Abstract
Background
Smoking starts in early adulthood and persists throughout the life course, but the association between these trajectories and midlife cognition remains unclear.
Objective
Determine the association between early to midlife smoking trajectories and midlife cognition.
Design
Prospective cohort study.
Participants
Participants were 3364 adults (mean age = 50.1 ± 3.6, 56% female, 46% Black) from the Coronary Artery Risk Development in Young Adults (CARDIA) study: 1638 ever smokers and 1726 never smokers.
Main Measures
Smoking trajectories were identified in latent class analysis among 1638 ever smokers using smoking measures every 2–5 years from baseline (age 18–30 in 1985–1986) through year 25 (2010–2011). Poor cognition was based on cognitive domain scores ≥ 1 SD below the mean on tests of processing speed (Digit Symbol Substitution Test), executive function (Stroop), and memory (Rey Auditory Verbal Learning Test) at year 25.
Results
Five smoking trajectories emerged over 25 years: quitters (19%), and minimal stable (40%), moderate stable (20%), heavy stable (15%), and heavy declining smokers (5%). Heavy stable smokers showed poor cognition on all 3 domains compared to never smoking (processing speed AOR = 2.22 95% CI 1.53–3.22; executive function AOR = 1.58 95% CI 1.05–2.36; memory AOR = 1.48 95% CI 1.05–2.10). Compared to never smoking, both heavy declining (AOR = 1.95 95% CI 1.06–3.68) and moderate stable smokers (AOR = 1.56 95% CI 1.11–2.19) exhibited slower processing speed, and heavy declining smokers additionally had poor executive function. For minimal stable smokers (processing speed AOR = 1.12 95% CI 0.85–1.51; executive function AOR = 0.97 95% CI 0.71–1.31; memory AOR = 1.21 95% CI 0.94–1.55) and quitters (processing speed AOR = 0.96 95% CI 0.63–1.48; executive function AOR = 0.98 95% CI 0.63–1.52; memory AOR = 0.97 95% CI 0.67–1.39), no association was observed.
Conclusions
The association between early to midlife smoking trajectories and midlife cognition was dose-dependent. Results underscore the cognitive health risk of moderate and heavy smoking and the potential benefits of quitting on cognition, even in midlife.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
About 48 million individuals worldwide have dementia,1 a condition characterized by the loss of cognitive and day-to-day functioning. Smoking in midlife (age 45–64 years) and late-life (age ≥ 65 years) periods may be a risk factor for cognitive decline and dementia,2 but studies are controversial. Smoking habits often begin in adolescence (age 10–17 years) and early adulthood (age 18–40 years) and persist for decades, with variable frequency and duration of exposure.3,4 Of adult smokers, about 90% start smoking in adolescence,5 and transition from experimentation to established smoking habits by the mid-to-late twenties.6 Over the life course, smoking tends to peak in early adulthood4,7,8 combined with significant life changes, such as going to college and entering the workforce,9 with declines taking place in midlife.3 Although the period from early to midlife (age 18–64 years) is often critical for establishing life-long smoking patterns,3,4 data are limited regarding associations of smoking during these earlier life stages with cognitive function.
Accumulating evidence from observational studies suggest that brain changes leading to dementia including vascular changes probably take decades to accumulate and may be detected as early as midlife,10,11 but the contribution of these earlier changes to cognitive aging is unclear. Most investigations of smoking and cognition have focused on risk relationships in midlife and late-life,12,13,14,15 and this association in earlier life periods is not well defined. Furthermore, although smoking exposure is traditionally indexed by pack-years (years smoked multiplied by cigarettes smoked per day),16 adults in early to midlife periods often develop different patterns of smoking over these earlier life stages, 3 which cannot be adequately captured by more traditional methods to assess smoking exposure. Understanding how these effects of early to midlife smoking may influence midlife cognition could inform a key time point for behavioral change.
As part of the ongoing Coronary Artery Risk Development in Young Adults (CARDIA) study, we determined the association between early to midlife smoking trajectories and midlife cognition. We also investigated the association between lifetime smoking exposure in pack-years and midlife cognition. We hypothesized that individuals with heavy smoking exposure over these earlier life periods would be at greater risk of poor midlife cognition.
