Abstract
Background
Empirical evidence on how health literacy affects diabetes outcomes is inconsistent. The purpose of this meta-analysis was to quantitatively summarize the findings on the associations between health literacy and diabetes knowledge, self-care activities, and glycemic control as disease-related outcomes, with specific focus on the type of health literacy assessment.
Data Sources
Nine databases (MEDLINE, CINAHL, Communication and Mass Media Complete, PsychInfo, PsychArticles, Psychology and Behavioral Sciences Collection, ERIC, Sociology, Embase) were searched for peer-reviewed original research articles published until 31 March 2018.
Methods
Studies with type 1 and/or type 2 diabetes patients aged 18 or older, providing a calculable baseline effect size for functional health literacy and diabetes knowledge, self-care activities, or HbA1C were included.
Results
The meta-analysis includes 61 studies with a total of 18,905 patients. The majority were conducted in the USA, on type 2 diabetes patients, and used the S-TOFHLA as a performance-based or the BHLS as a perception-based measure of functional health literacy. Meta-analytic results show that all three outcomes are related to health literacy. Diabetes knowledge was best predicted by performance-based health literacy measures, self-care by self-report measures, and glycemic control equally by both types of health literacy assessment.
Discussion
Health literacy plays a substantial role in diabetes knowledge. Findings for the role of health literacy in self-care and glycemic control remain heterogeneous, partly due to the type of health literacy assessment (performance- vs. perception-based). This has implications for the use of health literacy measures in clinical settings and original research. This meta-analysis was limited to functional health literacy and, due to the paucity of studies, did not investigate the role of other dimensions including communicative and critical health literacy.
Similar content being viewed by others
INTRODUCTION
Diabetes is a common chronic condition, which can lead to “long-term damage, dysfunction, and failure of different organs, especially the eyes, kidneys, nerves, heart, and blood vessels”.1 In 2015, the disease had a worldwide prevalence of 8.8% and is expected to grow to 10.4% by 2040,2 causing a substantial increment in self-care cost.3 Diabetes requires patients to actively self-manage the disease in their everyday lives. For this reason, the ability to effectively use health information and healthcare services is of great importance. As such, good self-management is closely related to health literacy, defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions”.4 These functional skills have been studied in the context of chronic diseases since the term health literacy first appeared in 1974,5 and their relations to health outcomes, use of healthcare services, and costs have been repeatedly documented.6 Concerning diabetes, a large body of empirical research assessing the relation between health literacy and diabetes-related knowledge, management, and outcomes has been summarized in numerous systematic and narrative reviews with heterogeneous results (e.g.,5,6,7,8,9) For example, Caruso and colleagues,10 in their systematic review of six systematic reviews, concluded that, while the link between health literacy and diabetes knowledge is well-established, inconsistent findings exist for the relationships between health literacy and diabetes-related outcomes. To the best of our knowledge, only one meta-analysis on eight studies11 investigated the role of health literacy in diabetes outcomes, focusing on health-literacy–sensitive interventions. Again, the heterogeneity levels in the final effect size were very high. A possible explanation is the variety of definitions and measurements of health literacy.12, 13 In clinical settings, health literacy has been traditionally assessed with word recognition tests like the Rapid Estimate of Adult Literacy in Medicine (REALM12) or combined health literacy and numeracy tests like the Short Test of Functional Health Literacy (S-TOFHLA13). These tests measure patients’ performance, i.e., basic comprehension, reading, and numeracy skills. Despite the introduction of shorter versions, they require time and clinical staff to assist in the administration. To overcome these shortcomings, brief screening tools have been developed and validated including the Brief Health Literacy Screening questions (BHLS14). These self-report tools measure patients’ perception of their (in-)abilities to function in healthcare settings covering comprehension, navigation, and writing skills. Furthermore, disease-specific literacy (e.g., Literacy Assessment for Diabetes (LAD)15) and numeracy tests (e.g., Diabetes Numeracy Test (DNT)16) have been proposed following the notion that measuring health literacy will be best achieved where content and context are well defined.12 In a previous review of four studies including both performance-based and self-report health literacy measures, Kiechle and colleagues did not find any differential effects of measurement type on self-reported health outcomes including diabetes management.17 However, the small number of “fair” rated studies did not allow a quantitative synthesis or more detailed subgroup analyses. That said, the present meta-analysis wants to shed light on the role of health literacy in diabetes-related knowledge, self-care, and glycemic control,18 taking into account variations in functional health literacy assessments.
