerhood MI, Saloner B. Racial and ethnic differences in opioid agonist treatment for opioid use disorder in a US national sample. Drug Alcohol Depen. 2017;178:512-8. doi:https://doi.org/10.1016/j.drugalcdep.2017.06.009
Jackson DS, Tiako MJN, Jordan A. Disparities in Addiction Treatment Learning from the Past to Forge an Equitable Future. Med Clin N Am. 2022;106(1):29-41. doi:https://doi.org/10.1016/j.mcna.2021.08.008
Andraka-Christou B. Addressing Racial And Ethnic Disparities In The Use Of Medications For Opioid Use Disorder. Health Affairs. 2021;40(6):920-7. doi:https://doi.org/10.1377/hlthaff.2020.02261
Hansen H, Roberts S. Two Tiers of Biomedicalization: Methadone, Buprenorphine, and the Racial Politics of Addiction Treatment. In Netherland J, editor, Critical Perspectives on Addiction. 2012. p. 79–102. (Advances in Medical Sociology). https://doi.org/10.1108/S1057-6290(2012)0000014008
Harris J, McElrath K. Methadone as Social Control: Institutionalized Stigma and the Prospect of Recovery. Qual Health Res. 2012;22(6):810-24. doi:https://doi.org/10.1177/1049732311432718
Suarez EA, Huybrechts KF, Straub L, Hernandez-Diaz S, Jones HE, Connery HS, et al. Buprenorphine versus Methadone for Opioid Use Disorder in Pregnancy. N Engl J Med. 2022;387(22):2033-44. doi:https://doi.org/10.1056/NEJMoa2203318
Krans EE, Kim JY, Chen QW, Rothenberger SD, James AE, Kelley D, et al. Outcomes associated with the use of medications for opioid use disorder during pregnancy. Addiction. 2021;116(12):3504-14. doi:https://doi.org/10.1111/add.15582
Wakeman SE, Larochelle MR, Ameli O, Chaisson CE, McPheeters JT, Crown WH, et al. Comparative Effectiveness of Different Treatment Pathways for Opioid Use Disorder. JAMA Netw Open. 2020;3(2):e1920622. https://doi.org/10.1001/jamanetworkopen.2019.20622
Harris RA. Race, Overdose Deaths, and Years of Lost Life. Jama Pediatr. 2022;176(7):729-. doi:https://doi.org/10.1001/jamapediatrics.2022.1171
Austin AE, Durrance CP, Ahrens KA, Chen Q, Hammerslag L, McDuffie MJ, et al. Duration of medication for opioid use disorder during pregnancy and postpartum by race/ethnicity: Results from 6 state Medicaid programs. Drug Alcohol Depend. 2023;247:109868. doi:https://doi.org/10.1016/j.drugalcdep.2023.109868
Martin CE, Scialli A, Terplan M. Unmet substance use disorder treatment need among reproductive age women. Drug Alcohol Depend. 2020;206:107679. doi:https://doi.org/10.1016/j.drugalcdep.2019.107679
Martin CE, Britton E, Shadowen H, Bachireddy C, Harrell A, Zhao X, et al. Disparities in opioid use disorder-related hospital use among postpartum Virginia Medicaid members. J Subst Use Addict Treat. 2023;145:208935. doi:https://doi.org/10.1016/j.josat.2022.208935
Alvidrez JL, Barksdale CL. Perspectives From the National Institutes of Health on Multidimensional Mental Health Disparities Research: A Framework for Advancing the Field. Am J Psychiat. 2022;179(6):417-21. doi:https://doi.org/10.1176/appi.ajp.21100969
Barksdale CL, Perez-Stable E, Gordon J. Innovative Directions to Advance Mental Health Disparities Research. Am J Psychiat. 2022;179(6):397-401. doi:https://doi.org/10.1176/appi.ajp.21100972
Hansen HB, Siegel CE, Case BG, Bertollo DN, DiRocco D, Galanter M. Variation in Use of Buprenorphine and Methadone Treatment by Racial, Ethnic, and Income Characteristics of Residential Social Areas in New York City. J Behav Health Ser R. 2013;40(3):367-77. doi:https://doi.org/10.1007/s11414-013-9341-3
Lagisetty PA, Ross R, Bohnert A, Clay M, Maust DT. Buprenorphine Treatment Divide by Race/Ethnicity and Payment. Jama Psychiat. 2019;76(9):979-81. doi:https://doi.org/10.1001/jamapsychiatry.2019.0876
Hadland SE, Bagley SM, Rodean J, Silverstein M, Levy S, Larochelle MR, et al. Receipt of Timely Addiction Treatment and Association of Early Medication Treatment With Retention in Care Among Youths With Opioid Use Disorder. Jama Pediatr. 2018;172(11):1029-37. doi:https://doi.org/10.1001/jamapediatrics.2018.2143