METHODS
Study Design and Sample
CARDIA is a prospective cohort study of 5115 Black and White women and men, initially age 18 to 30 years, recruited at four US cities (Birmingham, AL; Minneapolis, MN; Chicago, IL; and Oakland, CA) in 1985–1986. Participants have completed an initial examination (year 0) and repeated follow-up visits at years 2, 5, 7, 10, 15, 20, and 25. Participants provided written informed consent at each visit and study protocols were reviewed by institutional review boards from each study site. Further details regarding the design of CARDIA have been previously reported.17,18
Among the 5115 participants, 5078 (99.2%) completed ≥ 3 smoking assessments over 25 years, and 2621 reported lifetime smoking (included in analysis to identify smoking trajectory groups) and 2457 participants reported never smoking. There were 3499 participants reassessed at year 25, the time of cognitive testing. To examine the association between early to midlife (age range over 25 years of follow-up = 18 to 59) smoking trajectories and midlife cognition at year 25 (mean age, cognitive testing = 50.1 ± 3.6 years, range = 42 to 59), we included those with ≥ 3 smoking assessments over 25 years, and > 1 cognitive test at year 25. The final analytic cohort included 3364 participants (Appendix Fig. 1): 1638 were lifetime/ever smokers and 1726 were never smokers. Participants missing cognitive data were more likely to be male, Black, start smoking at younger ages, and had higher cholesterol.
Measures
Cigarette smoking was assessed at each CARDIA visit. Participants were asked about the number of years they smoked, the age they started smoking, number of cigarettes smoked per day, and, as applicable, years since smoking cessation. These data were used to determine their smoking status over 25 years. We defined ever smokers (lifetime smoking) as those reporting > 1 cigarette smoked per day for > 1 visit. Participants who never smoked were characterized as those reporting 0 cigarettes smoked per day for all visits. Among ever smokers, we estimated mean number of cigarettes smoked per day for all visits. Lifetime smoking exposure among ever smokers was calculated in pack-years (1 pack-year = smoking 1 pack per day for 1 year of smoking 7300 cigarettes or 1 year × 365 days per year × 1 pack per day × 20 cigarettes per pack),19 categorized as 0, 1 day to < 10 pack-years, and ≥ 10.3,20 Lifetime smoking trajectories were based on the number of cigarettes smoked per day among ever smokers, as described in the “Analyses” section.
Three cognitive tests were administered by interviewers at year 25. The Rey Auditory Verbal Learning Test (RAVLT) is a test of verbal memory with higher scores indicating better function;21 we reference this domain as verbal memory. The Digit Symbol Substitution Test (DSST) is a test of processing speed, executive function, and working memory with higher score suggesting better function;22 we refer to this domain as processing speed. The Stroop Test assesses executive function; lower interference scores represent better function;23,24 we refer to this domain as executive function. The inverse of the Stroop interference score was used to allow interpretation of better function with higher scores on all cognitive tests.19 We derived cognitive z-scores from each domain at year 25, and we defined poor cognitive function using a cutoff ≥ 1 SD below the CARDIA cohort mean for each test, as previously used in CARDIA25 and other population-based studies.26
We considered critical risk factors for cognitive aging outcomes at year 25, unless otherwise noted. We assessed demographic characteristics using self-reports and defined income based on one of nine pre-tax family income ranges, accounting for household size by adjusting for the number of people living in the home.27 Physical activity was measured with the CARDIA Physical Activity questionnaire.28 Depression was assessed using the Center for Epidemiologic Studies Depression (CESD) scale; scores ≥ 16 suggest clinical depression.29 We defined cardiovascular risk factors including obesity (body mass index ≥ 30 kg\m2), hypertension, diabetes, and high cholesterol, using a combination of self-report, clinic assessments, and medication use. We estimated lifetime alcohol use in drink-years over 25 years; 1 drink-year = the amount of alcohol used in 1 year by a person consuming 1 drink per day.30 Lifetime marijuana use was estimated in joint-years over 25 years; 1 joint-year = 365 days of marijuana use.31 Apolipoprotein ε4 (APOE ε4 presence or not), the high risk variant of APOE gene—the gene most commonly associated with increased risk for late-onset Alzheimer’s disease—was derived from year 7 blood samples.32,33
Analyses
Smoking trajectories were generated based on smoking assessments every 2–5 years from baseline (year 0) through year 25 (average cigarettes smoked per day at years 0, 2, 5, 7, 10, 15, 20, and 25) using latent class growth analysis, a person-centered approach to modeling that can be used to identify different groups of individuals with similar behavioral patterns over the life course.34,35 Participants who never smoked (48.3% [n = 2457] of sample), those reporting 0 cigarettes smoked per day for all visits, were specified as an a priori class and were excluded from the latent class growth trajectory analysis.36 Repeated smoking data was modeled as zero-inflated Poisson (ZIP), to account for extra zeros.35 We fit 3-, 4-, 5-, and 6-class models; each model for which a given number of trajectories were selected, cubic, quadradic, and linear terms were evaluated to identify the trajectory shapes that best fit the data.37 We determined the number of trajectories to retain by computing the Log Bayes factor, which compares Bayesian Information criterion (BIC) values between models, and indicates the more complex model with lower BIC values provides the best model fit. While a 6-trajectory model was associated with further improvement in model fit, one trajectory included < 5% of participants; therefore, a 5-trajectory model was retained for analyses.
