Abstract
Introduction
A person’s community, or lived environment, may play an important role in achieving optimal health outcomes. The objective of the current study was to assess the association of county-level vulnerability with the probability of having a non-elective colon resection. We hypothesized that individuals from areas with a high social vulnerability would be at greater risk of non-elective colon resection compared with patients from low social vulnerability areas.
Methods
Patients aged 65–99 who underwent a colon resection for a primary diagnosis of either diverticulitis (n = 11,812) or colon cancer (n = 33,312) were identified in Medicare Part A and Part B for years 2016–2017. Logistic regression analysis was used to evaluate differences in probability of undergoing an elective versus non-elective operation from counties relative to county-level social vulnerability index (SVI). Secondary outcomes included postoperative complications, mortality, readmission, and index hospitalization expenditure.
Results
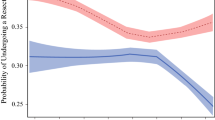
Among 45,124 patients, 11,812 (26.2%) underwent a colon resection for diverticulitis, while 33,312 (73.8%) had a resection for colon cancer; 31,012 (68.7%) patients had an elective procedure (diverticulitis n = 7291 (61.7%) vs. cancer n = 23,721 (71.2%)), while 14,112 (31.3%) had an emergent operation (diverticulitis n = 4521 (38.3%) vs. cancer n = 9591 (28.8%)). Patients with a high SVI were more likely to undergo an emergent colon operation compared with low SVI patients (43.7% vs. 40.4%) (p < 0.001). The association of high SVI with increased risk of an emergent colon operation was similar among patients with diverticulitis (emergent: low SVI 37.2% vs. high SVI 40.4%) or colon cancer (emergent: low SVI 26.0% vs. high SVI 29.9%) (both p < 0.05). On multivariable analyses, risk-adjusted probability of undergoing an urgent/emergent operation remained associated with SVI (p < 0.05).
Conclusion
Patients residing in vulnerable communities characterized by a high SVI were more likely to undergo a non-elective colon resection for either diverticulitis or colon cancer. Patients from high SVI areas had a higher risk of postoperative complications, as well as index hospitalization expenditures; however, there were no differences in mortality or readmission rates.

Similar content being viewed by others
References
Levy H, Janke A. Health literacy and access to care. J Health Commun. 2016;21 Suppl 1:43-50. doi:https://doi.org/10.1080/10810730.2015.1131776
Schoen C, Osborn R, Squires D, Doty MM. Access, affordability, and insurance complexity are often worse in the United States compared to ten other countries. Health Aff Proj Hope. 2013;32(12):2205-2215. doi:https://doi.org/10.1377/hlthaff.2013.0879
Collins SR, Gunja MZ, Doty MM, Beutel S. Americans’ Experiences with ACA Marketplace and Medicaid Coverage: Access to Care and Satisfaction. Published May 25, 2016. Accessed April 20, 2017. http://www.commonwealthfund.org/publications/issue-briefs/2016/may/aca-tracking-survey-access-to-care-and-satisfaction.