METHODS
We conducted this meta-analysis according to the MOOSE guidelines19 and, in part, the PRISMA guidelines.20
Study Sources and Searches
The first two authors searched in nine electronic databases up to 31 March 2018: MEDLINE, CINAHL, Communication and Mass Media Complete, Psychology and Behavioral Sciences Collection, PsychInfo, ERIC and Sociology, Embase, and PsychArticles. The detailed search strategy and keywords are reported in Appendix 1. We carried out an additional hand search by going through the reference list of relevant review articles identified through the database search and scanning the first 100 Google Scholar entries.
Study Selection
After duplicates were removed, the first two authors independently completed a title and abstract screening. We included only studies according to the following criteria: (1) written in English, (2) published in a peer review journal, (3) including only adult patients (≥ 18 years of age) with (4) type 1 or type 2 diabetes, (5) with at least one validated measure of health literacy or numeracy and one measure of diabetes knowledge or glycemic control (HbA1C) or self-care activities, and (6) an outcome which could be converted into an effect size. We excluded studies with children or adolescent populations or gestational diabetics. We further excluded conference abstracts, theses, books, or book sections. In case of longitudinal or intervention studies, we extracted only baseline measures. To obtain a measure of interrater reliability, we calculated the Cohen’s kappa statistic for title and abstract screening. If at least one of the two coders decided to retain an article, we included it in the full-text screening. Discrepancies after full-text screening were resolved by consensus.
Data Extraction
For each included study, we extracted information about the article (first author, year of publication, journal title), the study (country where the study was conducted, study design, sample size, type of health literacy measure), and principal outcomes (any data assessing the association between health literacy and diabetes knowledge, self-care, and glycemic control, which could be converted into an effect size). Finally, we collected sample characteristics including proportion of female, age, education level, ethnicity, type of diagnosis (diabetes type 1 or 2), presence of comorbidities, BMI, insulin use, diabetes duration, past diabetes education, social support, and insurance status.
Quality Assessment
Measures of health literacy, diabetes knowledge, and self-care activities require patients’ capacity to understand and respond to questions or tasks. Thus, as a form of quality assessment, we checked whether studies explicitly mentioned limited language proficiency, psychological problems, cognitive, vision, or hearing impairment of patients as an exclusion criterion. We used this quality information in subgroup analyses and tested whether there was a difference in the effect size between studies with good and poor quality.
Data Synthesis and Analysis
We conducted the meta-analysis using the “esc”21 and “meta”22 packages in R statistical software. We used Fisher’s r to z transformation as a measure of effect size, with results converted back to the r correlation coefficient. Since the raw data were heterogeneous, we used different transformation formulas23, 24 to compute the effect size. The analyses were implemented using the inverse-variance method with a random effects model and Hartung–Knapp–Sidik–Jonkman adjustment,25 which allows to control for the error rates of the effect size due to heterogeneity. Moreover, we use the restricted maximum-likelihood estimator (REML) to estimate the between-study variance τ2 and the I2 statistic26,27,28 to describe the heterogeneity of the effect size. Potential publication biases were assessed via Egger’s regression test for funnel plot asymmetry using the mixed-effects meta-regression model.29 To explain possible heterogeneity in the effect sizes, we implemented influence analyses (using the leaving-one-out method), meta-regression, and subgroup analyses. We performed sensitivity analyses of our results to potential moderators by a combination of stratified analyses and meta-regression modeling. This included distinguishing studies according to the type of health literacy or numeracy measure (performance-based or self-report, including a numeracy section or not, being diabetes specific or not). We also considered different sociodemographic and study-specific characteristics in subgroup analyses. Notably, we performed meta-regression analyses only for outcomes that had a sufficient number of studies, ideally at least ten.28
Role of the Funding Source
The authors received no specific funding for this meta-analysis.
RESULTS
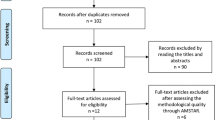
The initial database and hand search returned 2970 publications, of which 1491 were duplicates or no peer-reviewed journal articles. After title and abstract screening of 1479 records (Cohen’s kappa = 0.923), we assessed 113 full-text articles for eligibility. We excluded 52 articles resulting in a meta-analysis of 61 studies with 58 unique samples. The study selection process and the reasons for exclusion after full-text screening are reported in the PRISMA flowchart (Fig. 1).
