Abstract
Background
Most medical schools offer medical Spanish education to teach patient-physician communication skills with the growing Spanish-speaking population. Medical Spanish courses that lack basic standards of curricular structure, faculty educators, learner assessment, and institutional credit may increase student confidence without sufficiently improving skills, inadvertently exacerbating communication problems with linguistic minority patients.
Objective
To conduct a national environmental scan of US medical schools’ medical Spanish educational efforts, examine to what extent existing efforts meet basic standards, and identify next steps in improving the quality of medical Spanish education.
Design
Data were collected from March to November 2019 using an IRB-exempt online 6-item primary and 14-item secondary survey.
Participants
All deans of the Association of American Medical Colleges member US medical schools were invited to complete the primary survey. If a medical Spanish educator or leader was identified, that person was sent the secondary survey.
Main Measures
The presence of medical Spanish educational programs and, when present, whether the programs met four basic standards: formal curricular structure, faculty educator, learner assessment, and course credit.
Key Results
Seventy-nine percent of medical schools (125 out of 158) responded to either or both the primary and/or secondary surveys. Among participating schools, 78% (98/125) of medical schools offered medical Spanish programming; of those, 21% (21/98) met all basic standards. Likelihood of meeting all basic standards did not significantly differ by location, school size, or funding type. Fifty-four percent (53/98) report formal medical Spanish curricula, 69% (68/98) have faculty instructors, 57% (56/98) include post-course assessment, and 31% (30/98) provide course credit.
Conclusions
Recommended next steps for medical schools include formalizing medical Spanish courses as electives or required curricula; hiring and/or training faculty educators; incorporating learner assessment; and granting credit for student course completion. Future studies should evaluate implementation strategies to establish best practice recommendations beyond basic standards.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Effective patient-physician communication is one of the principal educational objectives of medical education, and medical history-taking alone has been shown to be sufficient to establish a diagnosis 75% of the time.1, 2 When designing educational content to teach clinical skills, it is essential to consider the communication needs, including language preferences, of the patient population.3 Accounting for the languages of United States (US) patients when designing curricula may improve language-concordant healthcare for the 25 million people with limited English proficiency (LEP), the majority of whom are Spanish speakers.4 Working with professional medical interpreters, while an essential strategy to address language discordance, is both underutilized5, 6 and inferior to competent language-concordant care.7 Moreover, the continued and likely underreported8 growth of the Spanish-speaking US population together with stagnant numbers of Hispanic/Latinx US physicians9 has resulted in a worsening Spanish-speaking physician deficit,10,11,12 prompting a national need to evaluate the scope and depth of medical Spanish education in US medical schools.
Medical Spanish courses focus on teaching “the use of Spanish in the practice of medicine for communication with patients”13 and have been proposed as an approach to meeting communication skills and cultural competency standards set by the Liaison Committee on Medical Education (LCME).14, 15 According to the most recent national survey, conducted between 2012 and 2014, a majority of US medical schools provide medical Spanish opportunities, but most do not evaluate learner skills.16 Program barriers identified included limited course length, heterogeneity of student language level, and insufficient faculty support.16
In response to the challenges identified to high-quality medical Spanish education, the guidelines first established by Reuland’s medical educator team in 200817 have been updated by language professor Hardin in 201318 and most recently in 2020 by a joint medical and language expert consensus.13 According to these sources, it is insufficient and unadvisable for institutions to encourage the isolated creation of medical Spanish educational interventions in response to student enthusiasm and demand19 without also providing resources for these courses to meet minimum basic standards. The basic standards include both administrative criteria (that courses be recognized in the school’s formal curriculum and that credit be granted to students) and pedagogical elements (instructor qualifications and learner assessment) that have been identified in prior literature3, 13, 14, 17, 18 as essential for effective and sustainable courses (Text Box 1).
