Abstract
Background
Endoscopic retrograde cholangiopancreatography (ERCP) is the first line treatment for choledocholithiasis. In many occasions, several attempts of ERCP are performed until failure is declared and surgical treatment is applied, in many times following procedure-related complications. We present the results of surgical management of patients with choledocholithiasis following repeated failures of ERCP due to impaction of multiple large stones.
Methods
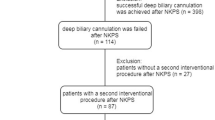
Patients that underwent surgical treatment for choledocholithiasis following repeated ERCP attempts between January 2006 and December 2018 were retrospectively assessed. Post-ERCP complications were evaluated and the surgical approach, technique, and outcomes were assessed.
Results
One hundred and two patients were operated on for choledocholithiasis following repeated failed ERCP. All the patients had at least 2 failed attempts (mean = 3.2 ± 1.7), and 25 (23.5%) suffered major ERCP-related complications. Following choledochotomy and stone extraction, bilioenteric anastomosis was done in the vast majority of patients (90.2%), most commonly choledochoduodenostomy (62%). Thirty-eight (37%) patients had minimally invasive procedure (laparoscopic n = 26, robotic assisted n = 12). Major post-operative complications (Clavien-Dindo ≥ 3) occurred in 24 patients (23.5%). Nine patients (8.8%) were re-operated and 10 (9.8%) were readmitted within 30 days from surgery. Three patients died within 30 days from surgery. Older patients had significantly more ERCP attempts and suffered higher post-operative mortality. During a median follow-up of 70 months, the only biliary complication was an anastomotic stricture in one patient.
Conclusion
Surgery for CBDS after failure of ERCP is safe and provides a highly effective long-term solution.
Similar content being viewed by others
References
Collins C, Maguire D, Ireland A, Fitzgerald E, O'Sullivan GC. A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy: natural history of choledocholithiasis revisited. Ann Surg. Jan 2004;239(1):28-33. https://doi.org/10.1097/01.sla.0000103069.00170.9c.
Hungness ES, Soper NJ. Management of common bile duct stones. J Gastrointest Surg. Apr 2006;10(4):612-619. https://doi.org/10.1016/j.gassur.2005.08.015.
Schacher FC, Giongo SM, Teixeira FJP, Mattos AZ. Endoscopic retrograde cholangiopancreatography versus surgery for choledocholithiasis - A meta-analysis. Ann Hepatol. Jul - Aug 2019;18(4):595-600. https://doi.org/10.1016/j.aohep.2019.01.010.
Ruiz Cuesta P, Hervas Molina AJ, Munoz Garcia-Borruel M, et al. Endoscopic retrograde cholangiopancreatography in patients with anatomic abnormalities of the stomach due to surgery. Gastroenterol Hepatol. Dec 2013;36(10):609-615. https://doi.org/10.1016/j.gastrohep.2013.08.001.
Senthilnathan P, Sharma D, Sabnis SC, et al. Laparoscopic choledochoduodenostomy as a reliable rescue procedure for complicated bile duct stones. Surg Endosc. Apr 2018;32(4):1828-1833. https://doi.org/10.1007/s00464-017-5868-3.
Dumonceau JM, Kapral C, Aabakken L, et al. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. Feb 2020;52(2):127-149. https://doi.org/10.1055/a-1075-4080.
Rustagi T, Jamidar PA. Endoscopic retrograde cholangiopancreatography (ERCP)-related adverse events: post-ERCP pancreatitis. Gastrointest Endosc Clin N Am. Jan 2015;25(1):107-121. https://doi.org/10.1016/j.giec.2014.09.006.
Szary NM, Al-Kawas FH. Complications of endoscopic retrograde cholangiopancreatography: how to avoid and manage them. Gastroenterol Hepatol (N Y). Aug 2013;9(8):496-504.
Rustagi T, Jamidar PA. Endoscopic retrograde cholangiopancreatography-related adverse events: general overview. Gastrointest Endosc Clin N Am. Jan 2015;25(1):97-106. https://doi.org/10.1016/j.giec.2014.09.005.
Weiser R, Pencovich N, Mlynarsky L, et al. Management of endoscopic retrograde cholangiopancreatography-related perforations: Experience of a tertiary center. Surgery. Apr 2017;161(4):920-929. https://doi.org/10.1016/j.surg.2016.10.029.
Prachayakul V, Aswakul P. Endoscopic retrograde cholangiopancreatography-related perforation: Management and prevention. World J Clin Cases. Oct 16 2014;2(10):522-527. https://doi.org/10.12998/wjcc.v2.i10.522.
Lyu Y, Cheng Y, Li T, Cheng B, Jin X. Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis: a meta-analysis. Surg Endosc. Oct 2019;33(10):3275-3286. https://doi.org/10.1007/s00464-018-06613-w.
Martin DJ, Vernon DR, Toouli J. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. Apr 19 2006(2):CD003327. https://doi.org/10.1002/14651858.CD003327.pub2.
Gupta N. Role of laparoscopic common bile duct exploration in the management of choledocholithiasis. World J Gastrointest Surg. May 27 2016;8(5):376-381. https://doi.org/10.4240/wjgs.v8.i5.376.
Zhang J, Ling X. Risk factors and management of primary choledocholithiasis: a systematic review. ANZ J Surg. Aug 19 2020. https://doi.org/10.1111/ans.16211.
Author information
Authors and Affiliations
Contributions
MY — study conception and design, acquisition of data, revising the draft critically for important intellectual content.
NP — drafting of manuscript, analysis, and interpretation of data.
REO — acquisition of data, revising the draft critically for important intellectual content.
NL — acquisition of data, revising the draft critically for important intellectual content.
YG — acquisition of data, revising the draft critically for important intellectual content.
AP — acquisition of data, revising the draft critically for important intellectual content.
IN — study conception and design, critical revision of manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Muhammad Younis and Niv Pencovich contributed equally to this work.
Rights and permissions
About this article
Cite this article
Younis, M., Pencovich, N., El-On, R. et al. Surgical Treatment for Choledocholithiasis Following Repeated Failed Endoscopic Retrograde Cholangiopancreatography. J Gastrointest Surg 26, 1233–1240 (2022). https://doi.org/10.1007/s11605-022-05309-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-022-05309-w