At year 25, we used descriptive statistics to compare participants with different smoking trajectories and never smokers. We used unadjusted and adjusted logistic regression to examine associations between early to midlife smoking trajectories (compared to never smokers) and poor midlife cognition. We also investigated the odds associated with poor midlife cognition in ever smokers with 1 day to < 10 and 10 or more pack-years of exposure (compared to never smokers) using unadjusted and adjusted logistic regression. Pack-year categorizations were based on previous work in CARDIA that used 10 as cutoff to distinguish light vs. chronic smoking.3,20 Adjusted logistic regression models controlled for age, sex, race, education, hypertension, diabetes, physical activity, alcohol and marijuana use, depression, and age started smoking. Analyses were conducted in SAS version 9.4 and R version 3.4.3.
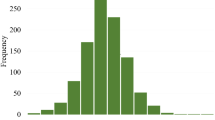
RESULTS
The 5 identified smoking trajectories reflected overall patterns of minimal, moderate, and heavy exposure, which were relatively stable or declined from early adulthood to midlife over 25 years. We labeled the trajectories as heavy declining, heavy stable, moderate stable, and minimal stable smokers and quitters (Fig. 1). Among 1638 (48.6%) ever smokers, there were 5.2% (n = 86) heavy declining, 15.1% (n = 248) heavy stable, 20.0% (n = 334) moderate stable, and 40.0% (n = 646) minimal stable smokers, and 19.7% (n = 324) quitters. Trajectory groups differed by age, race, sex, education, age participants started smoking, income, hypertension, diabetes, physical activity, depression, and marijuana and alcohol use. The trajectories did not differ in high cholesterol, obesity, or APOE ε4 status (Table 1).
Smoking trajectories of ever smokers. *The 5 trajectories of 1638 ever smokers in the Coronary Artery Risk Development in Young Adults study were characterized as follows: heavy declining (n = 86 [5.2%]), heavy stable (n = 248 [15.1%]), moderate stable (n = 646 [39.4%]), and minimal stable smokers (n = 324 [9.7%]) and quitters (n = 324 [9.7%]).
Compared to never smoking, the odds of poor cognitive performance at midlife were associated with minimal stable, moderate stable, and heavy stable trajectories on all tests (Fig. 2).
Association between early to midlife smoking trajectories and cognitive function in midlife among the 3364 CARDIA participants. *The adjusted logistic regression models controlled for age, race, sex, education, income, hypertension, diabetes, physical activity, depression, age started smoking, and alcohol and marijuana use. CARDIA indicates the Coronary Artery Risk Development in Young Adults study; circles, odds ratios; and error bars, 95% CI.
Heavy declining smoking was associated with poor performance on the DSST (OR = 2.70 95% CI 1.62–4.48) and Stroop test (OR = 1.80 95% CI 1.01–3.21), but not the RAVLT (OR = 1.17 95% CI 0.68–2.03). For quitters, no significant effect (RAVLT OR = 0.87 95% CI 0.63–1.21; DSST OR = 0.97 95% CI 0.66–1.41; Stroop OR = 0.89 95% CI 0.60–1.34) was observed. After multivariable adjustment for demographics, age started smoking, income, hypertension, diabetes, depression, physical activity, and alcohol and marijuana use, the effect observed for heavy declining (adjusted OR, AOR for DSST = 1.95 95% CI 1.06–3.68; Stroop AOR = 2.34 95% CI 1.21–4.51) and heavy stable smoking (DSST AOR = 2.22 95% CI 1.53–3.22; RAVLT AOR = 1.48 95% CI 1.05–2.10; Stroop AOR = 1.58 95% CI 1.05–2.35) remained significant, and for moderate stable smoking on the DSST (AOR = 1.56 95% CI 1.11–2.19). There was no longer an association for minimal stable smokers after adjustment.