Study Characteristics
The present meta-analysis is based on 61 studies30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90 with 58 unique samples. Overall, the analytical sample amounts to 18,905 patients. Of all studies, 51 used a cross-sectional design. Thirty-nine were conducted in North America (36 in the USA and 3 in Canada), 8 in Asia, 7 in Middle Eastern countries, and 4 in Europe. The sample size per study ranged from 36 to 2564 patients with diabetes type 1 (n = 1), type 2 (n = 35), type 1 and 2 (n = 16), or unspecified diabetes (n = 9). Nineteen studies reported on patients’ comorbidities including hypertension, retinopathy, or hyperlipidemia. Concerning our measures of interest, 33 studies assessed patients’ functional health literacy with a performance-based measure including the S-TOFHLA (n = 16) or adapted versions (n = 2), TOFHLA (n = 2), REALM (n = 9) or its revised version (n = 1), or other tests (n = 3). Another 18 studies used self-report measures such as the BHLS (n = 9), FCCHL (n = 5), or other partly ad hoc created measures (n = 4). Of all health literacy measures, 5 were diabetes-specific tests (n = 3) or diabetes-specific self-report scales (n = 2). Numeracy was assessed in 11 studies with performance-based measures including the DNT (n = 7), the NVS (n = 3), or the numeracy section of the WRAT-3R (n = 1). HbA1C was measured in 43 out of 61 studies. Twenty-seven studies assessed diabetes self-care activities using the SDSCA or subdimensions of this scale being used in 19 studies. Diabetes-related knowledge was measured in 26 studies either with the DKT (n = 9), the SKILLD instrument (n = 7), the DKQ (n = 3), or other mostly ad hoc created instruments (n = 7). Limited language proficiency or cognitive, vision, or hearing impairment of patients as an exclusion criterion was applied in 47 studies. Detailed information about each study and measures including references are reported in Appendices Table 2 and 3.
Health Literacy and Diabetes Knowledge
Higher levels of health literacy were significantly associated with better diabetes knowledge (n = 20, r = 0.308, p < 0.001, I2 = 85%). No particular study influenced the overall heterogeneity. However, studies using a performance-based test had a significantly (p = 0.023) larger effect size (n = 16, r = 0.339, p < 0.001) than studies using self-report measures (n = 4, r = 0.193, p = 0.030) (see Table 1 and Fig. 2). Using health literacy tests with a numeracy section led to a significantly (p = 0.002) smaller effect size (n = 8, r = 0.232, p = 0.002) compared to tests without (n = 8, r = 0.437, p < 0.001). Only one study used a diabetes-specific health literacy measure58; hence, it could not be compared with other studies using unspecific health literacy measures. Although the meta-analysis on numeracy and diabetes knowledge showed a large positive significant correlation (n = 6, r = 0.486, p = 0.001), the heterogeneity level was very high (I2 = 91%). Leaving out the study by Huizinga,49 the original validation study of the DNT in type 1 and 2 diabetic patients, decreased the heterogeneity level to 0%, yet the correlation remained rather unaffected (r = 0.419, p < 0.0001).
Health Literacy and Diabetes Self-Care
Higher levels of health literacy were not associated with more frequent self-care activities (n = 11, r = 0.052, p = 0.117, I2 = 51%). Leaving out the study by Inoue 50 decreased the heterogeneity level to 25%; however, the total effect size remained nonsignificant. Subgroup analyses revealed a significant (p = 0.025) difference related to the type of test: in studies including self-report health literacy measures, the overall association with self-care activities was significant and positive (n = 6, r = 0.095, p = 0.045), while no such association was found for studies with performance-based tests. Subgroup analyses did not show any differences between the effect sizes of studies using diabetes-specific and nonspecific measures. Only one study used a diabetes-specific health literacy measure and only one a health literacy test without a numeracy section42; hence, subgroup comparison could not be conducted. Moreover, there was an insufficient number of studies (n = 1)31 to perform a meta-analysis on numeracy and diabetes self-care. Finally, the meta-analyses on health literacy and single self-care activities (i.e., diet, blood monitoring, exercise, medication adherence, and foot care) did not reveal any significant relationships. However, subgroup analyses for single self-care activities showed that the correlations with exercise and with foot care were significantly positive in studies using self-report measures (n = 6, r = 0.098, p < 0.001, I2 = 0% for exercise and n = 3, r = 0.274, I2 = 92%, p = 0.023 for foot care) (see Table 1).
Health Literacy and Glycemic Control
Higher levels of health literacy were associated with lower levels of HbA1C (n = 36, r = − 0.048, p = 0.027, I2 = 71%). Leaving out the study by Niknami67 decreased the I2 level to 51% (r = − 0.030, p = 0.065). Subgroup analyses revealed that studies with performance-based measures had a significant effect size (n = 24, r = − 0.046, p = 0.034, I2 = 54%), while those using self-report measures, comprised of less than half as many studies, were not significant (n = 12, r = − 0.037, p = 0.439, I2 = 85%). However, the difference between the two types of measurement was not statistically significant (p = 0.858) (see Table 1 and Fig. 3). There were no differences in effect sizes related to the type of performance-based health literacy measure, i.e., including a numeracy section or being diabetes-specific. Furthermore, the pooled effect size of the meta-analysis on numeracy and glycemic control was not significant (n = 8, r = − 0.018, p = 0.653).