Text Box 1. Basic standards for medical Spanish education in US medical schools
1. Formal curriculum Course includes a formal curricular structure either as an elective or required course in which learner competencies are specified and in which students can enroll (as opposed to an extracurricular club or an unsupervised student-run or online course).13, 17, 18 2. Faculty educator Course is taught by a faculty educator, defined as clinical faculty (including physician or non-physician clinician faculty) or language department faculty, rather than solely taught by students or bilingual community members without professional training as educators.13, 18 3. Post-course assessment Student performance and achievement of learner competencies are evaluated with a post-course assessment, allowing students to understand the strengths and limitations of their medical Spanish proficiency for safe patient care.3, 13, 17 4. Credit-granting Institution provides and documents educational credit for learners after satisfactory completion of the course.13, 14 |
Basic standards for medical education in a second language are necessary to ensure safe and responsible application of physician language skills with patients. Educational interventions that lack standards may inadvertently exacerbate communication problems with linguistic minorities.13 For example, lack of learner assessment may increase confidence and reduce interpreter use without sufficiently increasing skills—a concept known as false fluency.20,21,22,23 It has been further documented that medical students with some Spanish skills provide patient care in Spanish without confirmed language competence24 and teach medical Spanish out of perceived necessity without faculty or institutional support.16
The primary purpose of our study is to conduct an environmental scan of US medical schools’ medical Spanish educational efforts and examine to what extent existing programs meet basic standards. Secondly, we aim to analyze whether characteristics such as location, private or public funding, and size are associated with meeting or lacking basic standards to help inform future quality improvement initiatives at schools with similar characteristics. By evaluating the current landscape—including updated status and gaps—of medical Spanish efforts in US medical schools, we aim to identify the next steps necessary for schools to achieve basic standards for medical Spanish education.
METHODS
Design
We surveyed US medical schools to collect information about institutional practices and programming regarding medical Spanish education. To ensure a representative sampling of schools, we used the Association of American Medical Colleges’ (AAMC) list of 155 member medical schools as a sampling frame for the study.25 Three medical school campuses with independent curricula that are part of a multi-campus AAMC site were contacted individually, resulting in a total of 158 schools. We sent an initial email invitation to each recipient of the online primary and secondary surveys, and up to 3 reminder emails over 8 months to non-respondents. We collected data from March to November 2019. The institutional review board of the University of Illinois at Chicago determined that this study met exemption criteria on October 28, 2017 (Protocol # 2017-1157).
Participants
We identified email addresses of the curriculum and/or diversity and inclusion deans through publicly available medical school websites. The 6-item primary survey requested the contact information of a medical Spanish educator or leader (such as a course director, instructor, or faculty advisor), if applicable. If such a person was not identified either because the primary survey was not completed or because a medical Spanish educator was not known or reported by the primary survey respondent, we approached the school’s Latino Medical Student Association (LMSA) chapter representative via email to request the contact information for a medical Spanish educator or leader. Then, we sent a more detailed 14-item secondary survey to the identified educator or leader.
Main Measures
Presence of Medical Spanish Programs
Primary and secondary surveys asked about whether medical Spanish is currently offered at the institution, and if so, what types of courses were offered.
Basic Standards
The secondary survey also inquired about instructor qualifications, institutional credit provided for participating students, and assessment methodology used to evaluate learner skills. We developed the surveys (Supplementary Appendix 1) based on previously identified barriers to medical Spanish course implementation or sustenance16 and evidence-based guidelines summarized in Text Box 1.13, 17, 18
Analysis
We calculated descriptive statistics (cell percent and column percent) to examine overall trends in survey responses. We compared proportions using chi-squared tests. More specifically, we made comparisons between the following: (a) schools who reported formal medical Spanish curricula and those who reported only extracurricular activities, (b) schools who reported faculty instructors and those who had student-run courses, and (c) schools who reported providing course credit and those who did not. We used logistic regression models to examine the likelihood of programs offering assessments and providing individualized feedback to learners, as well as meeting basic standards (Text Box 1). We asked educators about providing feedback separately from whether they conducted assessments because some schools may not conduct a formal assessment yet may provide substantive learner feedback (e.g., based on course participation or informal observations), whereas others may conduct an assessment that does not include actionable feedback (beyond passing or not).
