Abstract
Background
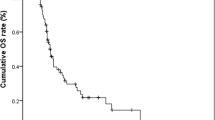
The effects of primary tumor location on colorectal liver metastasis (CRLM) and post-hepatic-metastasectomy overall survival (OS) are controversial. This study evaluated the difference in post-hepatic-metastasectomy OS among right-sided colon, left-sided colon, and rectal cancer groups.
Methods
In total, 381 patients who underwent curative-intent CRLM resection were enrolled. Patients were grouped based on the primary tumor location (right-sided, left-sided, and rectum). The Kaplan–Meier analysis and log-rank test were performed for survival analysis. The univariate and multivariate analyses of clinical and pathological factors were performed using the Cox proportional hazards model.
Results
Significant OS difference was noted among the three groups (log-rank, p = 0.014). The multivariate analysis revealed a 32% lower death risk in left-sided colon cancer compared with right-sided colon cancer (hazard ratio [HR] 0.68, p = 0.042), whereas no OS difference was noted between the rectal cancer and right-sided colon cancer groups. The left- versus right-sided OS advantage was noted only in the KRAS wild-type subgroup (HR 0.46, p = 0.002), and a rectal versus right-sided OS disadvantage was noted in the KRAS mutant subgroup (HR 1.78, p = 0.03).
Conclusions
The CRLM post-hepatic-metastasectomy OS was superior in left-sided colon cancer than in right-sided colon cancer and was similar in rectal and right-sided colon cancer. The OS difference in different primary tumor locations is dependent on KRAS mutation status, with a decreased left- versus right-sided death risk noted only in KRAS wild-type colon cancer and an increased rectal versus right-sided death risk noted only in KRAS mutant colon cancer.





Similar content being viewed by others
References
Bufill JA. Colorectal cancer: evidence for distinct genetic categories based on proximal or distal tumor location. Ann Intern Med. 1990;113(10):779-88. https://doi.org/10.7326/0003-4819-113-10-779.
Gervaz P, Bucher P, Morel P. Two colons-two cancers: paradigm shift and clinical implications. J Surg Oncol. 2004;88(4):261-6. https://doi.org/10.1002/jso.20156.
Dujovny N, Quiros RM, Saclarides TJ. Anorectal anatomy and embryology. Surg Oncol Clin N Am. 2004;13(2):277-93. https://doi.org/10.1016/j.soc.2004.01.002.
Salem ME, Weinberg BA, Xiu J, El-Deiry WS, Hwang JJ, Gatalica Z et al. Comparative molecular analyses of left-sided colon, right-sided colon, and rectal cancers. Oncotarget. 2017;8(49):86356-68. https://doi.org/10.18632/oncotarget.21169.
Petrelli F, Tomasello G, Borgonovo K, Ghidini M, Turati L, Dallera P et al. Prognostic Survival Associated With Left-Sided vs Right-Sided Colon Cancer: A Systematic Review and Meta-analysis. JAMA Oncol. 2017;3(2):211-9. https://doi.org/10.1001/jamaoncol.2016.4227.
Yahagi M, Okabayashi K, Hasegawa H, Tsuruta M, Kitagawa Y. The Worse Prognosis of Right-Sided Compared with Left-Sided Colon Cancers: a Systematic Review and Meta-analysis. J Gastrointest Surg. 2016;20(3):648-55. https://doi.org/10.1007/s11605-015-3026-6.
Arnold D, Lueza B, Douillard JY, Peeters M, Lenz HJ, Venook A et al. Prognostic and predictive value of primary tumour side in patients with RAS wild-type metastatic colorectal cancer treated with chemotherapy and EGFR directed antibodies in six randomized trials. Ann Oncol. 2017;28(8):1713-29. https://doi.org/10.1093/annonc/mdx175.
Meguid RA, Slidell MB, Wolfgang CL, Chang DC, Ahuja N. Is there a difference in survival between right- versus left-sided colon cancers? Ann Surg Oncol. 2008;15(9):2388-94. https://doi.org/10.1245/s10434-008-0015-y.
Price TJ, Beeke C, Ullah S, Padbury R, Maddern G, Roder D et al. Does the primary site of colorectal cancer impact outcomes for patients with metastatic disease? Cancer. 2015;121(6):830-5. https://doi.org/10.1002/cncr.29129.
Lu HJ, Lin JK, Chen WS, Jiang JK, Yang SH, Lan YT et al. Primary tumor location is an important predictive factor for wild-type KRAS metastatic colon cancer treated with cetuximab as front-line bio-therapy. Asia Pac J Clin Oncol. 2016;12(3):207-15. https://doi.org/10.1111/ajco.12469.