Additional Subgroup Analyses
Considering other potential moderators, primarily related to the study design, we found the following significant subgroup differences: the correlation between health literacy and diabetes knowledge was positive only for studies conducted in North and South America (n = 15, r = 0.351, p < 0.001, I2 = 79%). Furthermore, health literacy was negatively related to HbA1C in studies conducted only with diabetes type 2 patients (n = 23, r = − 0.063, p = 0.044, I2 = 77%) and a higher proportion of low-educated (n = 30, β = − 0.002, p = 0.022) and uninsured patients (n = 15, β = − 0.002, p = 0.043) impacted on the final effect. Detailed results on subgroup analyses are available from the first author upon request.
Publication Biases
Egger’s tests for funnel plot asymmetry did not reveal any publication bias, except for the meta-analysis on health literacy and diabetes knowledge (Egger’s regression test result: t = 2.744, p = 0.013).
DISCUSSION
Based on 61 studies, our meta-analysis is the first to summarize empirical evidence on the role of health literacy in diabetes-related knowledge, self-care, and glycemic control, taking into account different types of health literacy assessment.
We found that health literacy had a small though significant effect on better glycemic control, as measured using the HbA1C. The effect was even stronger when health literacy was assessed by performance-based measures such as the S-TOFHLA or REALM. Thus, clinicians interested in the assessment of health literacy to better predict glycemic control in their patients should rely on performance-based measures. To date, these are primarily available for functional health literacy and do not capture more advanced skills including navigation, communicative, and critical skills. Another finding from subgroup analyses is that the more patients are in need, because of low education and missing insurance, the stronger is the relationship between health literacy and HbA1C. One possible explanation is that general education and insurance status function as a “buffer,” and the lack of those two stresses even more the importance of an adequate level of health literacy to obtain good diabetes outcomes.
In a similar fashion, we found that health literacy was positively related to diabetes knowledge, echoing findings from systematic reviews on the two concepts.10 Again, the relationship was stronger when performance-based tests were used exclusively or in addition to other measures, as compared to measures based on (self-)perception. This is an important finding as research has previously shown that diabetes knowledge is related with successful self-management and health outcomes.91, 92
On the contrary, we found that health literacy had a positive impact on self-care activities only for studies that assessed literacy with perception-based measures. The same result was found in subgroup analyses for two specific self-care activities: exercise and food care, but not for diet and blood monitoring. The fact that all our measures of self-care activities are also self-reports suggests that such measures assess patients’ confidence in their capacity to comprehend and use medical materials, rather than their actual ability. Conceptually, confidence or, in other terms, self-efficacy differs from health literacy93 and has been found to be associated with diabetes care across different health literacy levels.94 Additionally, self-report data are prone to systematic biases, including patients’ difficulties in critical self-assessment and social desirability bias,95 especially in clinical assessment situations where patients may feel ashamed of their limited health literacy.96 It could also be that, as both the health literacy and the self-care measures are based on self-perception, the two may be linked by shared biases, i.e., that the reasons why a person misjudges his ability to understand nutrition rules might be the same as the reasons why he misperceives his factual nutrition behavior.
Based on these findings, for clinicians interested in health literacy screenings of patients, the question whether to use performance-based or self-report measures cannot be answered by a simple choice. Much depends on which diabetes outcome(s) they are concerned with. Glycemic control, the most studied outcome, is predicted by both performance-based and self-report health literacy measures, although performance-based measures tend to be the better predictor. Diabetes knowledge is best predicted by performance-based assessments of health literacy and numeracy. Self-care activities, usually reported by patients, are best predicted by self-report health literacy; however, this could be due to the nature of self-care information, which is also self-reported. Thus, one strong point which is evident is the following: if previously self-reported and performance-based measures were considered equally adequate in assessing health literacy, we can now assert that they are not. This point is important when clinicians have to decide which health literacy measure to use.
Given these findings, we call for more research on health literacy in diabetes outcomes. First, we recommend to invest in the development and validation of diabetes-specific performance-based measures of health literacy capturing more advanced skills beyond functional health literacy skills. The paucity of studies using diabetes-specific health literacy and numeracy measures, beyond mere reading and comprehension skills, does not yet allow a quantitative synthesis of the evidence on health literacy in diabetes management. Second, for researchers interested in the evaluation of diabetes interventions, performance-based literacy assessments should be used; they show strong effect sizes with diabetes knowledge and, to a lesser extent, glycemic control, and they overcome potential bias introduced by self-report measures. We also recommend to invest in the assessment of diabetes numeracy to produce more evidence on the relationship with different diabetes outcomes, especially self-care activities. Additionally, more research is needed to better understand the difference between diabetes-specific and general health literacy measures. In particular, considering that usually performance-based measures are not diabetes specific, the development of new disease-specific functional health literacy measures could be a promising route for future studies for improving healthcare.
