Abstract
Background
The Veterans Health Administration (VA) serves Veterans in the nation’s largest integrated healthcare system. VA seeks to provide high quality of healthcare to Veterans, but due to the VA Choice and MISSION Acts, VA increasingly pays for care outside of its system in the community. This systematic review compares care provided in VA and non-VA settings, and includes published studies from 2015 to 2023, updating 2 prior systematic reviews on this topic.
Methods
We searched PubMed, Web of Science, and PsychINFO from 2015 to 2023 for published literature comparing VA and non-VA care, including VA-paid community care. Records were included at the abstract or full-text level if they compared VA medical care with care provided in other healthcare systems, and included clinical quality, safety, access, patient experience, efficiency (cost), or equity outcomes. Data from included studies was abstracted by two independent reviewers, with disagreements resolved by consensus. Results were synthesized narratively and via graphical evidence maps.
Results
Thirty-seven studies were included after screening 2415 titles. Twelve studies compared VA and VA-paid community care. Most studies assessed clinical quality and safety, and studies of access were second most common. Only six studies assessed patient experience and six assessed cost or efficiency. Clinical quality and safety of VA care was better than or equal to non-VA care in most studies. Patient experience in VA care was better than or equal to experience in non-VA care in all studies, but access and cost/efficiency outcomes were mixed.
Discussion
VA care is consistently as good as or better than non-VA care in terms of clinical quality and safety. Access, cost/efficiency, and patient experience between the two systems are not well studied. Further research is needed on these outcomes and on services widely used by Veterans in VA-paid community care, like physical medicine and rehabilitation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The Veterans Health Administration (VA) is the nation’s largest integrated healthcare system, providing care for millions of U.S. military Veterans. Providing high quality of healthcare is a commitment VA makes to Veterans. Comparisons of VA-delivered care to care delivered in non-VA settings is central to assessing the quality of VA healthcare. Prior reviews conducted in 2011 and 2016 comparing outcomes between VA and non-VA care included data through 2014, and found that VA care performed similarly to or better than non-VA care in most, but not all, aspects of healthcare quality.1,2,3
Since that time concerns about access to care led to the Veteran Access, Choice, and Accountability (“Choice”) Act of 2014, which allowed Veterans to seek medical care in the community if the VA was unable to schedule a visit within 30 days or if the Veteran lived greater than 40 miles from their closest VA. This program also required independent performance assessments of VA’s healthcare services related to access and available expertise.4 Choice Act funding ended in 2017 and was followed by the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act of 2018 that further addressed concerns regarding Veteran access to care by expanding eligibility for VA-reimbursed community care (CC) options.5 These acts greatly expanded the potential for care delivered to Veterans and paid for by VA to be from community providers, raising additional questions about comparisons of the quality of healthcare. Unlike prior studies and reviews of prior studies where subjects sorted into VA or non-VA care due to eligibility or preference, there is now the situation where VA is enabling Veterans eligible for VA care to get care outside of VA – community care – at VA’s expense.
To address these gaps and update the understanding of Veteran care outcomes, we conducted a systematic review to compare clinical quality and safety, access, patient experience and cost between VA and non-VA medical care, with a particular focus on comparisons of the quality of healthcare between VA care and VA-paid community care.
METHODS
This review is part of a larger review commissioned by the Veterans Health Administration detailing differences between healthcare quality of VA and non-VA medical and surgical care.6 The protocol for this larger review was preregistered on PROSPERO (http://www.crd.york.ac.uk/PROSPERO/; registration number [CRD42022314154]).
Data Sources and Searches
We conducted broad searches using terms relating to “Veterans health” and “community health services” or “private sector.” To identify articles relevant to the key questions, a research librarian searched PubMed, Web of Science, and PsychINFO (January 2015 to March 2023). The start date was chosen to match the end date of the most recent review by O’Hanlon, et al.2 Additional citations were identified from hand-searching reference lists and consultation with content experts. We limited the search to published and indexed articles involving human subjects available in the English language. See Supplementary Material 1 for complete search strategy.
Study Selection, Data Abstraction, and Study Quality Assessment
Team members working independently screened the titles of retrieved citations, and titles flagged for potential inclusion were screened by a second team member. All disagreements were reconciled through group discussion. Full-text review was conducted in duplicate by independent team members with any disagreements resolved through discussion. All data abstraction were first completed by one reviewer and then checked by another; disagreements were resolved by consensus or discussion with an additional reviewer. Study selection criteria and data abstraction items are detailed in Supplementary Material 2. The risk of bias for these studies was judged by the representativeness of their samples being assessed and whether the measures of performance in the studies were valid and were applied equally across both study groups. Study quality assessment criteria and categorization are detailed in Supplementary Material 2 and 3.
Synthesis
Studies were summarized by a narrative synthesis. Studies were first classified into one or more Institute of Medicine healthcare quality domains:7 clinical quality and safety, access, patient experience and cost/efficiency. Within domains studies were grouped by clinical condition (cardiovascular, etc.). Studies failing one or more of the above quality criteria were not included in the synthesis (See Supplementary Material 4).
RESULTS
Search Results and Synthesis Overview
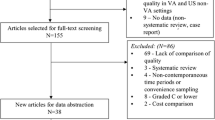
We identified 37 studies8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44 that met inclusion criteria, after successively screening 2415 titles after deduplication from 2448 titles, 183 abstracts, and 113 full-text articles (Fig. 1; full list of excluded studies available in Supplementary Material 4; evidence table in Supplementary Material 5). Our overall results are presented in the bubble plot/evidence maps in Figures 2 and 3. Twelve of these studies compared VA and VA-paid community care.
