Abstract
Background
Although tight blood pressure control is crucial in reducing vascular complications of diabetes, primary care providers often fail to appropriately intensify antihypertensive medications.
Objective
To identify novel visit-based factors associated with intensification of antihypertensive medications in adults with diabetes.
Design
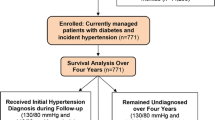
Non-concurrent prospective cohort study.
Patients
A total of 254 patients with type 2 diabetes and hypertension enrolled in an academically affiliated managed care program. Over a 24-month interval (1999–2001), we identified 1,374 visits at which blood pressure was suboptimally controlled (systolic BP ≥ 140 mmHg or diastolic BP ≥ 90 mmHg).
Measurements and Main Results
Intensification of antihypertensive medications at each visit was the primary outcome. Primary care providers intensified antihypertensive treatment in only 176 (13%) of 1,374 visits at which blood pressure was elevated. As expected, higher mean systolic and mean diastolic blood pressures were important predictors of intensification. Treatment was also more likely to be intensified at visits that were “routine” odds ratio (OR) 2.08; 95% Confidence Interval [95% CI] 1.36–3.18), or that paired patients with their usual primary care provider (OR 1.84; 95% CI 1.11–3.06). In contrast, several factors were associated with failure to intensify treatment, including capillary glucose >150 mg/dL (OR 0.54; 95% CI 0.31–0.94) and the presence of coronary heart disease (OR 0.61; 95% CI 0.38–0.95). Co-management by a cardiologist accounted partly for this failure (OR 0.65; 95% CI 0.41–1.03).
Conclusions
Failure to appropriately intensify antihypertensive treatment is common in diabetes care. Clinical distractions and shortcomings in continuity and coordination of care are possible targets for improvement.

Similar content being viewed by others
References
Hypertension in Diabetes Study (HDS). I. Prevalence of hypertension in newly presenting type 2 diabetic patients and the association with risk factors for cardiovascular and diabetic complications. J Hypertens. 1993;11:309–17.
Birkenhager WH, Staessen JA, Gasowski J, de Leeuw PW. Effects of antihypertensive treatment on endpoints in the diabetic patients randomized in the Systolic Hypertension in Europe (Syst-Eur) trial. J Nephrol. 2000;13:232–37.
UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317:703–13.
SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). JAMA. 1991;265:3255–64.
Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000;321:412–9.
Wang JG, Staessen JA, Gong L, Liu L. Chinese trial on isolated systolic hypertension in the elderly. Systolic hypertension in China (Syst-China) Collaborative Group. Arch Intern Med. 2000;160:211–20.
Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;351:1755–62.
Chin MH, Su AW, Jin L, Nerney MP. Variations in the care of elderly persons with diabetes among endocrinologists, general internists, and geriatricians. J Gerontol Ser A Biol Sci Med Sci. 2000;55:M601–M606.
Hicks PC, Westfall JM, Van Vorst RF, et al. Action or inaction? Decision-making in patients with diabetes and elevated blood pressure in primary care. Diabetes Care. 2006;29:2580–5.
Harris MI. Health care and health status and outcomes for patients with type 2 diabetes. Diabetes Care. 2000;23:754–8.
Supina AL, Guirguis LM, Majumdar SR, et al. Treatment gaps for hypertension management in rural Canadian patients with type 2 diabetes mellitus. Clin Ther. 2004;26:598–606.
Godley PJ, Maue SK, Farrelly EW, Frech F. The need for improved medical management of patients with concomitant hypertension and type 2 diabetes mellitus. Am J Manag Care. 2005;11:206–10.
Schaars CF, Denig P, Kasje WN, Stewart RE, Wolffenbuttel BH, Haaijer-Ruskamp FM. Physician, organizational, and patient factors associated with suboptimal blood pressure management in type 2 diabetic patients in primary care. Diabetes Care. 2004;27:123–8.
Toth EL, Majumdar SR, Guirguis LM, Lewanczuk RZ, Lee TK, Johnson JA. Compliance with clinical practice guidelines for type 2 diabetes in rural patients: treatment gaps and opportunities for improvement. Pharmacotherapy. 2003;23:659–65.
Berlowitz DR, Ash AS, Hickey EC, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339:1957–63.
Hyman DJ, Pavlik VN, Vallbona C. Physician role in lack of awareness and control of hypertension. J Clin Hypertens (Greenwich). 2000;2:324–30.
Oliveria SA, Lapuerta P, McCarthy BD, L’Italien GJ, Berlowitz D, Asch SM. Physician-related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162:413–20.
Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure . The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V. Arch Intern Med. 1993;153:154–83.
Steiner JF, Koepsell TD, Fihn SD, Inui TS. A general method of compliance assessment using centralized pharmacy records. Description and validation. Med Care. 1988;26:814–23.
Weiner J, Abrams C, Kaplowitz C. http://www.acg.jhsph.edu/ACGDocuments/newsletter_f2002.pdf. 2002 (accessed on January 9, 2007).
American Medical Association Doctor Finder. http://www.ama-assn.org. 2005 (accessed on March 10, 2005).
Maryland Board of Physicians. http://www.mbp.state.md.us. 2005 (accessed on March 10, 2005).
Cotton A, Aspy CB, Mold J, Stein H. Clinical decision-making in blood pressure management of patients with diabetes mellitus: an Oklahoma Physicians Resource/Research Network (OKPRN) Study. J Am Board Fam Med. 2006;19:232–9.
Berlowitz DR, Ash AS, Hickey EC, Glickman M, Friedman R., Kader B. Hypertension management in patients with diabetes: the need for more aggressive therapy. Diabetes Care. 2003;26:355–9.
Kelly J, Schumacher C, Mayer AM, Brown T. Diabetes care: a comparison of management systems. Alaska Med. 2000;42:13–9, 27.
Walsh MN, Simpson RJ Jr, Wan GJ, Weiss TW, Alexander CM, Markson LE, Berger ML, Pearson TA. Do disease management programs for patients with coronary heart disease make a difference? Experiences of nine practices. Am J Manag Care. 2002;8:937–46.
Acknowledgment
This work was presented at the national Society of General Internal Medicine in April 2006. Dr. Shari Bolen was supported by a T32 NRSA training grant. Dr. T. Alafia Samuels was supported by NIH training grant (HD 08487) and NIH/NHLBI Cardiovascular Epidemiology Training Grant (T32HL07024). Dr. Fred Brancati was supported by a Mid Career Award for Patient-Oriented Research in Diabetes from the NIDDK, Bethesda, MD (1K24-DK6222-01). Funding for this project was received from AHRQ Dissertation Grant (1R03HS011946-01), and from the Johns Hopkins Department of Epidemiology, Summer Epidemiology Program Fund. Funders provided financial resources only, and did not contribute to the project otherwise.
This study was reviewed and approved by the Johns Hopkins School of Public Health Institutional Review Board.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bolen, S.D., Samuels, T.A., Yeh, HC. et al. Failure to Intensify Antihypertensive Treatment by Primary Care Providers: A Cohort Study in Adults with Diabetes Mellitus and Hypertension. J GEN INTERN MED 23, 543–550 (2008). https://doi.org/10.1007/s11606-008-0507-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-008-0507-2