Our study has some limitations. We did not explore any differences among functional, communicative, and critical health literacy, given the limited number of studies reporting diabetes outcomes for all three dimensions of health literacy. Furthermore, it was not possible to evaluate other important factors, such as depressive symptoms or self-efficacy, due to the paucity of studies including these variables. Moreover, although we could explain a significant portion of study heterogeneity with different types of health literacy assessments, heterogeneity may also be affected by differences in the studies’ inclusion criteria and methodologies as well as patients’ comorbidities.
In sum, all three diabetes outcomes (knowledge, self-care, glycemic control) are related to health literacy. Knowledge seems more responsive to performance-based, self-care to perception-based, and glycemic control to both measures, with a preference for performance-based tools. In other words, when the outcome is assessed by a “soft” criterion such as self-reported self-care behavior, the relationship appears to be generated more by the perception-based measure of health literacy, while an outcome assessment based on “hard” criteria, e.g., blood sugar level, with reservations also a person’s diabetes knowledge, appears to react more strongly to more objective performance-based measures.
References
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2011;34 (Suppl 1):S62–9
Ogurtsova K, Fernandes JD da R, Huang Y, Linnenkamp U, Guariguata L, Cho NH, et al. IDF diabetes atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract 2017;128:40–50
Huang ES, Basu A, O’Grady M, Capretta JC. Projecting the future diabetes population size and related costs for the U.S. Diabetes Care 2009;32(12):2225–9
Ratzan S, Parker R. Introduction. In National Library of Medicine Current Bibliographies in Medicine: Health Literacy. Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services, 2000
Simonds S. Health education as social policy. Health Educ Monogr 1974;21:1–10
Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155(2):97–107
Al Sayah F, Williams B, Johnson JA. Measuring health literacy in individuals with diabetes: a systematic review and evaluation of available measures. Health Educ Behav Off Publ Soc Public Health Educ 2013;40(1):42–55
Bailey SC, Brega AG, Crutchfield TM, Elasy T, Herr H, Kaphingst K, et al. Update on health literacy and diabetes. Diabetes Educ 2014;40(5):581–604
Cavanaugh KL. Health literacy in diabetes care: explanation, evidence and equipment. Diabetes Manag Lond Engl 2011;1(2):191–9
Caruso R, Magon A, Baroni I, Dellafiore F, Arrigoni C, Pittella F, et al. Health literacy in type 2 diabetes patients: a systematic review of systematic reviews. Acta Diabetol 2018;55(1):1–12
Kim SH, Lee A. Health-literacy-sensitive diabetes self-management interventions: a systematic review and meta-analysis. Worldviews Evid Based Nurs 2016;13(4):324–33
Frisch A-L, Camerini L, Diviani N, Schulz PJ. Defining and measuring health literacy: how can we profit from other literacy domains? Health Promot Int 2012;27(1):117–26
Lee E-H, Kim C-J, Lee J, Moon SH. Self-administered health literacy instruments for people with diabetes: systematic review of measurement properties. J Adv Nurs 2017;73(9):2035–48
Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med 1993;25(6):391–5
Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults. J Gen Intern Med 1995;10(10):537–41
Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med 2008;23(5):561–6
Kiechle ES, Bailey SC, Hedlund LA, Viera AJ, Sheridan SL. Different measures, different outcomes? A systematic review of performance-based versus self-reported measures of health literacy and numeracy. J Gen Intern Med 2015;30(10):1538–46
Lyons TJ, Basu A. Biomarkers in diabetes: hemoglobin a1c, vascular and tissue markers. Transl Res 2012;159(4):303–12
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 2000;283(15):2008–12
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;349:g7647
Lüdecke D. Package “esc”: effect size computation for meta analysis [Internet]. 2018. Available from https://github.com/strengejacke/esc Accessed 18 July 2018
Schwarzer G, Carpenter JR, Rücker G. Meta-analysis with R (Use R!). Cham, Switzerland, Springer International Publishing, 2015
Peterson RA, Brown SP. On the use of beta coefficients in meta-analysis. J Appl Psychol 2005;90(1):175–81
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014;14:135
IntHout J, Ioannidis JP, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol 2014;14:25