Of 1638 ever smokers, 957 (58.4%) had < 10 pack-years of smoking exposure and 681 (41.5%) had 10 or more. Compared to never smoking, the odds of poor cognitive performance were associated with ≥ 10 pack-years of exposure on all tests (RAVLT OR = 1.73 95% CI 1.40–2.14; DSST OR = 3.09 95% CI 2.47–3.86; Stroop OR = 2.03 95% CI 1.59–2.59), and the odds ratio was greater having < 10 pack-years of exposure for the RAVLT and DSST (RAVLT OR = 1.26 95% CI 1.03–1.54; DSST OR = 1.36 95% CI 2.47–3.86), but not the Stroop test (OR = 1.16 95% CI 0.91–1.49). After adjustment, associations remained significant in those with ≥ 10 pack-years of exposure, but not < 10 pack-years of exposure (Fig. 3).
The association between lifetime smoking exposure in pack-years from early adulthood to midlife and poor cognitive function in midlife among the 3364 CARDIA participants. *The adjusted logistic regression models controlled for age, race, sex, education, income, hypertension, diabetes, physical activity, depression, age started smoking, and alcohol and marijuana use. CARDIA indicates the Coronary Artery Risk Development in Young Adults study; circles, odds ratios; and error bars, 95% CI.
DISCUSSION
In this cohort, we found that early to midlife smoking trajectories were differentially associated with cognition at midlife. In particular, heavy stable smokers were the most likely to have poor cognition relative to never smokers. Heavy declining and moderate stable smokers both were more likely to exhibit slower processing speed, while heavy declining smokers were additionally more likely to demonstrate worse executive function, but no effects were observed for minimal stable smokers or quitters.
Our results are supported by previous longitudinal studies of smoking in midlife and late-life. These investigations have found that smoking, especially heavy exposure, is associated with cognitive decline and risk of dementia in older adults. In the slightly older 1946 British National Birth Cohort,14 heavy smoking for adults in their mid-thirties was associated with decline in memory but not visual search at midlife. A large multi-ethnic cohort of healthcare members focused on an even later window of smoking exposure,15 midlife to late-life, and found that heavy smoking in midlife and late-life more than doubled the risk of late-life dementia. Findings were similar in a prospective study of community-dwellers,38 in whom sustained smoking throughout late-middle age was linked to risk of late-life dementia. We focused on an earlier period, early adulthood to midlife, and found that smoking exposure in these earlier life stages may be harmful to cognition as early as midlife. In particular, our results suggest that a trajectory of heavy smoking, starting in early adulthood (18 to 30 years), may contribute quite considerably to poor cognitive function by midlife (42 to 59 years), and also indicate that a trajectory of moderate smoking could lead to poor cognition by midlife. These findings suggest earlier life periods may be critical to promote behavior change interventions coupled with medication strategies that are focused on quitting to delay the process of cognitive aging.
Other investigations in more homogeneous, slightly older cohorts, such as the Whitehall II Cohort Study,39 Honolulu-Asia Aging Study,40 and the Doetinchem Cohort Study,41 have also indicated that midlife and late-life smoking may contribute to poor late-life cognition, but these studies have focused on evaluating current exposure. These findings are likewise consistent with prospective cohort studies of smoking and cognitive decline,2 as assessed with clinical measures of global cognitive function such as the Mini-Mental State Examination, but findings are mixed regarding other domains. Studies also have investigated the contribution of lifetime smoking to poor cognition 15,42,43 but have focused on older cohorts. In this study, the odds of poor midlife cognition were linked with ≥ 10 pack-years of smoking exposure, but not < 10 pack-years. These results align with studies indicating greater smoking exposure in midlife and late-life may raise the risk of cognitive aging later in life,15,42,43,44 but some studies found no association.45,46
Our results also add to the literature on the benefits of smoking cessation by indicating that quitting in earlier life periods may be a particularly effective strategy to reduce the risk of poor midlife cognition. This observation aligns with results from slightly older cohort studies, 39,47,48,49 which have reported quitting in midlife and late-life periods has no effect on cognition compared to never smoking. Previous clinical trials50 of smoking status on cognition among elderly adults (68 to 88 years) also highlight the benefits of smoking cessation, and suggest that quitting later in the life course attenuates the effect of smoking on cognitive aging. Our results support these findings and reinforce the importance of tobacco control and public health efforts that target smokers of all ages to increase the effectiveness of prevention and cessation.4 While these efforts often emphasize benefits of quitting for cancer, cardiovascular, and mortality risk, the benefits for brain health are often overlooked. Our results highlight the potential benefits of quitting on cognition even in midlife and provide support for cessation and prevention efforts to incorporate messaging on the cognitive benefits of quitting as early as midlife.