We examined school characteristics of location, size, and public or private funding as variables potentially associated with meeting basic standards. We analyzed location by AAMC region as well as by category of urban, suburban, or rural26 since the variable linguistic attributes of regional and local patient populations may influence schools’ curricular decisions regarding medical Spanish courses.3 We determined medical school funding source based on AAMC publicly available data,26 as well as school size (i.e., total matriculated students from 2019 to 2020).27 We conducted data compilation and analyses using Stata 16 (Stata Corp, College Station, TX).
RESULTS
Description of Survey Respondents
Seventy-nine percent of medical schools (125 out of 158) participated in the national survey; participation was defined as responding to either or both the primary and/or secondary surveys. Ninety-three percent (116/125) of responses represented schools who completed at least one of the surveys fully; 7% (9/125) were schools who provided partial responses (did not complete all survey questions). Participating and non-participating schools did not differ significantly by AAMC region, demonstrating geographic balance in responses across AAMC regions (Southern: 90%, Northeastern: 81%, Central: 78%, and Western: 70%) among participating schools (P = 0.183).
In the primary survey alone, 74% of medical schools (117/158) participated. Of 117 responses, 104 (89%) were full responses with answers recorded for all items. Of 158 schools, 111 (70%) identified a medical Spanish educator or leader and were sent the secondary survey; 103 of these 111 (93%) were identified through the primary survey, and 8 (7%) were identified through the LMSA chapter. Ninety-four percent of schools (104/111) who received a secondary survey participated, and 101 (97% of 104) were full responses. Of all 158 schools, 66% (104) participated in the secondary survey.
Across all primary survey respondents, 96% (112/117) agreed that medical Spanish education is wanted or needed at their institution. In addition, 84% (105/125) of all respondents and 91% (42/46) of schools who did not already have formal curricula agreed that a faculty development course to train faculty to teach medical Spanish would be desirable. Furthermore, 71% (74/104) of secondary survey respondents expressed interest in participating in a national task force of medical Spanish educators.
Curricular Structure
Among participating schools, 78% (98/125) reported some form of medical Spanish programming. Of that group, 54% (53/98) reported formal medical Spanish curricula (defined in Text Box 1). Extracurricular offerings included student-run programs (defined as student-led clubs or workshops, peer-taught courses, or self-study courses without faculty supervision) or online courses (commercial online programs for medical Spanish learning without faculty supervision). Fifty-nine percent of schools (58/98) reported having student-run programs, and 18% (18/98) reported sponsoring students to take online courses. Of note, some schools reported a combination of offerings. For example, 24% (24/98) had both student-run programs and formal curricula, 10% (10/98) had online and student-run options, and 8% (8/98) offered student-run, online, and formal curricular programs.
Some schools incorporated exposure to medical Spanish through clinical experiences, including clerkships and/or study abroad programs. For instance, 44% (43/98) reported offering local hospital or clinic clerkships with a high percentage Spanish-speaking population. Of 43 schools reporting clinical clerkships for students to practice Spanish in direct patient care, only one required that students first complete medical Spanish training. Additionally, 40% (17/43) of schools that offered local clerkships reported not having the option of a formal medical Spanish course. Seventy-two percent of schools (71/98) reported Spanish study abroad opportunities, although the majority (68%, 43/71) reported having no associated medical Spanish didactics.
Faculty and Course Credit
Sixty-nine percent of schools (68/98) reported having faculty medical Spanish educators. Most reported faculty educators who were clinical faculty (79%, 54/68), most of whom were physicians (78%, 42/54). Nearly half (49%, 32/68) reported language department faculty educators. Some schools (18%, 12/68) reported multiple instructors, including both clinical and language faculty, for different medical Spanish offerings. Other non-faculty instructors included students or bilingual community members without professional training as educators (e.g., translators, interpreters, and a librarian). A minority (31%, 30/98) of schools reported granting student course credit.