Borenstein M, Hedges L, Rothstein H. Meta-analysis: fixed effect vs. random effects. [Online White Paper] Available from https://www.meta-analysis.com/downloads/Meta-analysis%20fixed%20effect%20vs%20random%20effects.pdf. Accessed 11 December 2018
Ried K. Interpreting and understanding meta-analysis graphs—a practical guide. Aust Fam Physician 2006;35(8):635–8
Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, UK, Wiley, 2008
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629–34
Al Sayah F, Majumdar SR, Johnson JA. Association of inadequate health literacy with health outcomes in patients with type 2 diabetes and depression: secondary analysis of a controlled trial. Can J Diabetes 2015;39(4):259–65
Al Sayah F, Majumdar SR, Egede LE, Johnson JA. Associations between health literacy and health outcomes in a predominantly low-income African American population with type 2 diabetes. J Health Commun 2015;20(5):581–8
Al Sayah F, Soprovich A, Qiu W, Edwards AL, Johnson JA. Diabetic foot disease, self-care and clinical monitoring in adults with type 2 diabetes: the Alberta’s caring for diabetes (ABCD) COHORT STUDY. Can J Diabetes 2015;39 Suppl 3:S120–126
Al Sayah F, Williams B, Pederson JL, Majumdar SR, Johnson JA. Health literacy and nurses’ communication with type 2 diabetes patients in primary care settings. Nurs Res 2014;63(6):408–17
Alghodaier H, Jradi H, Mohammad NS, Bawazir A. Validation of a diabetes numeracy test in Arabic. PLOS ONE 2017;12(5):e0175442
Bains S., Osborn C.Y., Egede L.E. Association of health literacy and diabetes self-care utilizing the information-motivationbehavioral skills model. J Investig Med 2010;58(2):481
Bohanny W, Wu S-FV, Liu C-Y, Yeh S-H, Tsay S-L, Wang T-J. Health literacy, self-efficacy, and self-care behaviors in patients with type 2 diabetes mellitus. J Am Assoc Nurse Pract 2013;25(9):495–502
Bowen ME, Cavanaugh KL, Wolff K, Davis D, Gregory B, Rothman RL. Numeracy and dietary intake in patients with type 2 diabetes. Diabetes Educ 2013;39(2):240–7
Brega AG, Ang A, Vega W, Jiang L, Beals J, Mitchell CM, et al. Mechanisms underlying the relationship between health literacy and glycemic control in American Indians and Alaska Natives. Patient Educ Couns 2012;88(1):61–8
Cavanaugh K, Huizinga MM, Wallston KA, Gebretsadik T, Shintani A, Davis D, et al. Association of numeracy and diabetes control. Ann Intern Med 2008;148(10):737–46
Chahardah-Cherik S, Gheibizadeh M, Jahani S, Cheraghian B. The relationship between health literacy and health promoting behaviors in patients with type 2 diabetes. Int J Community Based Nurs Midwifery 2018;6(1):65–75
Chen G-D, Huang C-N, Yang Y-S, Lew-Ting C-Y. Patient perception of understanding health education and instructions has moderating effect on glycemic control. BMC Public Health 2014;14:683
Coccaro EF, Drossos T, Phillipson L. HbA1c levels as a function of emotional regulation and emotional intelligence in patients with type 2 diabetes. Prim Care Diabetes 2016;10(5):334–41
DeWalt DA, Boone RS, Pignone MP. Literacy and its relationship with self-efficacy, trust, and participation in medical decision making. Am J Health Behav 2007;31(Suppl1):S27–35
Eyuboglu E, Schulz PJ. Do health literacy and patient empowerment affect self-care behaviour? A survey study among Turkish patients with diabetes. BMJ Open 2016;6(3):e010186
Ferguson MO, Long JA, Zhu J, Small DS, Lawson B, Glick HA, et al. Low health literacy predicts misperceptions of diabetes control in patients with persistently elevated a1c. Diabetes Educ 2015;41(3):309–19
Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns 2003;51(3):267–75
Gerber B.S., Brodsky I.G., Lawless K.A., Smolin L.I., Arozullah A.M., Smith E.V., et al. Implementation and evaluation of a low-literacy diabetes education computer multimedia application. Diabetes Care 2005;28(7):1574–80
Gordilho Souza J, Apolinario D, Magaldi RM, Busse AL, Campora F, Jacob-Filho W. Functional health literacy and glycaemic control in older adults with type 2 diabetes: a cross-sectional study. BMJ Open 2014;4(2):e004180
Huizinga MM, Elasy TA, Wallston KA, Cavanaugh K, Davis D, Gregory RP, et al. Development and validation of the Diabetes Numeracy Test (DNT). BMC Health Serv Res 2008;8:96
Inoue M, Takahashi M, Kai I. Impact of communicative and critical health literacy on understanding of diabetes care and self-efficacy in diabetes management: a cross-sectional study of primary care in Japan. BMC Fam Pract 2013;14:40