Evidence map of VA vs. non-VA clinical quality/safety. Notes: Studies are listed on the vertical axis by their qualitative results (VA care is better than community care, VA care and community care are about equal, or results are mixed, and community care is better than VA care). Study quality is depicted by bubble size, with larger bubbles being studies of better quality and representativeness than studies depicted by smaller circles. The color of the bubble indicates the type of comparison: blue for studies comparing Veterans getting care from VA to Veterans getting VA-paid care in the community; orange for studies comparing Veterans getting care from VA and non-Veterans, or a general population, getting care in the community; and, yellow for studies comparing Veterans getting care from VA to Veterans getting care in the community not paid for by VA. Beside each circle is a brief annotation of the study topic, and inside the bubble is the year of publication (’18 = 2018,’19 = 2019, etc.).
Evidence map of VA vs. non-VA access, patient experience, and cost/efficiency. Notes: Studies are listed by domains of care of the outcomes they report by shape: diamonds for access; squares for patient experience; and triangles for cost/efficiency. Studies are also listed on the vertical axis by their qualitative results (VA care is better than community care, VA care and community care are about equal, or results are mixed, and community care is better than VA care). Study quality is depicted by bubble size, with larger bubbles being studies of better quality and representativeness than studies depicted by smaller circles. The color of the bubble indicates the type of comparison: blue for studies comparing Veterans getting care from VA to Veterans getting VA-paid care in the community; orange for studies comparing Veterans getting care from VA and non-Veterans, or a general population, getting care in the community; and, yellow for studies comparing Veterans getting care from VA to Veterans getting care in the community not paid for by VA. Beside each circle is a brief annotation of the study topic, and inside the bubble is the year of publication (’18 = 2018,’19 = 2019, etc.).
Risk of Bias/Study Quality
Twenty-five included studies8,11,12,14,15,16,19,20,21,22,24,25,27,28,30,32,33,35,37,39,40,41,42,43,44 met all our risk of bias criteria. These good quality studies were given more weight in our narrative synthesis than studies that did not meet one or more criterion. Twelve studies9,10,13,17,18,23,26,29,31,34,36,38 met some of our criteria at the middle study quality level, and were categorized as fair study quality (for reasons, see Supplementary Material 3). We included all these studies but gave them less weight when reaching our conclusions. Seven studies were rated at the lowest study quality level for one or more of our criteria, and were excluded from analyses entirely. See Supplementary Material 4 for the excluded studies and Supplementary Material 6 for the risk of bias table.
Clinical Quality and Safety
Twenty-six studies8,9,10,11,12,13,14,17,18,20,24,25,26,27,28,30,31,32,34,36,37,38,39,41,42,43,44 reported clinical quality outcomes. These outcomes were reported in five studies of cardiovascular disease,10,11,26,32,39 three studies of nursing home care,24,25,31 four studies of dialysis and end stage renal disease,9,27,42,43 three studies of mental health conditions,18,38,44 two studies of hospital safety indicators and outpatient clinical quality of care,8,12 two studies of cancer,34,36 two studies of chronic obstructive pulmonary disease,28,41 and five studies of miscellaneous conditions.14,20,37,13,17 Sixteen studies8,11,12,14,20,24,25,27,28,32,37,39,41,42,43,44 were of study good quality, and ten9,10,13,17,18,26,31,34,36,38 were of fair study quality. VA care was better in 15 of these studies,11,12,13,14,17,20,24,25,26,27,28,34,37,42,44 including 5 studies11,25,34,37,42 comparing VA and VA-paid community care. Clinical quality or safety was equal or mixed between VA and non-VA care in 7 studies,8,18,31,32,36,39,43 and worse in VA in 4 studies.9,10,38,41
Cardiovascular Disease Outcomes
We identified five studies, three11,32,39 of good study quality and two10,26 of fair study quality, that compared cardiovascular outcomes. In two studies VA care was better,11,26 in two studies VA and non-VA care was equal or outcomes were mixed,32,39 and in one study VA care was worse.10 Mortality was better for cardiovascular revascularization patients in the only study (VA: n = 15,340; non-VA: n = 3715) comparing VA and VA-paid community care (CC; VA: 0.65% vs. non-VA: 1.54%, p < 0.001).11 Mortality and readmission rates were similar for patients with advanced chronic systolic heart failure in VA and non-VA hospitals, despite VA patients being older and sicker, in an analysis of data from the Beta-blocker Evaluation of Survival Trial (BEST; VA: n = 898; non-VA: n = 1216).26 In two other studies, VA care was similar to non-VA care. An analysis (VA: n = 7929–26,231; non-VA: n = 124,220–269,856) of patients with for acute myocardial infarction (AMI), heart failure (HF), and pneumonia between VA and non-VA hospitals showed that mortality and readmission rates did not consistently favor either system.32 Similar mixed results were reported in a study (VA: n = 35,647; non-VA: n = 9922) of the adequacy of antihypertensive medication supply for dementia patients receiving care by VA or Medicare.39 One study showed that VA care was worse than non-VA care.10 In this study (VA: n = 2242; non-VA: n = 8825), heart failure patients in non-VA care were more likely to experience fewer emergency department visits (odds ratio [OR] 0.62, 95% confidence interval [CI] 0.60–0.64), hospitalizations (OR 0.98, 95% CI 0.95–1.02), and readmissions (OR 0.87, 95% CI 0.83–0.90), compared to patients receiving VA care.