The effects of smoking over the life course on specific cognitive domains are unclear but may involve several pathways. Physiologic studies51 suggest that smoking augments oxidative stress and inflammation, which could be important pathophysiologic mechanisms by increasing levels of amyloid and tau in developing dementia. Pathways of oxidative stress and inflammation may also directly increase neurodegenerative pathology.51 Smoking may increase dementia risk by other risk factors, such as poor diet,52,53 impaired pulmonary function,54 and depression.55 Imaging studies suggest smoking exposure could influence cognition and dementia risk through APOE ε4 pathways.56 Smoking also is a risk factor for cerebrovascular diseases,57,58,59including stroke, hypertension, and diabetes, suggesting smoking may affect cognition through vascular pathways. Our results observed with processing speed and executive function for moderate stable and heavy declining smokers may reflect associations with vascular mechanisms, while heavy stable smokers may have more extensive damage. These pathways, and the mechanisms by which early to midlife smoking may increase risk of poor cognition and subsequent dementia, need clarified in future studies.
CARDIA is a large, diverse, well-characterized longitudinal cohort in which we were able to identify early to midlife smoking trajectories and link these trajectories to cognition at midlife. We also used a population-based sampling method and accounted for several potential confounders. However, there are limitations to consider. Smoking patterns may change over time, but the trajectory analysis did not accommodate this.4 We were unable to assess every cognitive domain and there may be selection bias due to differential loss to follow-up. Since cognitive assessments were only available at year 25, we cannot determine when a change in cognition might have occurred and associate it with a change in smoking exposure. Participants with missing cognitive data were more likely to be smokers, but we expect this would contribute to a bias toward the null. Studies of older adults have reported on features that may be identified based on cognitive testing to estimate progression to dementia, but contribution of such cognitive features to dementia in midlife is unclear.10 Poor cognition in early- to middle-aged adults, such as those in CARDIA, may signal mild but mostly static change in cognition by midlife or may start to define a population at higher risk of later cognitive impairment.10 Finally, while our measure of poor cognition (≥ 1 SD below the mean) is standard in population-based studies of older adults, the clinical significance of poor cognitive function is not well-defined in the midlife period and the relevance this early in the life course is not yet clear.60
We identified a dose-response relationship between early to midlife smoking trajectories and cognitive health risk at midlife. While current public health and prevention efforts highlight tobacco-related harms for cancer, cardiovascular, and mortality risk, our study provides evidence for the need to also target cognitive function as early as midlife. Young and middle-aged adults, especially those who develop a trajectory of moderate or heavy smoking, may represent critical subgroups for early monitoring and education. Additional research is needed to improve early detection of those at highest risk of poor cognitive function and to determine effective cessation efforts to delay the process of cognitive aging even earlier in the life course.
References
Prince MJ, Wu F, Guo Y, et al. The burden of disease in older people and implications for health policy and practice. The Lancet. 2015;385(9967):549-562.
Anstey KJ, von Sanden C, Salim A, O’Kearney R. Smoking as a risk factor for dementia and cognitive decline: a meta-analysis of prospective studies. American journal of epidemiology. 2007;166(4):367-378.
Mathew A, Colangelo L, Allen N, et al. Life Course Cigarette Smoking and Lung Health from Young Adulthood to Middle Age: Findings from the CARDIA Lung Study. In: C16. CIGARETTE, E-CIGARETTE, AND MARIJUANA SMOKING: HUMAN AND MOUSE STUDIES. American Thoracic Society; 2018:A4449-A4449.