Ishikawa H, Takeuchi T, Yano E. Measuring functional, communicative, and critical health literacy among diabetic patients. Diabetes Care 2008;31(5):874–9
Jeppesen KM, Hull BP, Raines M, Miser WF. A validation study of the Spoken Knowledge in Low Literacy in Diabetes Scale (SKILLD). J Gen Intern Med. 2012;27(2):207–12
Jihye Jeong, Namhee Park, So Young Shin. The influence of health literacy and diabetes knowledge on diabetes self-care activities in Korean low-income elders with diabetes. J Korean Acad Community Health Nurs Jiyeog Sahoe Ganho Hakoeji 2014;25(3):217–24
Juul L, Rowlands G, Maindal HT. Relationships between health literacy, motivation and diet and physical activity in people with type 2 diabetes participating in peer-led support groups. Prim Care Diabetes 2018;12(4):331–7
Kim S, Love F, Quistberg DA, Shea JA. Association of health literacy with self-management behavior in patients with diabetes. Diabetes Care 2004;27(12):2980–2
Lai AY, Ishikawa H, Kiuchi T, Mooppil N, Griva K. Communicative and critical health literacy, and self-management behaviors in end-stage renal disease patients with diabetes on hemodialysis. Patient Educ Couns 2013;91(2):221–7
Lee Y-J, Shin S-J, Wang R-H, Lin K-D, Lee Y-L, Wang Y-H. Pathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 diabetes mellitus. Patient Educ Couns 2016;99(2):287–94
Leung AY, Lou VW, Cheung MK, Chan SS, Chi I. Development and validation of Chinese health literacy scale for diabetes. J Clin Nurs 2013;22(15/16):2090–9
Mancuso JM. Impact of health literacy and patient trust on glycemic control in an urban USA population. Nurs Health Sci. 2010;12(1):94–104
Maneze D, Everett B, Astorga C, Yogendran D, Salamonson Y. The influence of health literacy and depression on diabetes self-management: a cross-sectional study. J Diabetes Res 2016;2016:3458969
Mayberry LS, Rothman RL, Osborn CY. Family members’ obstructive behaviors appear to be more harmful among adults with type 2 diabetes and limited health literacy. J Health Commun 2014;19:132–43
McCleary-Jones V. Health Literacy and its association with diabetes knowledge, self-efficacy and disease self-management among African Americans with diabetes mellitus. ABNF J 2011;22(2):25–32
Miser WF, Jeppesen KM, Wallace LS. Clinical utility of a brief screen for health literacy and numeracy among adults with diabetes mellitus. Fam Med 2013;45(6):417–23
Morris NS, MacLean CD, Littenberg B. Literacy and health outcomes: a cross-sectional study in 1002 adults with diabetes. BMC Fam Pract 2006;7:49
Morris NS, MacLean CD, Littenberg B. Change in health literacy over 2 years in older adults with diabetes. Diabetes Educ 2013;39(5):638–46
Newsome C., Mallawaarachchi I., Garcia J., Ray G. Association between health literacy and diabetes control in a pharmacist-run disease state management clinic. Cogent Med 2016;3: 1269628
Niknami M, Mirbalouchzehi A, Zareban I, Kalkalinia E, Gasem Rikhtgarha, Hosseinzadeh H. Association of health literacy with type 2 diabetes mellitus self-management and clinical outcomes within the primary care setting of Iran. Aust J Prim Health 2018;24(2):162–70
Osborn CY, Cavanaugh K, Wallston KA, Rothman RL. Self-efficacy links health literacy and numeracy to glycemic control. J Health Commun 2010;15:146–58
Osborn CY, Cavanaugh K, Wallston KA, White RO, Rothman RL, Osborn CY, et al. Diabetes numeracy: an overlooked factor in understanding racial disparities in glycemic control. Diabetes Care 2009;32(9):1614–9
Powell CK, Hill EG, Clancy DE. The relationship between health literacy and diabetes knowledge and readiness to take health actions. Diabetes Educ 2007;33(1):144–51
Radwan M, Elsous A, Al-Sharif H, Abu Mustafa A. Glycemic control among primary care patients with type 2 diabetes mellitus in the Gaza Strip, Palestine. Ther Adv Endocrinol Metab 2018;9(1):3–14
Reisi M, Mostafavi F, Javadzade H, Mahaki B, Tavassoli E, Sharifirad G. Impact of health literacy, self-efficacy, and outcome expectations on adherence to self-care behaviors in Iranians with type 2 diabetes. Oman Med J 2016;31(1):52–9
Rothman RL, DeWalt DA, Malone R, Bryant B, Shintani A, Crigler B, et al. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA 2004;292(14):1711–6
Rothman RL, Malone R, Bryant B, Wolfe C, Padgett P, DeWalt DA, et al. The spoken knowledge in low literacy in diabetes scale: a diabetes knowledge scale for vulnerable patients. Diabetes Educ 2005;31(2):215–24
Saeed H, Saleem Z, Naeem R, Shahzadi I, Islam M. Impact of health literacy on diabetes outcomes: a cross-sectional study from Lahore, Pakistan. Public Health 2018;156:8–14