Nursing Home Care Outcomes
Three studies, two24,25 of good and one31 of fair study quality, were included that compared a national sample of clinical quality and safety outcomes in VA Community Living Centers (CLC) versus nursing homes (NH) in the community. Clinical quality was better in VA in two studies,24,25 and equal to non-VA care in another study.31 In one study (VA: n = 23,839; non-VA: n = 1,674,578) using risk-adjusted analyses, patients had lower rates of emergency department visits (VA: 8.27% vs. non-VA: 11.85%, p < 0.001) and higher rates of successful discharges (VA: 67.74% vs. non-VA: 57.04%, p < 0.001) in VA CLCs versus community NHs, but rehospitalization rates were worse in VA (VA: 22.5% vs. non-VA: 21.1%, p < 0.001).24 Results were better in VA in a study (VA: n = 12,660; non-VA: n = 5612) of post-stroke patients in nursing homes: VA CLC patients required and received less rehabilitation therapy, and received more restorative nursing care compared to VA-contracted community NHs.25 Activities to prevent catheter-associated urinary tract infection (CAUTI) were also neither consistently better nor worse in VA in a third study (VA: n = 47 facilities; non-VA: n = 306 facilities) comparing VA CLCs and community NHs.31
Dialysis and end-Stage Renal Disease Outcomes
We also included four studies, three27,42,43 of good study quality and one9 of fair study quality, which compared clinical quality outcomes for Veterans receiving care for end-stage renal disease (ESRD) or for dialysis through the VA or outside the VA. VA clinical quality was better in two studies,27,42 equal in one study,43 and worse in one study.9 In two studies, 2-year mortality was lower in VA care versus non-VA care in the community for ESRD (VA: n = 1100; non-VA: n = 18,215; VA: 32.4% [95% CI 29.2% to 35.4] vs. Medicare: 36.7% [95% CI 36.0% to 37.4%] vs. VA Purchased Care: 36.0% [95% CI 34.0% to 38.0%])42 and pre-ESRD patients (VA: n = 2966; non-VA: n = 2966; VA: 44% vs. Medicare: 53%; adjusted risk difference: 6% [95% CI 4% to 8%]).27 Another study (VA: n = 1101; non-VA: n = 3805 [VA Purchased Care], 18,267 [Medicare]) found that risk of hospitalization after dialysis was similar in VA and non-VA settings (p < 0.0001, but authors noted that the differences found were so small as to not be clinically meaningful).43 In a final study (VA: n = 3663; non-VA: n = 297,794), VA performed worse, as kidney transplantation was less likely for VA patients compared to patients with private insurance (hazard ratio [HR] 0.72, 95% CI 0.68–0.76) or Medicare (HR 0.85, 95% CI 0.81–0.90) receiving non-VA care.9
Mental Health Conditions
We included three national studies, one of good44 and two of fair18,38 study quality, that assessed clinical quality and safety outcomes for Veterans and non-Veterans with mental health conditions. VA clinical quality was better in one study,44 mixed in one study,18 and worse in the last study.38 The good quality study (VA: n = 836,519; non-VA: n = 545,484)44 found better clinical quality of medication treatment among VA-treated patients versus non-VA-treated patients. One fair quality study (VA: n = 303; non-VA: n = 242) found lower depression symptoms and equivalent posttraumatic stress disorder symptoms among Veterans receiving in-person, VA-paid community care, compared to those who received VA tele-mental healthcare.18 The other fair quality study (VA: n = 105 facilities; non-VA: n = 141 facilities) found worse clinical quality of inpatient psychiatric care in VA hospitals compared to non-VA hospitals.38
Hospital Patient Safety Indicators and Outpatient Clinical Quality of Care
We identified two good quality studies that compared a number of clinical quality indicators in inpatient (e.g., death among surgical patients with treatable conditions, pressure ulcers, iatrogenic pneumothorax, etc.) and outpatient (e.g., breast and colorectal cancer screening, blood pressure control among patients with hypertension, eye examination among diabetics, etc.) care.8,12 Both studies assessed national samples for both VA and non-VA care, including more than 100 VA facilities and hundreds or thousands of non-VA facilities. In the first study (VA: n = 129 facilities; non-VA: n = 4010 facilities), clinical quality of inpatient care in VA was better than non-VA care for most measures.12 In the second study (VA: n = 135 facilities; non-VA: n = 402 facilities), VA clinical quality of inpatient and outpatient care was better for many measures, however, VA had higher 30-day risk-standardized readmission rates than non-VA care.8
Cancer Outcomes
Two studies34,36 of cancer care, both of fair quality, also met our inclusion criteria. In the first study34 (VA: n = 235; non-VA: n = 235) of colorectal cancer care, the adenoma detection rate (OR 0.39, 95% CI 0.25 to 0.63) and compliance with surveillance guidelines (OR 0.21, 95% CI 0.09 to 0.45) was worse in non-VA compared to VA. In the second study36 (VA: n = 18,054; non-VA: n = 13,277) of nonsmall long cancer, aggressive care at end of life in some measures declined more significantly in VA (p < 0.001) compared to non-VA from 2006 to 2012. For other measures, there was no difference between systems.
