ABSTRACT
OBJECTIVES
The current review examines the effectiveness of simulation-based medical education (SBME) for training health professionals in cardiac physical examination and examines the relative effectiveness of key instructional design features.
METHODS
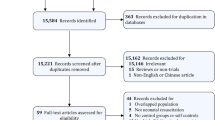
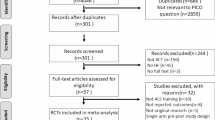
Data sources included a comprehensive, systematic search of MEDLINE, EMBASE, CINAHL, PsychINFO, ERIC, Web of Science, and Scopus through May 2011. Included studies investigated SBME to teach health profession learners cardiac physical examination skills using outcomes of knowledge or skill. We carried out duplicate assessment of study quality and data abstraction and pooled effect sizes using random effects.
RESULTS
We identified 18 articles for inclusion. Thirteen compared SBME to no-intervention (either single group pre-post comparisons or SBME added to other instruction common to all learners, such as traditional bedside teaching), three compared SBME to other educational interventions, and two compared two SBME interventions. Meta-analysis of the 13 no-intervention comparison studies demonstrated that simulation-based instruction in cardiac auscultation was effective, with pooled effect sizes of 1.10 (95 % CI 0.49–1.72; p < 0.001; I2 = 92.4 %) for knowledge outcomes and 0.87 (95 % CI 0.52–1.22; p < 0.001; I2 = 91.5 %) for skills. In sub-group analysis, hands-on practice with the simulator appeared to be an important teaching technique. Narrative review of the comparative effectiveness studies suggests that SBME may be of similar effectiveness to other active educational interventions, but more studies are required.
LIMITATIONS
The quantity of published evidence and the relative lack of comparative effectiveness studies limit this review.
CONCLUSIONS
SBME is an effective educational strategy for teaching cardiac auscultation. Future studies should focus on comparing key instructional design features and establishing SBME’s relative effectiveness compared to other educational interventions.




Similar content being viewed by others
REFERENCES
Conn RD, O’Keefe JH. Cardiac physical diagnosis in the digital age: an important but increasingly neglected skill (from stethoscopes to microchips). Am J Cardiol. 2009;104(4):590–5.
Mangione S, Nieman LZ, Gracely E, Kaye D. The teaching and practice of cardiac auscultation during internal medicine and cardiology training: a nationwide survey. Ann Intern Med. 1993;119(1):47.
Vukanovic-Criley JM, Criley S, Warde CM, Boker JR, Guevara-Matheus L, Churchill WH, et al. Competency in cardiac examination skills in medical students, trainees, physicians, and faculty: a multicenter study. Arch Intern Med. 2006;166(6):610–6.
Gordon MS, Ewy GA, Felner JM, Forker AD, Gessner I, McGuire C, et al. Teaching bedside cardiologic examination skills using “Harvey”, the cardiology patient simulator. Med Clin North Am. 1980;64(2):305–13.
McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med. 2011;86(6):706–11.
Passiment M, Sacks H, Huang G. Medical Simulation in Medical Education: Results of an AAMC Survey. Association of American Medical Colleges. Washington DC: 2011 Sept. pp.1-48.
Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011;306(9):978–88.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12.
Reed DA, Cook DA, Beckman TJ, Levine RB, Kern DE, Wright SM. Association between funding and quality of published medical education research. JAMA. 2007;298(9):1002–9.
Issenberg SB, McGaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27(1):10–28.
Borenstein M. Effect sizes for continuous data. In: Cooper H, Hedges LV, Valentine JC, eds. The Handbook of Research Synthesis and Meta-Analysis. 2nd ed. New York: Russell Sage; 2009.
Morris SB, DeShon RP. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychol Methods. 2002;7(1):105–25.
Hunter J, Schmidt F. Methods of Meta-Analysis: Correcting Error and Bias in Research Findings. Thousand Oaks: Sage; 2004.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Terrin N, Schmid CH, Lau J, Olkin I. Adjusting for publication bias in the presence of heterogeneity. Stat Med. 2003;22(13):2113–26.
Cohen J. Statistical Power Analysis for the Behavioral Sciences. New Jersey: Lawrence Erlbaum Associates Inc; 1988.
Penta FB, Kofman S. The effectiveness of simulation devices in teaching selected skills of physical diagnosis. J Med Educ. 1973;48(5):442–5.
Woolliscroft JO, Calhoun JG, Tenhaken JD, Judge RD. Harvey: the impact of a cardiovascular teaching simulator on student skill acquisition. Med Teach. 1987;9(1):53–7.