Chen KH, Shao YY, Chen HM, Lin YL, Lin ZZ, Lai MS et al. Primary tumor site is a useful predictor of cetuximab efficacy in the third-line or salvage treatment of KRAS wild-type (exon 2 non-mutant) metastatic colorectal cancer: a nationwide cohort study. BMC Cancer. 2016;16:327. https://doi.org/10.1186/s12885-016-2358-2.
Moretto R, Cremolini C, Rossini D, Pietrantonio F, Battaglin F, Mennitto A et al. Location of Primary Tumor and Benefit From Anti-Epidermal Growth Factor Receptor Monoclonal Antibodies in Patients With RAS and BRAF Wild-Type Metastatic Colorectal Cancer. Oncologist. 2016;21(8):988-94. https://doi.org/10.1634/theoncologist.2016-0084.
Venook AP, Niedzwiecki D, Innocenti F, Fruth B, Greene C, O’Neil BH et al. Impact of primary (1º) tumor location on overall survival (OS) and progression-free survival (PFS) in patients (pts) with metastatic colorectal cancer (mCRC): Analysis of CALGB/SWOG 80405 (Alliance). Journal of Clinical Oncology. 2016;34(15_suppl):3504-. https://doi.org/10.1200/JCO.2016.34.15_suppl.3504.
Schwartzberg LS, Rivera F, Karthaus M, Fasola G, Canon JL, Hecht JR et al. PEAK: a randomized, multicenter phase II study of panitumumab plus modified fluorouracil, leucovorin, and oxaliplatin (mFOLFOX6) or bevacizumab plus mFOLFOX6 in patients with previously untreated, unresectable, wild-type KRAS exon 2 metastatic colorectal cancer. J Clin Oncol. 2014;32(21):2240-7. https://doi.org/10.1200/JCO.2013.53.2473.
Rivera F, Karthaus M, Hecht JR, Sevilla I, Forget F, Fasola G et al. Final analysis of the randomised PEAK trial: overall survival and tumour responses during first-line treatment with mFOLFOX6 plus either panitumumab or bevacizumab in patients with metastatic colorectal carcinoma. Int J Colorectal Dis. 2017;32(8):1179-90. https://doi.org/10.1007/s00384-017-2800-1.
Douillard JY, Siena S, Cassidy J, Tabernero J, Burkes R, Barugel M et al. Randomized, phase III trial of panitumumab with infusional fluorouracil, leucovorin, and oxaliplatin (FOLFOX4) versus FOLFOX4 alone as first-line treatment in patients with previously untreated metastatic colorectal cancer: the PRIME study. J Clin Oncol. 2010;28(31):4697-705. https://doi.org/10.1200/JCO.2009.27.4860.
Douillard JY, Siena S, Cassidy J, Tabernero J, Burkes R, Barugel M et al. Final results from PRIME: randomized phase III study of panitumumab with FOLFOX4 for first-line treatment of metastatic colorectal cancer. Ann Oncol. 2014;25(7):1346-55. https://doi.org/10.1093/annonc/mdu141.
Van Cutsem E, Nordlinger B, Adam R, Kohne CH, Pozzo C, Poston G et al. Towards a pan-European consensus on the treatment of patients with colorectal liver metastases. Eur J Cancer. 2006;42(14):2212-21. https://doi.org/10.1016/j.ejca.2006.04.012.
Stangl R, Altendorf-Hofmann A, Charnley RM, Scheele J. Factors influencing the natural history of colorectal liver metastases. The Lancet. 1994;343(8910):1405-10. https://doi.org/10.1016/s0140-6736(94)92529-1.
Choti MA, Sitzmann JV, Tiburi MF, Sumetchotimetha W, Rangsin R, Schulick RD et al. Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg. 2002;235(6):759-66. https://doi.org/10.1097/00000658-200206000-00002.
Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg. 2005;241(5):715–22, discussion 22–4. https://doi.org/10.1097/01.sla.0000160703.75808.7d.
Kanas GP, Taylor A, Primrose JN, Langeberg WJ, Kelsh MA, Mowat FS et al. Survival after liver resection in metastatic colorectal cancer: review and meta-analysis of prognostic factors. Clin Epidemiol. 2012;4:283-301. https://doi.org/10.2147/CLEP.S34285.
Aloia TA, Vauthey JN, Loyer EM, Ribero D, Pawlik TM, Wei SH et al. Solitary colorectal liver metastasis: resection determines outcome. Arch Surg. 2006;141(5):460–6; discussion 6–7. https://doi.org/10.1001/archsurg.141.5.460.
Marques MC, HS CR, Costa WL, Jr., de Jesus VHF, de Macedo MP, Diniz AL et al. Is primary sidedness a prognostic factor in patients with resected colon cancer liver metastases (CLM)? J Surg Oncol. 2018;117(5):858–63. https://doi.org/10.1002/jso.25048.