Chronic Obstructive Pulmonary Disease (COPD) Outcomes
Clinical quality outcomes for COPD patients were described in two good quality studies. VA clinical quality was better in the first study28 and worse in the second study.41 Thirty-day readmission rates (VA: 15.3% [95% CI 11.8% to 20.2%] vs. non-VA: 19.5% [95% CI 15.8% to 26.1%]) and mortality rates (VA: 6% [95% CI 3.2% to 10.5%] vs. non-VA 8.5% [95% CI 4.9% to 14.3%]) for COPD patients were significantly lower in VA versus non-VA hospitals in one study (VA: n = 126; non-VA: n = 3523).28 In another study (VA: n = 32,856; non-VA: n = 158,137), VA performed worse, with lower pulmonary rehabilitation rates among VA patients hospitalized for COPD (1.5%) than Medicare beneficiaries with the same condition (2%; p-value not reported.41
Miscellaneous Conditions
We identified for 5 studies, three14,20,37 of good study quality and two13,17 of fair study quality, that reported clinical quality and safety outcomes in miscellaneous conditions. VA clinical quality and safety was better in all studies. In the first study (VA: n = 231,611; non-VA: n = 1,238,546), patients transported by ambulance to an emergency department had lower 30-day mortality per 100 patients in VA hospitals compared to non-VA hospitals (VA: 9.32 [95% 9.15 to 9.50] vs non-VA: 11.67 [95% CI 11.58 to 11.76).14 In the second study (VA: n = 9522; non-VA: n = 17,921), hospitalizations that could have been avoided following chemotherapy were higher among Veterans receiving care through Medicare than through VA (OR 1.58, 95% CI 1.41–1.78).20 VA care was also better than non-VA care in a study (VA: n = 35,647; non-VA: n = 9922) analyzing measures of diabetes control17 and in a study (VA: n = 256,608; non-VA: n = 2005) of possibly inappropriate neuroimaging studies in patients presenting with headache or neuropathy.13 In the last study (VA: n = 6775; non-VA: n = 3423),37 Veterans completed genetic consultations they were referred for less often in VA-paid community care (OR 0.43, 95% CI 0.28 to 0.65), compared to VA care. Patients who had VA-paid community care genetic consultations were also less likely to receive follow up cancer surveillance and risk-reducing procedures (OR 0.64, 95% CI 0.52 to 0.78) than patients in VA care.
Access
Eleven studies9,11,15,16,18,21,22,29,33,34,40 reported outcomes related to access. Five of these studies described wait times,16,21,22,33,34 three listed different patient-reported access outcomes,15,18,40 two reported distance to VA or non-VA facilities,8,10 and one noted self-reported delays in care.28 Seven11,15,16,21,22,33,40 of these studies were of good study quality, while four9,18,29,34 were of fair study quality. In four of these studies,16,21,22,33 three of which compared VA and VA-paid community care,16,21,22 VA access was better. In three other studies,15,18,40 access was equal in VA and non-VA care, and in four studies,9,11,29,34 access in VA was worse.
Wait Times
Four good quality studies16,21,22,33 and one fair quality study34 evaluated wait times in various primary and specialty care settings. VA wait times were better or improved more in four studies,16,21,22,33 and were worse in one study.34 In the first study (VA: n = 15–30 metropolitan areas; non-VA: n = 15–30 metropolitan areas),33 wait times for outpatient primary care, dermatology, cardiology, and orthopedics visits in VA decreased from a mean of 22.5 days (SD 7.3 days) in 2014 to 17.6 days (SD 4.9 days; p = 0.046) in 2017, to be shorter than private sector wait times in that year (p < 0.001). Mean private sector wait times of 18.7 days (standard deviation [SD] 7.9 days) in 2014, which were nonsignificantly shorter than VA wait times during that year, increased by a nonsignificant amount (4.8 days [SD 5.2 days]; p-value not reported) from 2014 to 2017. In the second study (VA: n = 420,590–487,014; non-VA: n = 76,706–150,429), wait times between fiscal year (FY) 2015 and FY 2018 for outpatient physical therapy, optometry, orthopedics, and dental care declined more significantly for VA care compared to VA-paid community care for urban and rural Veterans.22 Cardiology wait times declined at the same rate in both systems. In the third study (VA: n = 2,504,355; non-VA: n = 533,609), overall wait times in outpatient cardiology, gastroenterology, orthopedics, and urology between 2018 and 2019 were lower in VA care compared to VA-paid Choice care (VA 41.1, SD 15.9 days vs non-VA 49.0, SD 15.5 days; p-value not reported).21 In the fourth study (VA: n = 4,016,156; non-VA: n = 3,042,060),16 wait times from 2018 to 2021 were shorter in adjusted analyses were lower in VA care compared to VA-paid community care in 15 of 18 VISNs for primary care, in 16 of 18 VISNs for mental health care, and in 17 of 18 VISNs for all other specialty care (p-values not reported). In the last study (VA: n = 235; non-VA: n = 235),34 time to colonoscopy was significantly longer in VA (83.8 days, 95% CI 45.2 to 122.4), compared to VA-paid community care (58.4 days, 95% CI 24.7 to 92.1 days; p < 0.0001).