Dutra LM, Glantz SA, Lisha NE, Song AV. Beyond experimentation: Five trajectories of cigarette smoking in a longitudinal sample of youth. PloS one. 2017;12(2):e0171808.
Academies IoMotN. Public Health Implications of Raising the Minimum Age of Legal Access to Tobacco Products. 2015.
Chen K, Kandel DB. The natural history of drug use from adolescence to the mid-thirties in a general population sample. American journal of public health. 1995;85(1):41-47.
Fuemmeler B, Lee C-T, Ranby KW, et al. Individual-and community-level correlates of cigarette-smoking trajectories from age 13 to 32 in a US population-based sample. Drug and alcohol dependence. 2013;132(1-2):301-308.
Pollard MS, Tucker JS, Green HD, Kennedy D, Go M-H. Friendship networks and trajectories of adolescent tobacco use. Addictive behaviors. 2010;35(7):678-685.
Health UDo, Services H. Preventing tobacco use among youth and young adults: a report of the Surgeon General. In: Atlanta, GA: US Department of Health and Human Services, Centers for Disease …; 2012.
Livingston G, Sommerlad A, Orgeta V, et al. Dementia prevention, intervention, and care. The Lancet. 2017;390(10113):2673-2734.
Cabeza R, Nyberg L, Park DC. Cognitive neuroscience of aging: Linking cognitive and cerebral aging. Oxford University Press; 2016.
Anstey KJ, Cherbuin N, Herath PM. Development of a new method for assessing global risk of Alzheimer’s disease for use in population health approaches to prevention. Prevention Science. 2013;14(4):411-421.
Sabia S, Marmot M, Dufouil C, Singh-Manoux A. Smoking history and cognitive function in middle age from the Whitehall II study. Archives of internal medicine. 2008;168(11):1165-1173.
Richards M, Jarvis MJ, Thompson N, Wadsworth ME. Cigarette smoking and cognitive decline in midlife: evidence from a prospective birth cohort study. American Journal of Public Health. 2003;93(6):994-998.
Rusanen M, Kivipelto M, Quesenberry CP, Zhou J, Whitmer RA. Heavy smoking in midlife and long-term risk of Alzheimer disease and vascular dementia. Archives of internal medicine. 2011;171(4):333-339.
Bernaards CM, Twisk JW, Snel J, Van Mechelen W, Kemper HC. Is calculating pack-years retrospectively a valid method to estimate life-time tobacco smoking? A comparison between prospectively calculated pack-years and retrospectively calculated pack-years. Addiction. 2001;96(11):1653-1661.
Hughes GH, Cutter G, Donahue R, et al. Recruitment in the coronary artery disease risk development in young adults (CARDIA) study. Controlled clinical trials. 1987;8(4):68-73.
Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. Journal of clinical epidemiology. 1988;41(11):1105-1116.
Auer R, Vittinghoff E, Kiefe C, et al. Change in physical activity after smoking cessation: the C oronary A rtery R isk D evelopment in Y oung A dults (CARDIA) study. Addiction. 2014;109(7):1172-1183.
Pletcher MJ, Hulley BJ, Houston T, Kiefe CI, Benowitz N, Sidney S. Menthol Cigarettes, Smoking Cessation, Atherosclerosis, and Pulmonary Function: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. Archives of Internal Medicine. 2006;166(17):1915-1922.
Schmidt M. Rey auditory verbal learning test: A handbook. Western Psychological Services Los Angeles, CA; 1996.
Wechsler D. Wechsler adult intelligence scale. Psychological corporation New York; 1955.
MacLeod CM. Half a century of research on the Stroop effect: an integrative review. Psychological bulletin. 1991;109(2):163.
Stroop JR. Studies of interference in serial verbal reactions. Journal of Experimental Psychology: General. 1992;121(1):15.
Hoang TD, Reis J, Zhu N, et al. Effect of early adult patterns of physical activity and television viewing on midlife cognitive function. JAMA psychiatry. 2016;73(1):73-79.
McEvoy CT, Guyer H, Langa KM, Yaffe K. Neuroprotective diets are associated with better cognitive function: the health and retirement study. Journal of the American Geriatrics Society. 2017;65(8):1857-1862.