Schillinger D, Barton LR, Karter AJ, Wang F, Adler N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep Wash DC 1974 2006;121(3):245–54
Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, et al. Association of health literacy with diabetes outcomes. JAMA 2002;288(4):475–82
Schillinger D, Piette J, Grumbach K, Wang F, Wilson C, Daher C, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med 2003;163(1):83–90
Swavely D, Vorderstrasse A, Maldonado E, Eid S, Etchason J. Implementation and evaluation of a low health literacy and culturally sensitive diabetes education program. J Healthc Qual Promot Excell Healthc 2014;36(6):16–23
Tang YH, Pang SMC, Chan MF, Yeung GSP, Yeung VTF. Health literacy, complication awareness, and diabetic control in patients with type 2 diabetes mellitus. J Adv Nurs 2008;62(1):74–83
Thabit H, Shah S, Nash M, Brema I, Nolan JJ, Martin G. Globalization, immigration and diabetes self-management: an empirical study amongst immigrants with type 2 diabetes mellitus in Ireland. QJM Mon J Assoc Physicians 2009;102(10):713–20
van der Heide I, Uiters E, Rademakers J, Struijs JN, Schuit AJ, Baan CA. Associations among health literacy, diabetes knowledge, and self-management behavior in adults with diabetes: results of a Dutch cross-sectional study. J Health Commun 2014;19:115–31
Wallace AS, Seligman HK, Davis TC, Schillinger D, Arnold CL, Bryant-Shilliday B, et al. Literacy-appropriate educational materials and brief counseling improve diabetes self-management. Patient Educ Couns 2009;75(3):328–33
White RO, Osborn CY, Gebretsadik T, Kripalani S, Rothman RL. Health literacy, physician trust, and diabetes-related self-care activities in Hispanics with limited resources. J Health Care Poor Underserved 2013;24(4):1756–68
White RO, Osborn CY, Gebretsadik T, Kripalani S, Rothman RL, White RO 3rd, et al. Development and validation of a Spanish diabetes-specific numeracy measure: DNT-15 Latino. Diabetes Technol Ther 2011;13(9):893–8
Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med 1998;158(2):166–72
Woodard LD, Landrum CR, Amspoker AB, Ramsey D, Naik AD. Interaction between functional health literacy, patient activation, and glycemic control. Patient Prefer Adherence 2014;8:1019–24
Yamashita T, Kart CS. Is diabetes-specific health literacy associated with diabetes-related outcomes in older adults? J Diabetes 2011;3(2):138–46
Young CF, Yun K, Kang E, Shubrook JH, Dugan JA. Correlations between A1C and diabetes knowledge, diabetes numeracy, and food security in a vulnerable type 2 diabetes population. Diabetes Spectr 2018;31(2):177–83
Zuercher E, Diatta ID, Burnand B, Peytremann-Bridevaux I. Health literacy and quality of care of patients with diabetes: a cross-sectional analysis. Prim Care Diabetes 2017;11(3):233–40
Gomes MB, Santos DC, Pizarro MH, Barros BSV, de Melo LGN, Negrato CA. Does knowledge on diabetes management influence glycemic control? A nationwide study in patients with type 1 diabetes in Brazil. Patient Prefer Adherence 2018;12:53–62
Kueh YC, Morris T, Ismail A-A-S. The effect of diabetes knowledge and attitudes on self-management and quality of life among people with type 2 diabetes. Psychol Health Med 2017;22(2):138–44
Schulz PJ, Nakamoto K. Health literacy and patient empowerment in health communication: the importance of separating conjoined twins. Patient Educ Couns 2013;90(1):4–11
Sarkar U, Fisher L, Schillinger D Is Self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care 2006;29(4):823–9
Althubaiti A. Information bias in health research: definition, pitfalls, and adjustment methods. J Multidiscip Healthc 2016;9:211–7
Parikh NS, Parker RM, Nurss JR, Baker DW, Williams MV. Shame and health literacy: the unspoken connection. Patient Educ Couns 1996;27(1):33–9
Author information
Authors and Affiliations
Contributions
L.M., A.L.C., and P.J.S. formulated the research questions and defined the search terms. L.M. carried out the electronic searches. L.M. and A.L.C. carried out the search process, the methodological assessment, and the extraction of studies information. L.M. carried out the meta-analysis. All authors were involved in writing and reviewing the final manuscript.
Corresponding author
Ethics declarations
Not applicable.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marciano, L., Camerini, AL. & Schulz, P.J. The Role of Health Literacy in Diabetes Knowledge, Self-Care, and Glycemic Control: a Meta-analysis. J GEN INTERN MED 34, 1007–1017 (2019). https://doi.org/10.1007/s11606-019-04832-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-019-04832-y