Post-Course Assessments
Overall, 57% of respondents (56/98) reported learner post-course assessments. Schools with formal curricula had significantly greater use of post-course assessments (80% versus 20%, P < 0.001) and individualized performance feedback for learners (78% versus 22%, P < 0.001). Assessment types varied, including standardized patient (SP) encounters (29%, 28/98), the telephone-based Clinician Cultural and Linguistic Assessment (CCLA)28 (27%, 26/98), written examinations (27%, 26/98), oral faculty-administered examinations (25%, 25/98), or faculty-observed patient interviews (13%, 13/98). Some schools used mixed assessment methodology combining two or more methods. Schools with faculty instructors had significantly greater use of assessments (87% versus 46%, P < 0.001) and individualized feedback (87% versus 46%, P < 0.001). In addition, credit-granting courses had significantly greater use of assessments (44% versus 12%, P = 0.001) and feedback (52% versus 2%, P < 0.001).
A multivariate analysis controlling for these factors indicated that schools with formal curricula (Odds Ratio [OR] = 9.56, P < 0.001) and faculty instructors (OR = 3.48, P = 0.045) had significantly greater odds of conducting post-course assessments; similarly, schools with formal curricula (OR = 4.67, P = 0.011), faculty instructor (OR = 4.07, P = 0.044), and credit hours (OR = 25.28, P = 0.003) had significantly greater odds of providing feedback. Peer-taught courses did not have a significant impact on the likelihood of conducting assessments or providing feedback.
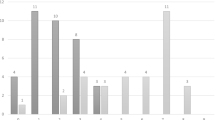
Effect of School Characteristics
Table 1 shows the regional distribution of current US medical Spanish educational offerings by key program features. Western schools were significantly more likely to provide credit for medical Spanish courses, and Northeast schools reported a significantly greater number of Spanish-speaking country study abroad experiences without formal didactics. Other program features did not significantly vary by region. Across all regions, one-third or fewer schools per region met all four basic standards. When analyzed by other school characteristics, school funding type (public or private) and location type (urban, suburban, or rural) had no significant effect on program features or likelihood of meeting all basic standards. Schools of bigger size were more likely to report abroad clerkships with Spanish didactic component (P = 0.030), but school size had no other effects of significance on medical Spanish programming.
DISCUSSION
Our national survey participants were deans and medical Spanish educators with geographically balanced data representation from 87% of AAMC-member US medical schools. Our findings confirm that a vast majority of medical schools (78% of participating schools) offer some form of Spanish programming. This represents a significant increase in the number of medical schools offering medical Spanish during the past 5 years, compared to 66% as identified by a 2012-2014 national survey16 (12% increase, P = 0.017).
Importantly, compared to prior efforts to describe medical Spanish educational programs, our survey further examines what is meant by schools reporting Spanish programming. While 78% of respondent schools reported teaching medical Spanish, less than a quarter (21%) of those schools that offered medical Spanish met all four basic standards. More schools offered medical Spanish in the form of extracurricular activities such as student-run clubs, workshops, or interest groups (59%) or as clinical experiences locally or abroad (71%), rather than as formal curricula (54%). In most cases, clinical experiences with Spanish-speaking patients were not paired with formal Spanish communication skills education or assessment, potentially posing concerns regarding miscommunication. While practice through student clubs and clinical exposures is valuable for learning, these opportunities should be paired with formal education under faculty supervision that allows students to gain and verify specific communication competencies prior to patient care.13, 15
Our survey shows that medical students continue to demonstrate positive leadership in medical Spanish education, as evidenced by the 59% of schools that report student-run efforts. Medical students’ commendable leadership in this arena should be supported, guided, and assessed using evidence-based curricula (such as courses that have published successful outcomes15, 29,30,31,32) and applying competency criteria13 by trained professionals. The survey results found that courses in which faculty teach or direct medical Spanish courses are significantly more likely to meet basic standards related to assessment. Informal medical Spanish initiatives, such as extracurricular offerings or clinical experiences, are significantly more likely to forgo learner assessment altogether compared to formal curricula, raising concerns related to insufficient training and false fluency.5, 20
Furthermore, our results demonstrate that medical Spanish courses that received institutional support by formalizing curricula and granting course credit were more likely to conduct student skills assessment. However, the majority of courses (69%, 68/98) were not acknowledged institutionally as credit-granting, even when taught by faculty with formal curricula, making it difficult for faculty to justify spending the amount of effort required to develop and teach a high-quality course. Furthermore, students may be unable or unwilling to dedicate time to non-credit-granting medical Spanish opportunities, even if high in quality, due to competing demands of coursework that provides grades, credit, or examination components.