Patient-Reported Access Outcomes
Patient-reported access to care was mixed in two good quality studies,15,40 and one fair quality study.18 VA and VA-paid CC patients, in one study (VA: n = 29,095–432,218; non-VA: n = 29,095–432,218), rated access to specialty care as better in the second quarter of 2016, but no different for primary and mental health care, and ratings for all three care types did not differ over time between VA and VA-paid CC by the fourth quarter of 2017.40 In a second analysis (VA: n = 1,019,732; non-VA: n = 63,638), rural Veterans reported better satisfaction with access to care in FY16 and FY19 in VA compared to VA-paid CC, but satisfaction with access to specialty care was similar between groups. Urban Veterans reported worse satisfaction with access to VA care in both years.15 In the last analysis (VA: n = 303; non-VA: n = 242), VA patients reported more access-related barriers to mental health care compared to patients receiving VA-paid community care (p < 0.001).18
Other Access Outcomes
A good quality study,11 and two fair quality studies9,29 reported other access outcomes. VA access was worse in all three studies.9,11,29 Authors of the first study (VA: n = 15,340; non-VA: n = 3715)11 found that VA patients traveled farther than CC patients for both percutaneous coronary intervention (PCI; VA: 90.8 miles vs. non-VA: 60.1 miles; p < 0.001) and coronary artery bypass graft (CABG; VA: 123.2 miles vs. non-VA: 81.5 miles; p = 0.02). Patients also incurred higher travel costs in VA for both PCI (VA: $238 vs. non-VA: $198; p = 0.004) and CABG (VA: $958 vs. non-VA: $630; p < 0.001). The second (VA: n = 3663; non-VA: n = 297,794) and third (VA: n = 203; non-VA: n = 10,719) studies, VA patients lived farther away from kidney transplant centers than patients using Medicare or private insurance,9 and were more likely to report delays in seeking care than patients using Medicare, Medicaid, or commercial insurance.29
Patient Experience
Six studies8,12,15,18,23,40 reported patient experience outcomes. Two studies15,40 described ratings of providers, three studies8,12,18 reported various patient experience measures, and another23 reported Yelp ratings of hospitals. Four8,12,15,40 of these studies were good quality, and two18,23 were of fair quality. Patient experience between VA and non-VA care was equal or mixed in four studies.8,12,18,23 VA patient experience was better in two studies,15,40 both of which compared VA to VA-paid community care.
The first study (VA: n = 29,095–432,218; non-VA: n = 29,095–432,218) reported that provider ratings for primary, specialty, and mental health care were higher for patients in VA care compared to those in VA-paid CC care.40 These ratings did not change over time. Rural and urban Veterans in another study (VA: n = 1,019,732; non-VA: n = 63,638) also rated providers in primary and specialty care in VA more highly than providers in VA-paid CC care during both FY16 and FY19.15 Ratings of VA and non-VA hospitals were mixed in a third study (VA: n = 135 facilities; non-VA: n = 402 facilities), with non-VA hospitals receiving higher scores for hospital quietness, pain management, responsiveness of hospital staff, and communication with doctors or nurses, and VA hospitals being rated higher for communication about medicine, hospital cleanliness, and care transitions.8 The fourth study (VA: n = 129 facilities; non-VA: n = 4010 facilities), which assessed national samples of VA and non-VA hospitals, also reported mixed results. Some patient experience domains were better in non-VA care, but there was no difference for other domains.12 In the fifth study (VA: n = 303; non-VA; n = 242), patient centeredness was not different (p = 0.243) between VA tele-mental healthcare and VA-paid, in-person mental healthcare in the community.18 In the last study (VA: n = 39 facilities; non-VA: n = 39 facilities), VA and non-VA university affiliate Yelp ratings did not differ after adjustment for bed size, teaching hospital and graduate medical education status, and The Joint Commission certification.23
Cost/Efficiency
We identified 6 studies reporting on efficiency or cost outcomes: one study analyzed patients with cardiac disease,11 one study examined imaging in patients with prostate cancer,30 one study investigated end-of-life care,19 one study looked at patients undergoing dialysis,43 another study analyzed low-value prostate-specific antigen testing (PSA),35 and the last study examined in-person and tele-mental healthcare.18 Five studies were of good quality,11,19,30,35,43 and one was of fair quality.18 Cost/efficiency in VA care was equal or mixed to non-VA care in four studies,11,18,19,43 and better in two studies.30,35
In the first study (VA: n = 15,340; non-VA: n = 3715), costs were lower in VA than in VA-paid community care for patients receiving PCI (VA: $15,683 vs. non-VA: $22,025; p < 0.001) but higher in VA than VA-paid CC for patients receiving CABG (VA: $63,144 vs. non-VA: $55,526; p < 0.01).11 In a study (VA: n = 27,811; non-VA: n = 56,671) of low-risk prostate cancer patients, those receiving care in VA were less likely to receive guideline-discordant imaging (relative risk 0.79, 95% CI 0.67, 0.92) compared to those receiving care paid by Medicare.30 In the third study (VA: n = 10,341; non-VA: n = 18,542), dually enrolled cancer patients had similar costs of care no matter if they were either Medicare- or VA-reliant.19 In the fourth study (VA: n = 1101; non-VA: n = 3805 [VA Purchased Care], 18,267 [Medicare]), days of hospitalization after dialysis were similar in VA and non-VA settings.43 In the fifth study (VA: n = 36,469; non-VA: n = 17,981), low-value PSA testing was associated with 9.9 fewer downstream services per 100 Veterans (95% CI 9.7 to 10.1) and $11.9 less spending per Veteran, (95% CI $7.6 to $16.2) in VA compared to non-VA care.35 In the last study (VA: n = 303; non-VA; n = 242), the numbers of encounters did not significantly differ (p = 0.276) between patients receiving VA tele-mental healthcare or VA-paid, in-person mental healthcare in the community.18
Equity
We did not find any studies reporting on equity outcomes.