Diaz A, Schoenbrunner A, Pawlik TM. Trends in the Geospatial Distribution of Inpatient Adult Surgical Services across the United States: Ann Surg. Published online May 2019:1. https://doi.org/10.1097/SLA.0000000000003366
Kind AJH, Buckingham WR. Making Neighborhood-Disadvantage Metrics Accessible — The Neighborhood Atlas. N Engl J Med. 2018;378(26):2456-2458. doi:https://doi.org/10.1056/NEJMp1802313
Kolak M, Bhatt J, Park YH, Padrón NA, Molefe A. Quantification of Neighborhood-Level Social Determinants of Health in the Continental United States. JAMA Netw Open. 2020;3(1):e1919928. doi:https://doi.org/10.1001/jamanetworkopen.2019.19928
Arcaya M, Tucker-Seeley R, Kim R, Schnake-Mahl A, So M, Subramanian S. Research on Neighborhood Effects on Health in the United States: A Systematic Review of Study Characteristics. Soc Sci Med 1982. 2016;168:16 29. doi:https://doi.org/10.1016/j.socscimed.2016.08.047
Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep Wash DC 1974. 2001;116(5):404-416. doi:https://doi.org/10.1093/phr/116.5.404
Chetty R, Hendren N, Katz LF. The Effects of Exposure to Better Neighborhoods on Children: New Evidence from the Moving to Opportunity Experiment. Am Econ Rev. 2016;106(4):855-902. doi:https://doi.org/10.1257/aer.20150572
Sharkey P. Neighborhoods, Cities, and Economic Mobility. RSF Russell Sage Found J Soc Sci. 2016;2(2):159-177. doi:https://doi.org/10.7758/RSF.2016.2.2.07
McGinnis JM. Income, Life Expectancy, and Community Health: Underscoring the Opportunity. JAMA. 2016;315(16):1709-1710. doi:https://doi.org/10.1001/jama.2016.4729
Branas CC, MacKenzie EJ, Williams JC, et al. Access to Trauma Centers in the United States. JAMA. 2005;293(21):2626-2633. doi:https://doi.org/10.1001/jama.293.21.2626
Jarman MP, Curriero FC, Haut ER, Porter KP, Castillo RC. Associations of Distance to Trauma Care, Community Income, and Neighborhood Median Age With Rates of Injury Mortality. JAMA Surg. 2018;153(6):535-543. doi:https://doi.org/10.1001/jamasurg.2017.6133
Anaya DA, Flum DR. Risk of Emergency Colectomy and Colostomy in Patients With Diverticular Disease. Arch Surg. 2005;140(7):681-685. doi:https://doi.org/10.1001/archsurg.140.7.681
Aslar AK, Özdemir S, Mahmoudi H, Kuzu MA. Analysis of 230 Cases of Emergent Surgery for Obstructing Colon Cancer—Lessons Learned. J Gastrointest Surg. 2011;15(1):110-119. doi:https://doi.org/10.1007/s11605-010-1360-2
Sjo OH, Larsen S, Lunde OC, Nesbakken A. Short term outcome after emergency and elective surgery for colon cancer. Colorectal Dis. 2009;11(7):733-739. doi:https://doi.org/10.1111/j.1463-1318.2008.01613.x
CDC’s Social Vulnerability Index. Published September 5, 2018. Accessed March 14, 2020. https://svi.cdc.gov/
Osborne NH, Nicholas LH, Ryan AM, Thumma JR, Dimick JB. Association of hospital participation in a quality reporting program with surgical outcomes and expenditures for Medicare beneficiaries. JAMA. 2015;313(5):496-504. doi:https://doi.org/10.1001/jama.2015.25
Iezzoni LI, Daley J, Heeren T, et al. Identifying complications of care using administrative data. Med Care. 1994;32(7):700-715. doi:https://doi.org/10.1097/00005650-199407000-00004
Paredes AZ, Hyer JM, Beal EW, et al. Impact of skilled nursing facility quality on postoperative outcomes after pancreatic surgery. Surgery. 2019;166(1):1-7. doi:https://doi.org/10.1016/j.surg.2018.12.008
Khubchandani JA, Shen C, Ayturk D, Kiefe CI, Santry HP. Disparities in access to emergency general surgery care in the United States. Surgery. 2018;163(2):243-250. doi:https://doi.org/10.1016/j.surg.2017.07.026
Zogg CK, Scott JW, Jiang W, Wolf LL, Haider AH. Differential access to care: The role of age, insurance, and income on race/ethnicity-related disparities in adult perforated appendix admission rates. Surgery. 2016;160(5):1145-1154. doi:https://doi.org/10.1016/j.surg.2016.06.002
Bennett KM, Scarborough JE, Pappas TN, Kepler TB. Patient socioeconomic status is an independent predictor of operative mortality. Ann Surg. 2010;252(3):552-557; discussion 557-558. doi:https://doi.org/10.1097/SLA.0b013e3181f2ac64
