Abstract
BACKGROUND
Inadequate health literacy is prevalent among seniors and is associated with poor health outcomes. At hospital discharge, medications are frequently changed and patients are informed of these changes via their discharge instructions.
OBJECTIVES
Explore the association between health literacy and medication discrepancies 48 hours after hospital discharge and determine the causes of discharge medication discrepancies.
DESIGN
Face-to-face surveys assessing health literacy at hospital discharge using the short form of the Test of Functional Health Literacy in Adults (sTOFHLA). We obtained the medication lists from the written discharge instructions. At 48 hrs post-discharge, we phoned subjects to assess their current medication regimen, any medication discrepancies, and the causes of the discrepancies.
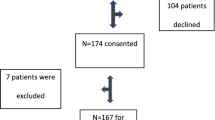
PARTICIPANTS
Two hundred and fifty-four community-dwelling seniors ≥70 years, admitted to acute medicine services for >24 hours at an urban hospital.
RESULTS
Of 254 seniors [mean age 79.3 yrs, 53.1% female], 142 (56%) had a medication discrepancy between their discharge instructions and their actual home medication use 48 hrs after discharge. Subjects with inadequate and marginal health literacy were significantly more likely to have unintentional non-adherence—meaning the subject did not understand how to take the medication [inadequate health literacy 47.7% vs. marginal 31.8% vs. adequate 20.5% p = 0.002]. Conversely, those with adequate health literacy were significantly more likely to have intentional non-adherence—meaning the subject understood the instructions but chose not to follow them as a reason for the medications discrepancy compared with marginal and inadequate health literacy [adequate 73.3% vs. marginal 11.1% vs. inadequate 15.6%, p < 0.001]. Another common cause of discrepancies was inaccurate discharge instructions (39.3%).
CONCLUSION
Seniors with adequate health literacy are more inclined to purposefully not adhere to their discharge instructions. Seniors with inadequate health literacy are more likely to err due to misunderstanding their discharge instructions. Together, these results may explain why previous studies have shown a lack of association between health literacy and overall medication discrepancies.

Similar content being viewed by others
REFERENCES
Unroe KT, Pfeiffenberger T, Riegelhaupt S, Jastrzembski J, Lokhnygina Y, Colón-Emeric C. Inpatient medication reconciliation at admission and discharge: A retrospective cohort study of age and other risk factors for medication discrepancies. Am J Geriatr Pharmacother. 2010;8(2):115–26.
Rogers P. Reconciling Medications at Admission: Safe Practice Recommendations and Implementation Strategies. Joint Comm J Qual Patient Saf. 2006;32(1):37–50.
Calkins DR. Davis RB, Reiley P et al. Patient-Physician Communication at Hospital Discharge and Patients' Understanding of the Postdischarge Treatment Plan. Arch Intern Med. 1997;157:1026–30.
Joint Commission on Accreditation of Healthcare Organizations. Using Medication Reconciliation to Reduce Errors. Oakbrook Terace (IL): Joint Commission on Accreditation of Healthcare Organizations; 2006 [Accessed March 1, 2011] Available from: http://www.jointcommission.org/assets/1/18/SEA_35.PDF
Joint Commission on Accreditation of Healthcare Organizations. 2005 National Safety Goals. Oakbrook Terace (IL): Joint Commission on Accreditation of Healthcare Organizations; 2006 [Accessed March 1, 2011] Available from: http://www.jointcommission.org/npsg_reconciling_medication/
Gray SL, Blough DK. Adverse drug events in elderly patients receiving home health services following hospital discharge. Ann Pharmacother. 1999;33:1147–53.
Gillick MR, Gillick LS. Adverse consequences of hospitalization in the elderly. Soc Sci Med. 1982;16:1033–8.
Forster AJ, Clark HD, Menard A. Adverse events among medical patients after discharge from hospital. Can Med Assoc J. 2004;170:345–9.
Beers MH. DJ, Hasegawa J, Tamai IY. Influence of hospitalization on drug therapy in the elderly. J Am Geriatr Soc. 1989;37:679–83.
Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161–7.
Forster AJ, Clark HD, Menard A. Adverse events among medical patients after discharge from hospital. Can Med Assoc J. 2004;170:345–9.
Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118:219–23.
Coleman ESJ, Raha D, Min S. Posthospital medication discrepancies. Arch Intern Med. 2005;165:1842–7.
DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42:200–9.
Gellad WF, Grenard JL, Marcum ZA. A Systematic Review of Barriers to Medication Adherence in the Elderly: Looking Beyond Cost and Regimen Complexity. Am J Geriatr Pharm. 2011;9(1):11–23.
Ettenhofer ML, Foley J, Castellon SA, Hinkin CH. Reciprocal prediction of medication adherence and neurocognition in HIV/AIDS. Neurology. 2010;74(15):1217–22.
Nielsen-Bohlman L, Panzer A, Kindig DA eds. Health Literacy: A Prescription to End Confusion. Institute of Medicine, 2004. National Academies Press, 500 Fifth St. NW, Washington, DC 20001
Kutner M, Greenberg E, Jin Y, Paulsen C. The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy (NCES 2006–483).U.S. Department of Education.Washington, DC: National Center for Education Statistics
Gazmararian J, Baker D, Williams M, et al. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281(6):545–51.
Baker DW, Gazmararian JA, Williams MV, et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Publ Health. 2002;92(8):1278–83.
Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. J Gen Intern Med. 1998;13(12):791–8.
Paasche-Orlow MK, Cheng DM, Palepu A, Meli S, Faber V, Samet JH. Health literacy, antiretroviral adherence, and HIV-RNA suppression: a longitudinal perspective. J Gen Intern Med. 2006;21:835–40.
Hironaka LK, Paasche-Orlow MK, Young RL, Bauchner H, Geltman PL. Caregiver health literacy and adherence to a daily multi-vitamin with iron regimen in infants. Patient Educ Counsel. 2009;75(3):376–80.
Lindquist LA, Go L, Fleisher J, Jain N, Baker DW. Improvements in cognition following hospital discharge of community dwelling seniors. July: J Gen Intern Med; 2011.
Folstein MF, McHugh PR. Mini Mental State: A practical method for grading the cognitive state of patient for the clinician. J Psych Res. 1975;12:196–8.
Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients' literacy skills. J Gen Intern Med. 1995;10(10):537–41.
Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Counsel. 1999;38(1):33–42.
Coleman EA, Smith JD, Raha D, Min SJ. Post-hospital medication discrepancies: prevalence, types and contributing factors. Arch of Int Med. 2005;165(16):1842–7.
Smith JD, Coleman EA, Min S. Identifying post-acute medication discrepancies in community dwelling older adults: a new tool. Am J Geriatr Pharmacother. 2004;2(2):141–8.
Baker DW, Gazmararian JA, Sudano J, Patterson M, Parker RM, Williams MV. Health literacy and performance on the Mini-Mental State Examination. Aging Ment Health. 2002;6(1):22–9.
Murphy DA, Lam P, Naar-King S, Robert D, Parsons JT, Muenz LR. Health literacy and antiretroviral adherence among HIV-infected adolescents. Patient Educ Counsel. 2010;79(1):25–9.
Lindquist LA, Baker DW. Understanding preventable hospital readmissions: masqueraders, markers, and true causal factors. J Hosp Med. 2011;6(2):51–3.
Acknowledgements
Dr. Lindquist and this study were funded by a grant from the National Institute of Aging (K23AG028439-04). The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. Preliminary data for this paper were presented as an abstract at the Society of General Internal Medicine 2010 National Meeting.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lindquist, L.A., Go, L., Fleisher, J. et al. Relationship of Health Literacy to Intentional and Unintentional Non-Adherence of Hospital Discharge Medications. J GEN INTERN MED 27, 173–178 (2012). https://doi.org/10.1007/s11606-011-1886-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-011-1886-3