DISCUSSION
Our systematic review identified 37 studies comparing clinical quality, safety, access, patient experience, or efficiency/cost between VA delivered care and non-VA delivered care. The large majority of studies assessed clinical quality and safety; followed by comparisons of access to care. Few studies, only 6 in each category, assessed patient experience or cost/efficiency. We found no studies comparing VA to non-VA care on equity. In the domain of clinical quality and safety, the great majority of studies found that VA care is as good as, or better than, care in the community. For the domains of access and of cost/efficiency, VA care was not consistently better or worse than non-VA care. The few studies of patient experience found that VA care and non-VA were not consistently different, but VA care was never worse.
The studies best able to address implications of the Choice and MISSION acts were designed to capture data of Veterans receiving VA-paid community care. In these comparisons, clinical quality and safety was generally better in VA-delivered care. Differences between sites of care were more mixed for the other domains – access, patient experience, and cost.
Key among the clinical quality and safety outcomes is mortality. In studies of cardiac revascularization,11 ESRD42 and pre-ESRD27 dialysis, COPD,28 and ambulance rides to emergency departments,14 mortality was lower in VA care. In the two other studies with this outcome, mortality did not differ between VA and non-VA care.
The overarching conclusion from the published studies since 2015 reinforce the conclusions of the two prior reviews1,2 of studies comparing VA care to non-VA care: on average, VA care performs better than or similar to non-VA care in the domain of clinical quality and safety. This review expands those earlier conclusions to include the healthcare quality domain of access, and combined with studies from the 2016 review can now also make early conclusions on patient experience and efficiency/cost. In each of these domains of access, patient experience, and cost/efficiency, comparative results of performance are more mixed than in the domain of quality/safety, however in the domain of patient experience VA care was never worse.
Limitations
Beyond the usual limitation of any systematic review, the quantity and quality of the original studies, we had several additional limitations. First, there was the possibility of publication bias or subconscious investigator bias, as most of the published studies were written by VA authors. We scrutinized each study for objective evidence of bias to diminish the contribution of such bias to our overall conclusions. Second, there was the possibility of confounding by patient populations in VA or non-VA care. Studies attempted to control for this through multivariable methods (e.g., Chan 202214 had robust controls and concluded that post-ambulance care had lower mortality in VA), but VA patients generally have worse, unmeasured social determinants of health45,46 than those in the community, so included studies may favor non-VA care. Finally, we were limited by how different stakeholders may value our included outcomes. We did not attempt to rank different outcomes (e.g., wait times or provider ratings) by importance, as this assessment could differ by stakeholder.
Future Research
Despite several dozen publications comparing VA care with non-VA care, there are several clinical areas utilized heavily in the community via the MISSION Act, such as physical medicine and rehabilitation, that are not represented in the literature. In addition, it would greatly facilitate comparisons of VA care to non-VA care if non-VA care had the same degree of comprehensive performance data that are publicly available. Lastly, we expect that this topic is a moving target, and thus this review needs regular updating of published studies to remain up to date.
CONCLUSION
In general, most published studies of comparisons of healthcare quality show that Veterans getting care from VA get the same or better clinical quality than Veterans getting community care or the general public getting non-VA care.
Data Availability
The data supporting the findings of this study are available within the article and its supplementary material.
References
Trivedi AN, Matula S, Miake-Lye I, Glassman PA, Shekelle P, Asch S. Systematic review: comparison of the quality of medical care in Veterans Affairs and non-Veterans Affairs settings. Med Care. 2011;49(1):76-88.https://doi.org/10.1097/MLR.0b013e3181f53575
O'Hanlon C, Huang C, Sloss E, et al. Comparing VA and Non-VA Quality of Care: A Systematic Review. J Gen Intern Med. 2017;32(1):105-121.https://doi.org/10.1007/s11606-016-3775-2
Baker A. Crossing the Quality Chasm: A New Health System for the 21st Century. vol 323(7322). BMJ; 2011.
Veterans Access, Choice, and Accountability Act of 2014, (2014).
VA MISSON Act of 2018, (2018).
Shekelle P M-GM, Blegen M, et al. VA versus Non-VA Quality of Care: A Systematic Review. . Vol. VA ESP Project #05–226;. 2022.
Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academies Press; 2001.