Buhmann B, Rainwater L, Schmaus G, Smeeding TM. Equivalence scales, well-being, inequality, and poverty: sensitivity estimates across ten countries using the Luxembourg Income Study (LIS) database. Review of income and wealth. 1988;34(2):115-142.
Jacobs Jr DR, Hahn LP, Haskell WL, Pirie P, Sidney S. Validity and reliability of short physical activity history: CARDIA and the Minnesota Heart Health Program. Journal of cardiopulmonary rehabilitation. 1989;9(11):448.
Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied psychological measurement. 1977;1(3):385-401.
Pletcher MJ, Varosy P, Kiefe CI, Lewis CE, Sidney S, Hulley SB. Alcohol consumption, binge drinking, and early coronary calcification: findings from the Coronary Artery Risk Development in Young Adults (CARDIA) Study. American Journal of Epidemiology. 2005;161(5):423-433.
Pletcher MJ, Vittinghoff E, Kalhan R, et al. Association between marijuana exposure and pulmonary function over 20 years. Jama. 2012;307(2):173-181.
Howard BV, Gidding SS, Liu K. Association of apolipoprotein E phenotype with plasma lipoproteins in African-American and white young adults: The CARDIA Study. American journal of epidemiology. 1998;148(9):859-868.
Dufouil C, Tzourio C, Brayne C, Berr C, Amouyel P, Alpérovitch A. Influence of apolipoprotein E genotype on the risk of cognitive deterioration in moderate drinkers and smokers. Epidemiology. 2000;11(3):280-284.
Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociological methods & research. 2007;35(4):542-571.
Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological methods & research. 2001;29(3):374-393.
Orlando M, Tucker JS, Ellickson PL, Klein DJ. Developmental trajectories of cigarette smoking and their correlates from early adolescence to young adulthood. Journal of consulting and clinical psychology. 2004;72(3):400.
Andruff H, Carraro N, Thompson A, Gaudreau P, Louvet B. Latent class growth modelling: a tutorial. Tutorials in Quantitative Methods for Psychology. 2009;5(1):11-24.
Ohara T, Ninomiya T, Hata J, et al. Midlife and late-life smoking and risk of dementia in the community: The Hisayama Study. Journal of the American Geriatrics Society. 2015;63(11):2332-2339.
Sabia S, Elbaz A, Dugravot A, et al. Impact of smoking on cognitive decline in early old age: the Whitehall II cohort study. Archives of general psychiatry. 2012;69(6):627-635.
Galanis DJ, Petrovitch H, Launer LJ, Harris TB, Foley DJ, White LR. Smoking history in middle age and subsequent cognitive performance in elderly Japanese-American men: the Honolulu-Asia Aging Study. American Journal of Epidemiology. 1997;145(6):507-515.
Nooyens AC, van Gelder BM, Verschuren WMJAJoPH. Smoking and cognitive decline among middle-aged men and women: the Doetinchem Cohort Study. 2008;98(12):2244-2250.
Ott A, Slooter A, Hofman A, et al. Smoking and risk of dementia and Alzheimer’s disease in a population-based cohort study: the Rotterdam Study. The Lancet. 1998;351(9119):1840-1843.
Reitz C, den Heijer T, van Duijn C, Hofman A, Breteler M. Relation between smoking and risk of dementia and Alzheimer disease: the Rotterdam Study. Neurology. 2007;69(10):998-1005.
Tyas SL, White LR, Petrovitch H, et al. Mid-life smoking and late-life dementia: the Honolulu-Asia Aging Study. Neurobiology of aging. 2003;24(4):589-596.
Chen W-T, Wang P-N, Wang S-J, Fuh J-L, Lin K-N, Liu H-C. Smoking and cognitive performance in the community elderly: A longitudinal study. Journal of geriatric psychiatry and neurology. 2003;16(1):18-22.
Wang C-C, Lu T-H, Liao W-C, et al. Cigarette smoking and cognitive impairment: a 10-year cohort study in Taiwan. Archives of gerontology and geriatrics. 2010;51(2):143-148.
Prince M, Albanese E, Guerchet M, Prina MJWAR. Dementia and risk reduction: an analysis of protective and modifiable factors. 2014:66-83.
McKenzie J, Bhatti L, d’Espaignet ETJGWHO. WHO Tobacco Knowledge Summaries: Tobacco and Dementia. 2014.