Harrell JS, Champagne MT, Jarr S, Miyaya M. Heart sound simulation: how useful for critical care nurses? Heart Lung. 1990;19(2):197–202.
Oddone EZ, Waugh RA, Samsa G, Corey R, Feussner JR. Teaching cardiovascular examination skills: results from a randomized controlled trial. Am J Med. 1993;95(4):389–96.
Takashina T, Shimizu M, Katayama H. A new cardiology patient simulator. Cardiology. 1997;88(5):408–13.
Issenberg S, Gordon DL, Stewart GM, Felner JM. Bedside cardiology skills training for the physician assistant using simulation technology. Perspect Physician Assist Educ. 2000;11(1):99–103.
Issenberg SB, McGaghie WC, Gordon DL, Symes S, Petrusa ER, Hart IR, et al. Effectiveness of a cardiology review course for internal medicine residents using simulation technology and deliberate practice. Teach Learn Med. 2002;14(4):223–8.
Issenberg SB, Gordon MS, Greber AA. Bedside cardiology skills training for the osteopathic internist using simulation technology. J Am Osteopath Assoc. 2003;103(12):603–7.
Fraser K, Peets A, Walker I, Tworek J, Paget M, Wright B, et al. The effect of simulator training on clinical skills acquisition, retention and transfer. Med Educ. 2009;43(8):784–9.
Butter J, McGaghie WC, Cohen ER, Kaye M, Wayne DB. Simulation-based mastery learning improves cardiac auscultation skills in medical students. J Gen Intern Med. 2010;25(8):780–5.
Tiffen J, Corbridge S, Robinson P. Patient simulator for teaching heart and lung assessment skills to advanced practice nursing students. Clin Simul Nurs. 2011;7(3):e91–7.
Kern DH, Mainous AG III, Carey M, Beddingfield A. Simulation-based teaching to improve cardiovascular exam skills performance among third-year medical students. Teach Learn Med. 2011;23(1):15–20.
de Giovanni D, Roberts T, Norman G. Relative effectiveness of high- versus low-fidelity simulation in learning heart sounds. Med Educ. 2009;43(7):661–8.
Ewy GA, Felner JM, Juul D, Mayer JW, Sajid AW, Waugh RA. Test of a cardiology patient simulator with students in fourth-year electives. J Med Educ. 1987;62(9):738–43.
Waugh RA, Mayer JW, Ewy GA, Felner JM, Issenberg BS, Gessner IH, et al. Multimedia computer-assisted instruction in cardiology. Arch Intern Med. 1995;155(2):197–203.
Fraser K, Wright B, Girard L, Tworek J, Paget M, Welikovich L, et al. Simulation training improves diagnostic performance on a real patient with similar clinical findings. Chest. 2011;139(2):376–81.
Champagne MT, Harrell JS, Friedman BJ. Use of a heart sound simulator in teaching cardiac auscultation. Focus Crit Care. 1989;16(6):448–56.
Barrett M, Kuzma M, Seto T, Richards P, Mason D, Barrett D, et al. The power of repetition in mastering cardiac auscultation. Am J Med. 2006;119(1):73–5.
McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. Effect of practice on standardised learning outcomes in simulation-based medical education. Med Educ. 2006;40(8):792–7.
Oxman A, Guyatt G. When to believe a subgroup analysis. In: R H, ed. Users Guides Interactive. Chicago, IL: JAMA Publishing Group; 2002.
Veloski J, Boex JR, Grasberger MJ, Evans A, Wolfson DB. Systematic review of the literature on assessment, feedback and physicians’ clinical performance: BEME Guide No. 7. Med Teach. 2006;28(2):117–28.
Acknowledgements
The authors thank Ryan Brydges, Patricia Erwin, Stanley J. Hamstra, Jason Szostek, Amy Wang, and Ben Zendejas for their assistance with literature searching, abstract reviewing, and data extraction.
Funding/Support
This work was supported by intramural funds, including an award from the Division of General Internal Medicine, Mayo Clinic.
Role of Sponsors
The funding sources for this study played no role in the design and conduct of the study; in the collection, management, analysis, and interpretation of the data; or in the preparation of the manuscript. The funding sources did not review the manuscript.
Conflict of Interest
The authors declare that they do not have a conflict of interest. There was no industry relationship with this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McKinney, J., Cook, D.A., Wood, D. et al. Simulation-Based Training for Cardiac Auscultation Skills: Systematic Review and Meta-Analysis. J GEN INTERN MED 28, 283–291 (2013). https://doi.org/10.1007/s11606-012-2198-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-2198-y