Anhang Price R, Sloss EM, Cefalu M, Farmer CM, Hussey PS. Comparing Quality of Care in Veterans Affairs and Non-Veterans Affairs Settings. J Gen Intern Med. 2018;33(10):1631-1638.https://doi.org/10.1007/s11606-018-4433-7
Augustine JJ, Arrigain S, Balabhadrapatruni K, Desai N, Schold JD. Significantly Lower Rates of Kidney Transplantation among Candidates Listed with the Veterans Administration: A National and Local Comparison. J Am Soc Nephrol. 2018;29(10):2574-2582.https://doi.org/10.1681/asn.2017111204
Axon RN, Gebregziabher M, Everett CJ, Heidenreich P, Hunt KJ. Dual health care system use is associated with higher rates of hospitalization and hospital readmission among veterans with heart failure. Am Heart J. 2016;174:157-63.https://doi.org/10.1016/j.ahj.2015.09.023
Barnett PG, Hong JS, Carey E, Grunwald GK, Joynt Maddox K, Maddox TM. Comparison of Accessibility, Cost, and Quality of Elective Coronary Revascularization Between Veterans Affairs and Community Care Hospitals. JAMA Cardiol. 2018;3(2):133-141.https://doi.org/10.1001/jamacardio.2017.4843
Blay E, Jr., DeLancey JO, Hewitt DB, Chung JW, Bilimoria KY. Initial Public Reporting of Quality at Veterans Affairs vs Non-Veterans Affairs Hospitals. JAMA Intern Med. 2017;177(6):882-885.https://doi.org/10.1001/jamainternmed.2017.0605
Burke JF, Kerr EA, McCammon RJ, Holleman R, Langa KM, Callaghan BC. Neuroimaging overuse is more common in Medicare compared with the VA. Neurology. 2016;87(8):792-8.https://doi.org/10.1212/wnl.0000000000002963
Chan DC, Danesh K, Costantini S, Card D, Taylor L, Studdert DM. Mortality among US veterans after emergency visits to Veterans Affairs and other hospitals: retrospective cohort study. BMJ. 2022;376:e068099.https://doi.org/10.1136/bmj-2021-068099
Davila H, Rosen AK, Beilstein-Wedel E, Shwartz M, Chatelain L, Jr., Gurewich D. Rural Veterans' Experiences With Outpatient Care in the Veterans Health Administration Versus Community Care. Med Care. 2021;59(Suppl 3):S286-S291.https://doi.org/10.1097/MLR.0000000000001552
Feyman Y, Asfaw DA, Griffith KN. Geographic Variation in Appointment Wait Times for US Military Veterans. JAMA Netw Open. 2022;5(8):e2228783.https://doi.org/10.1001/jamanetworkopen.2022.28783
Florez HJ, Ghosh A, Pop-Busui R, et al. Differences in complications, cardiovascular risk factor, and diabetes management among participants enrolled at veterans affairs (VA) and non-VA medical centers in the glycemia reduction approaches in diabetes: A comparative effectiveness study (GRADE). Diabetes Res Clin Pract. 2021;184:109188.https://doi.org/10.1016/j.diabres.2021.109188
Fortney JC, Carey EP, Rajan S, Rise PJ, Gunzburger EC, Felker BL. A comparison of patient-reported mental health outcomes for the Department of Veterans Affairs' regional telehealth and Community Care Programs. Health Serv Res. 2022;57(4):755-763.https://doi.org/10.1111/1475-6773.13993
Gidwani R, Asch SM, Needleman J, et al. End-of-Life Cost Trajectories in Cancer Patients Treated by Medicare versus the Veterans Health Administration. J Am Geriatr Soc. 2021;69(4):916-923.https://doi.org/10.1111/jgs.16941
Gidwani-Marszowski R, Faricy-Anderson K, Asch SM, Illarmo S, Ananth L, Patel MI. Potentially avoidable hospitalizations after chemotherapy: Differences across medicare and the Veterans Health Administration. Cancer. 2020;126(14):3297-3302.https://doi.org/10.1002/cncr.32896
Griffith KN, Ndugga NJ, Pizer SD. Appointment Wait Times for Specialty Care in Veterans Health Administration Facilities vs Community Medical Centers. JAMA Netw Open. 2020;3(8):e2014313.https://doi.org/10.1001/jamanetworkopen.2020.14313
Gurewich D, Shwartz M, Beilstein-Wedel E, Davila H, Rosen AK. Did Access to Care Improve Since Passage of the Veterans Choice Act?: Differences Between Rural and Urban Veterans. Med Care. 2021;59(Suppl 3):S270-S278. https://doi.org/10.1097/MLR.0000000000001490
Heidenreich PA, Zapata A, Shieh L, Oliva N, Sahay A. Patient ratings of Veterans Affairs and affiliated hospitals. Am J Manag Care. 2017;23(6):382-384.
Intrator O, O'Hanlon CE, Makineni R, Scott WJ, Saliba D. Comparing Post-Acute Populations and Care in Veterans Affairs and Community Nursing Homes. J Am Med Dir Assoc. 2021;22(12):2425-2431.e7. https://doi.org/10.1016/j.jamda.2021.10.007
Jia H, Pei Q, Sullivan CT, et al. Poststroke Rehabilitation and Restorative Care Utilization: A Comparison Between VA Community Living Centers and VA-contracted Community Nursing Homes. Med Care. 2016;54(3):235-42.https://doi.org/10.1097/mlr.0000000000000494
Jones LG, Sin MK, Hage FG, et al. Characteristics and outcomes of patients with advanced chronic systolic heart failure receiving care at the Veterans Affairs versus other hospitals: insights from the Beta-blocker Evaluation of Survival Trial (BEST). Circ Heart Fail. 2015;8(1):17-24.https://doi.org/10.1161/circheartfailure.114.001300
Kurella Tamura M, Thomas IC, Montez-Rath ME, et al. Dialysis Initiation and Mortality Among Older Veterans With Kidney Failure Treated in Medicare vs the Department of Veterans Affairs. JAMA Intern Med. 2018;178(5):657-664.https://doi.org/10.1001/jamainternmed.2018.0411
LaBedz SL, Krishnan JA, Chung YC, et al. Chronic Obstructive Pulmonary Disease Outcomes at Veterans Affairs Versus Non-Veterans Affairs Hospitals. Chronic Obstr Pulm Dis. 2021;8(3):306-313.https://doi.org/10.15326/jcopdf.2021.0201