Foster VA, Harrison JM, Williams CR, Asiodu IV, Ayala S, Getrouw-Moore J, et al. Reimagining Perinatal Mental Health: An Expansive Vision For Structural Change. Health Affairs. 2021;40(10):1592-6. doi:https://doi.org/10.1377/hlthaff.2021.00805
Hansen H, Jordan A, Plough A, Alegria M, Cunningham C, Ostrovsky A. Lessons for the Opioid Crisis-Integrating Social Determinants of Health Into Clinical Care. Am J Public Health. 2022;112:S109-S11. doi:https://doi.org/10.2105/Ajph.2021.306651
Carter EB, Mazzoni SE, Collaborative EW. A paradigm shift to address racial inequities in perinatal healthcare. Am J Obstet Gynecol. 2021;225(1):108-9. doi:https://doi.org/10.1016/j.ajog.2021.04.215
Ickovics JR, Kershaw TS, Westdahl C, Rising SS, Klima C, Reynolds H, et al. Group prenatal care and preterm birth weight: Results from a matched cohort study at public clinics. Obstet Gynecol. 2003;102(5):1051-7. doi:https://doi.org/10.1016/S0029-7844(03)00765-8
Ali MM, Cutler E, Mutter R, Henke RM, O'Brien PL, Pines JM, et al. Opioid Use Disorder and Prescribed Opioid Regimens: Evidence from Commercial and Medicaid Claims, 2005-2015. J Med Toxicol. 2019;15(3):156-68. doi:https://doi.org/10.1007/s13181-019-00715-0
Dunphy CC, Zhang K, Xu LK, Guy GP. Racial-Ethnic Disparities of Buprenorphine and Vivitrol Receipt in Medicaid. Am J Prev Med. 2022;63(5):717-25. doi:https://doi.org/10.1016/j.amepre.2022.05.006
Viano S, Baker DJ. How Administrative Data Collection and Analysis Can Better Reflect Racial and Ethnic Identities. Rev Res Educ. 2020;44:301-31. doi:https://doi.org/10.3102/0091732x20903321
Bird HE, Huhn AS, Dunn KE. Fentanyl Absorption, Distribution, Metabolism, and Excretion: Narrative Review and Clinical Significance Related to Illicitly Manufactured Fentanyl. J Addict Med. 2023. doi:https://doi.org/10.1097/ADM.0000000000001185
Kleinman RA. Comparison of Driving Times to Opioid Treatment Programs and Pharmacies in the US. Jama Psychiat. 2020;77(11):1163-71. doi:https://doi.org/10.1001/jamapsychiatry.2020.1624
Patrick SW, Richards MR, Dupont WD, McNeer E, Buntin MB, Martin PR, et al. Association of Pregnancy and Insurance Status With Treatment Access for Opioid Use Disorder. JAMA Netw Open. 2020;3(8):e2013456. https://doi.org/10.1001/jamanetworkopen.2020.13456
Patrick S, Faherty LJ, Dick AW, Scott TA, Dudley J, Stein BD. Association Among County-Level Economic Factors, Clinician Supply, Metropolitan or Rural Location, and Neonatal Abstinence Syndrome. Jama-J Am Med Assoc. 2019;321(4):385-93. doi:https://doi.org/10.1001/jama.2018.20851
Tiako MJN, Culhane J, South E, Srinivas SK, Meisel ZF. Prevalence and Geographic Distribution of Obstetrician-Gynecologists Who Treat Medicaid Enrollees and Are Trained to Prescribe Buprenorphine. JAMA Netw Open. 2020;3(12):e2029043. https://doi.org/10.1001/jamanetworkopen.2020.29043
Terplan M, Laird HJ, Hand DJ, Wright TE, Premkumar A, Martin CE, et al. Opioid Detoxification During Pregnancy A Systematic Review. Obstet Gynecol. 2018;131(5):803-14. doi:https://doi.org/10.1097/Aog.0000000000002562
Acknowledgements
Nuri Farber MD and the Psychiatry Residency Research Education Program (PRREP) of Washington University; Laura Bierut MD and Patricia Cavazos-Rehg PhD of the K12 Career Development Award Program in Substance Use and Substance Use Disorder at Washington University; Jeremy Goldbach PhD and Kathleen Bucholz PhD of the Transdisciplinary Training in Addictions Research (TranSTAR) T32 Program of Washington University; Matthew Keller MS and John Sahrmann MA from the Center for Administrative Data Research (CADR) of Washington University. In addition, we acknowledge Matt Keller MS, John Sahrmann MS, and Dustin Stwalley MA and the Center for Administrative Data Research (CADR) at Washington University for assistance with data acquisition, management, and storage.
