Abstract
BACKGROUND
The inaccurate recording of medicines on admission to hospital is an important cause of medication error. Medication reconciliation has been used to identify and correct these errors.
OBJECTIVE
To determine if a multimodal intervention involving medication reconciliation with real-time feedback and education would reduce the number of errors made by medical staff when recording medicines at the time of admission to hospital.
DESIGN
Observational study.
PARTICIPANTS
Patients admitted to the general medical wards of a teaching hospital were studied prospectively. Patients ≥75 years of age and on ≥5 medications were identified as the ‘target group.’
INTERVENTION
After admission, a second medication history was taken, and discrepancies were identified and communicated to the medical teams. An educational intervention to encourage prescribers to obtain accurate medication histories was conducted at the same time.
MEASUREMENTS
The discrepancy rate was measured before and after the intervention.
MAIN RESULTS
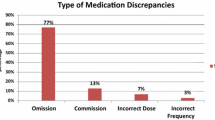
There were 470 admissions in the ‘target group.’ Three hundred and thirty-eight of the admissions (71.9%) had one or more unintentional discrepancies. Although many discrepancies had little potential to cause harm, 33% were rated as clinically significant. During the study the discrepancy rate (prior to reconciliation) fell from 2.6 (SD 2.6) to 1.0 (SD 1.1) per admission (p < 0.0001). This decline in discrepancy rate remained significant (p = 0.001) even when only clinically important discrepancies were included. The proportion of admissions with one or more clinically important discrepancies also decreased during the study from 46% to 24% (p = 0.023).
CONCLUSIONS
Errors in the recording of medicines at the time of hospital admission are common. Combining the feedback provided by medication reconciliation with prescriber education reduced the error rate. This approach may be useful when the resources are not available to perform medication reconciliation for all patients admitted to hospital.




Similar content being viewed by others
References
Cornish PL, Knowles SR, Marchesano R, et al. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med. 2005;165:424–9.
Rozich JD, Resar RK. Medication safety: one organization’s approach to the challenge. J Clin Outcomes Manage. 2001;8:27–34.
Sullivan C, Gleason KM, Rooney D, Groszek JM, Barnard C. Medication reconciliation in the acute care setting: opportunity and challenge for nursing. J Nurs Care Qual. 2005;20:95–8.
Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ. 2005;173:510–5.
Manno MS, Hayes DD. Best-Practice Interventions: How medication reconciliation saves lives. Nursing. 2006;36:63–64.
Institute for Healthcare Improvement. Overview of the 5 Million Lives Campaign. Available at: http://www.ihi.org/IHI/Programs/Campaign/Campaign.htm?TabId=1. Accessed 14 February, 2010.
Thompson, C. A. JCAHO views medication reconciliation as adverse-event prevention. Am J Health Syst Pharm. 2005;62:1528,1530,1532.
Boockvar KS, Carlson LaCorte H, Giambanco V, Fridman B, Siu A. Medication reconciliation for reducing drug-discrepancy adverse events. Am J Geriatr Pharmacother. 2006;4:236–43.
Collins D, Nickless G, Green C. Medication histories: does anyone know what medicines a patient should be taking? Int J Pharm Pract. 2004;12:173–8.
Pronovost P, Weast B, Schwarz M, et al. Medication reconciliation: a practical tool to reduce the risk of medication errors. J Crit Care. 2003;18:201–5.
Slee A, Farrar K, Hughes D, Constable S. Optimising medical treatment—how pharmacist-acquired medication histories have a positive impact on patient care. Pharmaceut J. 2006;277:737–9.
Budnitz DS, Pollock DA, Weidenbach KN, Mendelsohn AB, Schroeder TJ, Annest JL. National surveillance of emergency department visits for outpatient adverse drug events. JAMA. 2006;296:1858–66.
Donohoo, E., Hoa, V., Jarvis, J., Keen, S., Morgan, E, eds. MIMS New ethicals—Issue 4. Auckland: CMPMedica (NZ) Ltd; 2005.
Fisher LD, van Belle G. Biostatistics: A Methodology for the Health Sciences. New York: John Wiley and Sons; 1993.
Fertleman M, Barnett N, Patel T. Improving medication management for patients: the effect of a pharmacist on post-admission ward rounds. Qual Safe Health Care. 2005;14:207–11.
Varkey P, Cunningham J, O’meara J, et al. Multidisciplinary approach to inpatient medication reconciliation in an academic setting. Am J Health Syst Pharm. 2007;64:1–12.
Schnipper JL, Liang CL, Bhan I, Labonville SA, Broverman CA. Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Intern Med. 2009;169:771–80.
Lau HS, Florax C, Porsius AJ, De Boer A. The completeness of medication histories in hospital medical records of patients admitted to general internal medicine wards. Br J Clin Pharmacol. 2000;49:597–603.
Cohen J, Wilson C, Ward F. Improve drug history taking. Pharm Pract. 1998;8:13–6.
Grimshaw JM, Shirran L, Thomas R, et al. Changing provider behavior: an overview of systematic reviews of interventions. Med Care. 2001;39:2–45.
Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients' care. Lancet. 2003;362:1225–30.
Acknowledgements
Amy Chan was supported by a summer studentship from the Maurice and Phyllis Paykel Trust. The project was funded by the Auckland District Health Board. The results of this study were presented at the meeting of the Australasian Society of Clinical and Experimental Pharmacology in Auckland, New Zealand, on 31 August 2007
We would like to dedicate this study to the late Professor Peter Black who originally formulated the idea of this project. We would like to thank all the medical staff, pharmacists and nurses involved in this project. We are particularly grateful to Paul Gelber, Rob Ticehurst, Lynne Byers (Pharmacy); John Henley, David Spriggs, Matt Dawes (General Medicine); Lisa Noonan (Pharmacology) and to Greg Gamble, Department of Medicine, University of Auckland, for assistance with the statistical analysis.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chan, A.H.Y., Garratt, E., Lawrence, B. et al. Effect of Education on the Recording of Medicines on Admission to Hospital. J GEN INTERN MED 25, 537–542 (2010). https://doi.org/10.1007/s11606-010-1317-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-010-1317-x