The study is limited by possible respondent bias. As a voluntary survey, it is possible that participating schools felt particularly strongly about the topic surveyed. Future study is needed to evaluate not only whether schools’ medical Spanish efforts meet minimum basic standards but also to establish best practice recommendations for ideal implementation of each standard. For example, even among schools with formal courses, the curricular structure may vary (e.g., short intensive courses that require full-time student effort for several weeks vs. longitudinal courses spanning a year or more). Types of learning activities and topics covered may also vary and merit additional evaluation. Secondly, faculty qualifications could be further studied including the effectiveness of language compared to medical faculty, single or multiple educators, and faculty development programs. Third, institutional support strategies at existing programs that meet basic standards should be analyzed to identify replicable models for faculty recruitment and retention, credit designation for students, and timing of courses within the larger institutional communication skills curricula.
Finally, the basic standard of assessment represents a critical component to ensure that learners are accurately aware of their language skills and limitations prior to patient care. Currently, medical Spanish assessment varies widely both in type of evaluation conducted and in the amount of feedback provided to learners. Prior literature on clinical communication skills evaluation supports the use of performance-based examinations, such as SP encounters, to assess learner communication skills,33, 34 but further study is needed to evaluate specifically the effectiveness of different types of medical Spanish assessment, their relationship to learner competencies or clinical performance, and accessible methods of implementation in US medical schools. Inclusion of individualized feedback (e.g., specific strengths and limitations) in assessment results may be considered as part of best practice recommendations for meeting the medical Spanish assessment basic standard. Future studies should investigate the effectiveness and practical implications (e.g., cost and effort) of conducting a single post-course assessment versus multiple assessments during the educational intervention as well as acceptable passing standards that signify readiness for patient care in Spanish without an interpreter.
Despite increasing national efforts in offering medical Spanish education to medical students, few existing courses meet basic standards. The recommended next steps for medical schools to enhance high-quality medical Spanish education include formalizing medical Spanish courses into the medical school elective or required curricula; hiring and/or training clinical and/or language faculty educators; incorporating learner assessment; and granting course credit. These strategies are expected to positively impact the quality of LCME-required medical communication skills training in languages besides English and can be adapted to future programs for other languages and health professions. Enhancing the structure and consistency of US medical schools’ existing medical Spanish efforts through curricular integration, faculty development, learner assessment, and course credit designation will in turn support the sustainable development of a competent language-concordant physician workforce.
Data Availability
Medical school funding source and location type were obtained from publicly available data from the Association of American Medical Colleges (AAMC), Medical School Admission Requirements, accessible at https://apps.aamc.org/msar-ui/#/landing. The total number of matriculated students from 2019 to 2020 was obtained from publicly available reports from the AAMC, accessible at https://www.aamc.org/data-reports/students-residents/interactive-data/2019-facts-enrollment-graduates-and-md-phd-data.
References
Peterson MC, Holbrook JH, Von Hales D, Smith NL, Staker LV. Contributions of the history, physical examination, and laboratory investigation in making medical diagnoses. West J Med. 1992\; 156(2):163-5.
Lown B. The lost art of healing: practicing compassion in medicine. New York Ballantine Books:1999.