Funding
This project was funded by R21 DA044744 (Richard Grucza/Laura Bierut). Effort for some personnel was supported by grants T32 DA015035 (Kevin Xu, PI: Kathleen Bucholz, Jeremy Goldbach), K12 DA041449 (Kevin Xu, PI: Laura Bierut, Patricia Cavazos-Rehg), R25 MH11247301 (K Xu, PI: Nuri Farber/Ginger Nicol), K23 DA053507 (Caitlin Martin), K23 DA048169 (Davida Schiff), and R01 DA047867 (Hendrée Jones), but these grants did not fund the analyses of the Merative™ MarketScan® Multi-State Medicaid Database data performed by Dr. Xu. CADR is supported in part by the Washington University Institute of Clinical and Translational Sciences via grants UL1 TR002345 (from the National Center for Advancing Translational Sciences of the National Institutes of Health).
Author information
Authors and Affiliations
Contributions
Concept: Xu, Carter, Schiff, Grucza.
Design: Xu, Carter, Schiff, Grucza, Jones, Kelly, Martin, Bierut.
Analysis of data: Xu.
Interpretation of data: Xu, Carter, Schiff, Grucza, Jones, Kelly, Martin, Bierut.
Drafting of manuscript: Xu, Carter, Schiff, Grucza.
Obtained funding: Grucza, Bierut.
Administrative, technical, or material support: Grucza, Bierut.
Critical revision for important intellectual content: Xu, Carter, Schiff, Grucza, Jones, Kelly, Martin, Bierut.
Dr. Kevin Xu was the only individual who had access to the data and the only one to perform analyses. All of the other authors did not have access to the data, although contributed to the interpretation of data.
Corresponding author
Ethics declarations
Conflict of Interest
All authors report no conflicts of interest. LJB is listed as an inventor on US Patent 8080371, ‘Markers for Addiction’, covering use of SNPs in determining the diagnosis, prognosis and treatment of addiction. All other authors declare no financial interests. All authors do not have any financial or non-financial relationships with organizations that may have an interest in our submitted work.
Positionality Statement
The authors acknowledge that their social identities inevitably influence their science. Perinatal substance use disorders is an area that holds special significance for the lead author, as his medical training overlapped with a surge in maternal overdoses during the COVID-19 pandemic, which were concomitant with rollbacks in perinatal health access in Missouri. While the lead author, who identifies as a US Chinese-American male physician-scientist, has had lived experiences of racism, he has not been pregnant, nor has personally suffered from addiction, and seeks to approach this topic area with humility. He has thus worked to build an interdisciplinary team of co-authors with a diverse array of backgrounds and areas of clinical expertise. The majority of authors, including the co-last author, are female scientists. The authors’ academic ranks include full professor, associate professor, assistant professor, and instructor/new faculty member. The institutions where the authors are employed span private universities, public universities, academic medical centers, public safety-net hospitals, and non-profit substance use disorder treatment centers in multiple states. As part of their commitment to rigorous antiracist science, the authors have sought to contextualize their results with conceptual models, cite prior work of scientists from historically marginalized groups, use people-first and affirming language, and thoroughly acknowledge the methodological limitations influencing their race/ethnicity data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ebony B Carter, MD, MPH, and Richard A Grucza, PhD, share co-last authorship.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, K.Y., Schiff, D.M., Jones, H.E. et al. Racial and Ethnic Inequities in Buprenorphine and Methadone Utilization Among Reproductive-Age Women with Opioid Use Disorder: an Analysis of Multi-state Medicaid Claims in the USA. J GEN INTERN MED 38, 3499–3508 (2023). https://doi.org/10.1007/s11606-023-08306-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08306-0