Wang K, Xu D, Yan XL, Poston G, Xing BC. The impact of primary tumour location in patients undergoing hepatic resection for colorectal liver metastasis. Eur J Surg Oncol. 2018;44(6):771-7. https://doi.org/10.1016/j.ejso.2018.02.210.
Makowiec F, Menzel M, Bronsert P, Holzner PA, Klock A, Lang SA et al. Does the site of primary colorectal cancer influence the outcome after resection of isolated liver metastases? Dig Liver Dis. 2018;50(10):1088-92. https://doi.org/10.1016/j.dld.2018.06.019.
Creasy JM, Sadot E, Koerkamp BG, Chou JF, Gonen M, Kemeny NE et al. The Impact of Primary Tumor Location on Long-Term Survival in Patients Undergoing Hepatic Resection for Metastatic Colon Cancer. Ann Surg Oncol. 2018;25(2):431-8. https://doi.org/10.1245/s10434-017-6264-x.
Sasaki K, Andreatos N, Margonis GA, He J, Weiss M, Johnston F et al. The prognostic implications of primary colorectal tumor location on recurrence and overall survival in patients undergoing resection for colorectal liver metastasis. J Surg Oncol. 2016;114(7):803-9. https://doi.org/10.1002/jso.24425.
Yamashita S, Brudvik KW, Kopetz SE, Maru D, Clarke CN, Passot G et al. Embryonic Origin of Primary Colon Cancer Predicts Pathologic Response and Survival in Patients Undergoing Resection for Colon Cancer Liver Metastases. Ann Surg. 2018;267(3):514-20. https://doi.org/10.1097/SLA.0000000000002087.
Loree JM, Pereira AAL, Lam M, Willauer AN, Raghav K, Dasari A et al. Classifying Colorectal Cancer by Tumor Location Rather than Sidedness Highlights a Continuum in Mutation Profiles and Consensus Molecular Subtypes. Clin Cancer Res. 2018;24(5):1062-72. https://doi.org/10.1158/1078-0432.CCR-17-2484.
Brule SY, Jonker DJ, Karapetis CS, O'Callaghan CJ, Moore MJ, Wong R et al. Location of colon cancer (right-sided versus left-sided) as a prognostic factor and a predictor of benefit from cetuximab in NCIC CO.17. Eur J Cancer. 2015;51(11):1405–14. https://doi.org/10.1016/j.ejca.2015.03.015.
Yoon HH, Tougeron D, Shi Q, Alberts SR, Mahoney MR, Nelson GD et al. KRAS codon 12 and 13 mutations in relation to disease-free survival in BRAF-wild-type stage III colon cancers from an adjuvant chemotherapy trial (N0147 alliance). Clin Cancer Res. 2014;20(11):3033-43. https://doi.org/10.1158/1078-0432.CCR-13-3140.
Salem ME, Yin J, Renfro LA, Weinberg BA, Maughan T, Adams R et al. Rectal versus left-sided colon cancers: Clinicopathological differences observed in a pooled analysis of 4,182 patients enrolled to 8 clinical trials from the ARCAD database. Journal of Clinical Oncology. 2017;35(4_suppl):675-. https://doi.org/10.1200/JCO.2017.35.4_suppl.675.
Minsky BD. Unique considerations in the patient with rectal cancer. Semin Oncol. 2011;38(4):542-51. https://doi.org/10.1053/j.seminoncol.2011.05.008.
Chlebowski RT, Wactawski-Wende J, Ritenbaugh C, Hubbell FA, Ascensao J, Rodabough RJ et al. Estrogen plus progestin and colorectal cancer in postmenopausal women. N Engl J Med. 2004;350(10):991-1004. https://doi.org/10.1056/NEJMoa032071.
Hendifar A, Yang D, Lenz F, Lurje G, Pohl A, Lenz C et al. Gender disparities in metastatic colorectal cancer survival. Clin Cancer Res. 2009;15(20):6391-7. https://doi.org/10.1158/1078-0432.CCR-09-0877.
Funding
We give thanks for grants from the Taiwan Clinical Oncology Research Foundation and to the Taipei Veterans General Hospital Big Data Center.
Author information
Authors and Affiliations
Contributions
THC: Data analysis and manuscript writing. WSC, JKJ, SHY, HSW, SCC, YTL, CCL, HHL, SCH, HHC, GYC, CYH, HJL, SCC, and YC: Data collection or management. HWT: Project development, data analysis, and manuscript editing.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, TH., Chen, WS., Jiang, JK. et al. Effect of Primary Tumor Location on Postmetastasectomy Survival in Patients with Colorectal Cancer Liver Metastasis. J Gastrointest Surg 25, 650–661 (2021). https://doi.org/10.1007/s11605-020-04855-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04855-5