Zhong G, Wang Y, Zhang Y, Guo JJ, Zhao YJPo. Smoking is associated with an increased risk of dementia: a meta-analysis of prospective cohort studies with investigation of potential effect modifiers. 2015;10(3):e0118333.
Almeida OP, Garrido GJ, Alfonso H, et al. 24-month effect of smoking cessation on cognitive function and brain structure in later life. Neuroimage. 2011;55(4):1480-1489.
Durazzo TC, Mattsson N, Weiner MW, Initiative AsDN. Smoking and increased Alzheimer’s disease risk: a review of potential mechanisms. Alzheimer’s & Dementia. 2014;10:S122-S145.
Gardener H, Wright CB, Dong C, et al. Ideal cardiovascular health and cognitive aging in the Northern Manhattan Study. Journal of the American Heart Association. 2016;5(3):e002731.
Cao L, Tan L, Wang H-F, et al. Dietary patterns and risk of dementia: a systematic review and meta-analysis of cohort studies. Molecular neurobiology. 2016;53(9):6144-6154.
Singh B, Mielke MM, Parsaik AK, et al. A prospective study of chronic obstructive pulmonary disease and the risk for mild cognitive impairment. JAMA neurology. 2014;71(5):581-588.
Mendelsohn C. Smoking and depression: a review. Australian family physician. 2012;41(5):304.
Knopman DS, Mosley TH, Catellier DJ, Coker LH. Fourteen-year longitudinal study of vascular risk factors, APOE genotype, and cognition: the ARIC MRI Study. Alzheimer’s & Dementia. 2009;5(3):207-214.
Bowman TS, Gaziano JM, Buring JE, Sesso HD. A prospective study of cigarette smoking and risk of incident hypertension in women. Journal of the American College of Cardiology. 2007;50(21):2085-2092.
Yeh H-C, Brancati FL. Smoking cessation and the risk for type 2 diabetes mellitus. Annals of Internal Medicine. 2010;152(11):755-756.
Holbrook J. Cigarette smoking and cardiovascular diseases. A statement for health professionals by a task force appointed by the steering committee of the American Heart Association. Circulation. 1984;70:1114A-A1117.
Jak AJ, Bondi MW, Delano-Wood L, et al. Quantification of five neuropsychological approaches to defining mild cognitive impairment. The American Journal of Geriatric Psychiatry. 2009;17(5):368-375.
Acknowledgements
We would like to thank Tina D. Hoang, MSPH, for her assistance with the manuscript.
Funding
The Coronary Artery Risk Development in Young Adults (CARDIA) Study is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the University of Alabama at Birmingham (HHSN268201800005I & HHSN268201800007I), the Northwestern University (HHSN268201800003I), the University of Minnesota (HHSN268201800006I), and the Kaiser Foundation Research Institute (HHSN268201800004I). The CARDIA Cognitive ancillary study is supported by the National Institute on Aging grant R01 AG063887-01 (NIA Multiple-PI: K Yaffe and S Sidney). This research is also supported by the NIA grant K24 AG031155 (PI: K Yaffe). This manuscript has been reviewed by CARDIA for scientific content.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the U.S. Department of Health and Human Services. The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation of the manuscript. Before submission for publication, the manuscript was approved by the CARDIA Publications and Presentations committee.
Conflict of Interest
Dr. Yaffe reported serving on the Data Safety Monitoring Board for Eli Lilly and several National Institute on Aging-sponsored studies, reported serving on the board of directors for Alector Inc., and reported serving on the Beeson Scientific Advisory Board. No other disclosures were reported.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentations
Partial data were presented as part of a poster presentation (Early Adult to Mid-Life Smoking and Cognitive Function: Findings from the CARDIA Study) at the Alzheimer’s Association International Conference, Los Angeles, CA, July 13–18, 2019.
Supplementary Information
ESM 1
(DOCX 60 kb)
Rights and permissions
About this article
Cite this article
Bahorik, A.L., Sidney, S., Kramer-Feldman, J. et al. Early to Midlife Smoking Trajectories and Cognitive Function in Middle-Aged US Adults: the CARDIA Study. J GEN INTERN MED 37, 1023–1030 (2022). https://doi.org/10.1007/s11606-020-06450-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-020-06450-5