Ortega P, Pérez N, Robles B, Turmelle Y, Acosta D. Teaching Medical Spanish to Improve Population Health: Evidence for Incorporating Language Education and Assessment in U.S. Medical Schools. Health Equity. 2019;3(1):557–566. doi:https://doi.org/10.1089/heq.2019.0028
Zong J, Batalova J. The limited English proficient population in the United States. Migration Policy Institute; 2015
Diamond, L.C., Schenker, Y., Curry, L., Bradley, E.H., Fernandez, A. Getting By: Under-Use of Interpreters by Resident Physicians. J Gen Intern Med, 2009; 24(2): 256-262.
Showstack R. Patients don’t have language barriers; the healthcare system does. Emergency Medicine Journal. 2019;36:580-581.
Diamond L, Izquierdo K, Canfield D, Matsoukas K, Gany F. A Systematic Review of the Impact of Patient-Physician Non-English Language Concordance on Quality of Care and Outcomes. J Gen Intern Med. 2019;34(8):1591–1606. doi:https://doi.org/10.1007/s11606-019-04847-5
Azar KM, Moreno MR, Wong EC, Shin JJ, Soto C, Palaniappan LP. Accuracy of data entry of patient race/ethnicity/ancestry and preferred spoken language in an ambulatory care setting. Health Serv Res. 2012;47(1 Pt 1):228–240.
Association of American Medical Colleges. Table B-4: Total U.S. Medical School Graduates by Race/Ethnicity and Sex, 2014-2015 through 2018-2019. https://www.aamc.org/download/321536/data/factstableb4.pdf. Accessed 3 Sept 2020.
García ME, Bindman AB, Coffman J. Language-Concordant Primary Care Physicians for a Diverse Population: The View from California. Health Equity. 2019;3(1):343–349. doi:https://doi.org/10.1089/heq.2019.0035
Fernández A, Pérez-Stable EJ. ¿Doctor, habla español? Increasing the Supply and Quality of Language-Concordant Physicians for Spanish-Speaking Patients. J Gen Intern Med. 2015;30(10):1394–1396. doi:https://doi.org/10.1007/s11606-015-3436-x
Ortega P. Spanish Language Concordance in Medical Care: A Multifaceted Challenge and Call to Action. Academic Medicine 2018;93(9):1276-1289.
Ortega P, Diamond L, Alemán MA, Fatás-Cabeza J, Magaña D, Pazo V, Pérez N, Girotti JA, Ríos E. Medical Spanish Standardization in U.S. Medical Schools: Consensus Statement from a Multidisciplinary Expert Panel. Acad Med. 2020;95(1):22-31.
Liaison Committee on Medical Education. Functions and structure of a medical school: Standards for accreditation of medical education programs leading to the MD degree. Effective academic year: 2021–22. http://lcme.org/publications. Published March 2020. Accessed 17 April 2020.
Ortega P, Pérez N, Robles B, Turmelle Y, Acosta D. Strategies for Teaching Linguistic Preparedness for Physicians: Medical Spanish and Global Linguistic Competence in Undergraduate Medical Education. Health Equity. 2019;3(1):557-566. https://doi.org/10.1089/heq.2019.0029
Morales R, Rodríguez L, Singh A, Stratta E, Mendoza L, Valerio MA, & Vela M. National Survey of Medical Spanish Curriculum in U.S. Medical Schools. J Gen Intern Med. 2015;30(10):1434-1439.
Reuland DS, Frasier PY, Slatt LM, Alemán MA. A longitudinal medical Spanish program at one U.S. medical school. J Gen Intern Med. 2008 Jul;23(7):1033-7.
Hardin KJ, Hardin DM. Medical Spanish programs in the United States: a critical review of published studies and a proposal of best practices. Teach Learn Med. 2013;25(4):306-11.
Ortega P. In Reply to Schmuter. Acad Med. 2020;95(2):172. doi:https://doi.org/10.1097/ACM.0000000000003082
Flores G, Mendoza FS. ¿Dolor aquí? ¿Fiebre?: A little knowledge requires caution. Arch Ped Adolesc Med 2002;156(7):638-40.