Lee D, Begley CE. Delays in Seeking Health Care: Comparison of Veterans and the General Population. J Public Health Manag Pract. 2017;23(2):160-168.https://doi.org/10.1097/phh.0000000000000420
Makarov DV, Ciprut S, Walter D, et al. Association Between Guideline-Discordant Prostate Cancer Imaging Rates and Health Care Service Among Veterans and Medicare Recipients. JAMA Netw Open. 2018;1(4):e181172.https://doi.org/10.1001/jamanetworkopen.2018.1172
Mody L, Greene MT, Saint S, et al. Comparing Catheter-Associated Urinary Tract Infection Prevention Programs Between Veterans Affairs Nursing Homes and Non-Veterans Affairs Nursing Homes. Infect Control Hosp Epidemiol. 2017;38(3):287-293.https://doi.org/10.1017/ice.2016.279
Nuti SV, Qin L, Rumsfeld JS, et al. Association of Admission to Veterans Affairs Hospitals vs Non-Veterans Affairs Hospitals With Mortality and Readmission Rates Among Older Men Hospitalized With Acute Myocardial Infarction, Heart Failure, or Pneumonia. JAMA. 2016;315(6):582-92.https://doi.org/10.1001/jama.2016.0278
Penn M, Bhatnagar S, Kuy S, et al. Comparison of Wait Times for New Patients Between the Private Sector and United States Department of Veterans Affairs Medical Centers. JAMA Netw Open. 2019;2(1):e187096. https://doi.org/10.1001/jamanetworkopen.2018.7096
Petros V, Tsambikos E, Madhoun M, Tierney WM. Impact of Community Referral on Colonoscopy Quality Metrics in a Veterans Affairs Medical Center. Clin Transl Gastroenterol. 2022;13(3):e00460.https://doi.org/10.14309/ctg.0000000000000460
Pickering AN, Zhao X, Sileanu FE, et al. Assessment of Care Cascades Following Low-Value Prostate-Specific Antigen Testing Among Veterans Dually Enrolled in the US Veterans Health Administration and Medicare Systems. JAMA Netw Open. 2022;5(12):e2247180. https://doi.org/10.1001/jamanetworkopen.2022.47180
Presley CJ, Kaur K, Han L, et al. Aggressive End-of-Life Care in the Veterans Health Administration versus Fee-for-Service Medicare among Patients with Advanced Lung Cancer. J Palliat Med. 2022;25(6):932-939. https://doi.org/10.1089/jpm.2021.0436
Scheuner MT, Huynh AK, Chanfreau-Coffinier C, et al. Demographic Differences Among US Department of Veterans Affairs Patients Referred for Genetic Consultation to a Centralized VA Telehealth Program, VA Medical Centers, or the Community. JAMA Netw Open. 2022;5(4):e226687.https://doi.org/10.1001/jamanetworkopen.2022.6687
Shields MC, Rosenthal MB. Quality of Inpatient Psychiatric Care at VA, Other Government, Nonprofit, and For-Profit Hospitals: A Comparison. Psychiatr Serv. 2017;68(3):225-230. https://doi.org/10.1176/appi.ps.201600074
Thorpe CT, Gellad WF, Mor MK, et al. Effect of Dual Use of Veterans Affairs and Medicare Part D Drug Benefits on Antihypertensive Medication Supply in a National Cohort of Veterans with Dementia. Health Serv Res. 2018;53 Suppl 3(Suppl Suppl 3):5375–5401. https://doi.org/10.1111/1475-6773.13055
Vanneman ME, Wagner TH, Shwartz M, et al. Veterans' Experiences With Outpatient Care: Comparing The Veterans Affairs System With Community-Based Care. Health Aff (Millwood). 2020;39(8):1368-1376. https://doi.org/10.1377/hlthaff.2019.01375
Vercammen-Grandjean C, Schopfer DW, Zhang N, Whooley MA. Participation in Pulmonary Rehabilitation by Veterans Health Administration and Medicare Beneficiaries After Hospitalization for Chronic Obstructive Pulmonary Disease. J Cardiopulm Rehabil Prev. 2018;38(6):406-410. https://doi.org/10.1097/hcr.0000000000000357
Wang V, Coffman CJ, Stechuchak KM, et al. Survival among Veterans Obtaining Dialysis in VA and Non-VA Settings. J Am Soc Nephrol. 2019;30(1):159-168. https://doi.org/10.1681/asn.2018050521
Wang V, Coffman CJ, Stechuchak KM, et al. Comparative Assessment of Utilization and Hospital Outcomes of Veterans Receiving VA and Non-VA Outpatient Dialysis. Health Serv Res. 2018;53 Suppl 3(Suppl Suppl 3):5309–5330. https://doi.org/10.1111/1475-6773.13022
Watkins KE, Smith B, Akincigil A, et al. The Quality of Medication Treatment for Mental Disorders in the Department of Veterans Affairs and in Private-Sector Plans. Psychiatr Serv. 2016;67(4):391-6. https://doi.org/10.1176/appi.ps.201400537
Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252-7. https://doi.org/10.1001/archinte.160.21.3252
Duan-Porter W, Martinson BC, Greer N, et al. Evidence Review-Social Determinants of Health for Veterans. J Gen Intern Med. 2018;33(10):1785-1795.https://doi.org/10.1007/s11606-018-4566-8
Funding
This project was funded by the Veterans Health Administration Quality Enhancement Research Initiative (Project #ESP 05-226). Open access funding was provided by SCELC, the Statewide California Electronic Library Consortium.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Disclaimer
The views expressed are those of the authors and do not represent the views of the US Department of Veterans Affairs or the United States Government.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Apaydin, E.A., Paige, N.M., Begashaw, M.M. et al. Veterans Health Administration (VA) vs. Non-VA Healthcare Quality: A Systematic Review. J GEN INTERN MED 38, 2179–2188 (2023). https://doi.org/10.1007/s11606-023-08207-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08207-2