Mazor S, Hampers L, Chande V, Krug S. Teaching Spanish to pediatric emergency physicians: effects on patient satisfaction. Arch Pediatr Adolesc Med. 2002;156(7):693–695.
Prince D, Nelson M. Teaching Spanish to emergency medicine residents. Acad Emerg Med. 1995;2(1):32–36. doi: https://doi.org/10.1111/j.1553-2712.1995.tb03076.x.
Diamond LC, Jacobs EA. Let’s not contribute to disparities: the best methods for teaching clinicians how to overcome language barriers to healthcare. J Gen Intern Med. 2010;25 Suppl 2: S189-S193.
Vela B., Fritz G., Girotti, J. Medical Students’ Experiences on Interpreting for LEP Patients at Two US Medical Schools. J Racial Ethn Health Disparities. 2015;3(2):245-249.
Association of American Medical Colleges. AAMC Medical School Members. https://members.aamc.org/eweb/DynamicPage.aspx?site=AAMC&webcode=AAMCOrgSearchResult&orgtype=Medical%20School. Updated 2020. Accessed April 17, 2020.
Association of American Medical Colleges, Medical School Admission Requirements https://apps.aamc.org/msar-ui/#/landing. Accessed September 3, 2020.
Association of American Medical Colleges. Table B-5.2 Total Enrollment by U.S. Medical School and Race/Ethnicity (Alone or In Combination), 2019-2020. https://www.aamc.org/data-reports/students-residents/interactive-data/2019-facts-enrollment-graduates-and-md-phd-data. Accessed 3 Sept 2020.
Tang, G., Lanza, O., Rodríguez, F. M., & Chang, A. The Kaiser Permanente Clinician Cultural and Linguistic Assessment Initiative: research and development in patient-provider language concordance. Am J Public Health. 2011;101(2):205-8.
Ortega P, Park YS, Girotti JA. Evaluation of a Medical Spanish Elective for Senior Medical Students: Improving Outcomes through OSCE Assessments. Med Sci Educ. 2017;27(2):329-337. doi:https://doi.org/10.1007/s40670-017-0405-5
O’Rourke K, Gruener G, Quinones D, Stratta E, Howell J. Spanish Bilingual Medical Student Certification. MedEdPORTAL. 2013;(9). doi:https://doi.org/10.15766/mep_2374-8265.9400
Pereira JA, Hannibal K, Stecker J, Kasper J, Katz JN, Molina RL. Professional language use by alumni of the Harvard Medical School Medical Language Program. BMC Med Educ. 2020;20(1):4. Published 2020 Nov 6. doi:https://doi.org/10.1186/s12909-020-02323-x
Ortega P, López-Hinojosa I, Park YS, Girotti JA. Medical Spanish Musculoskeletal and Dermatologic Educational Module. MedEdPORTAL. 2021;17:11071. Published 2021 Jan 12. doi:https://doi.org/10.15766/mep_2374-8265.11071
Chalabian J, Dunnington G. Q4patients: a new method to assess the clinical skills of physicians. Best Pract Benchmarking Healthc. 1997;2(4):174-7.
Federation of State Medical Boards, National Board of Medical Examiners. Content description and general information: Step 2 Clinical Skills (CS). https://www.usmle.org/pdfs/step-2-cs/cs-info-manual.pdf. Updated 2019. Accessed 17 April 2020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
P. Ortega receives author royalties from Saunders, Elsevier. The authors declare that they have no other conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior presentations
Part of the data reported in this manuscript was presented by N. Francone and M.P. Santos at the Second Medical Spanish Summit virtual conference on October 10, 2020.
Supplementary Information
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Ortega, P., Francone, N.O., Santos, M.P. et al. Medical Spanish in US Medical Schools: a National Survey to Examine Existing Programs. J GEN INTERN MED 36, 2724–2730 (2021). https://doi.org/10.1007/s11606-021-06735-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-06735-3