Mehaffey JH, Hawkins RB, Charles EJ, et al. Socioeconomic “Distressed Communities Index” Improves Surgical Risk-adjustment: Ann Surg. 2020;271(3):470-474. doi:https://doi.org/10.1097/SLA.0000000000002997
Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. Am J Prev Med. 2009;36(1):74-81. doi:https://doi.org/10.1016/j.amepre.2008.09.025
Walker RE, Keane CR, Burke JG. Disparities and access to healthy food in the United States: A review of food deserts literature. Health Place. 2010;16(5):876-884. doi:https://doi.org/10.1016/j.healthplace.2010.04.013
Meyer OL, Castro-Schilo L, Aguilar-Gaxiola S. Determinants of mental health and self-rated health: a model of socioeconomic status, neighborhood safety, and physical activity. Am J Public Health. 2014;104(9):1734-1741. doi:https://doi.org/10.2105/AJPH.2014.302003
Williams DR, Costa MV, Odunlami AO, Mohammed SA. Moving Upstream: How Interventions that Address the Social Determinants of Health can Improve Health and Reduce Disparities. J Public Health Manag Pract JPHMP. 2008;14(Suppl):S8-17. doi:https://doi.org/10.1097/01.PHH.0000338382.36695.42
Thornton RLJ, Glover CM, Cené CW, Glik DC, Henderson JA, Williams DR. Evaluating Strategies For Reducing Health Disparities By Addressing The Social Determinants Of Health. Health Aff Proj Hope. 2016;35(8):1416-1423. doi:https://doi.org/10.1377/hlthaff.2015.1357
An R, Xiang X. Social Vulnerability and Obesity among U.S. Adults. Int J Health Sci IJHS. 2015;3(3). doi:https://doi.org/10.15640/ijhs.v3n3a2
Yee CW, Cunningham SD, Ickovics JR. Application of the Social Vulnerability Index for Identifying Teen Pregnancy Intervention Need in the United States. Matern Child Health J. 2019;23(11):1516-1524. doi:https://doi.org/10.1007/s10995-019-02792-7
Carmichael H, Moore A, Steward L, Velopulos CG. Using the Social Vulnerability Index to Examine Local Disparities in Emergent and Elective Cholecystectomy. J Surg Res. 2019;243:160-164. doi:https://doi.org/10.1016/j.jss.2019.05.022
Wilson K d’Almeida, Dray-Spira R, Aubrière C, et al. Frequency and correlates of late presentation for HIV infection in France: older adults are a risk group - results from the ANRS-VESPA2 Study, France. AIDS Care. 2014;26 Suppl 1:S83-93. doi:https://doi.org/10.1080/09540121.2014.906554
Fraser S, Bunce C, Wormald R, Brunner E. Deprivation and late presentation of glaucoma: case-control study. BMJ. 2001;322(7287):639-643. doi:https://doi.org/10.1136/bmj.322.7287.639
Kurani SS, McCoy RG, Lampman MA, et al. Association of Neighborhood Measures of Social Determinants of Health With Breast, Cervical, and Colorectal Cancer Screening Rates in the US Midwest. JAMA Netw Open. 2020;3(3):e200618. doi:https://doi.org/10.1001/jamanetworkopen.2020.0618
Regenbogen SE, Hardiman KM, Hendren S, Morris AM. Surgery for Diverticulitis in the 21st Century: A Systematic Review. JAMA Surg. 2014;149(3):292-303. doi:https://doi.org/10.1001/jamasurg.2013.5477
Koperna T, Kisser M, Schulz F. Emergency Surgery for Colon Cancer in the Aged. Arch Surg. 1997;132(9):1032-1037. doi:https://doi.org/10.1001/archsurg.1997.01430330098018
Scott JW, Olufajo OA, Brat GA, et al. Use of National Burden to Define Operative Emergency General Surgery. JAMA Surg. 2016;151(6):e160480. doi:https://doi.org/10.1001/jamasurg.2016.0480
Lavanchy JL, Vaisnora L, Haltmeier T, et al. Oncologic long-term outcomes of emergency versus elective resection for colorectal cancer. Int J Colorectal Dis. 2019;34(12):2091-2099. doi:https://doi.org/10.1007/s00384-019-03426-8
Soyalp C, Yuzkat N, Kilic M, Akyol ME, Demir CY, Gulhas N. Operative and prognostic parameters associated with elective versus emergency surgery in a retrospective cohort of elderly patients. Aging Clin Exp Res. 2019;31(3):403-410. doi:https://doi.org/10.1007/s40520-018-0976-z
Dimick JB, Chen SL, Taheri PA, Henderson WG, Khuri SF, Campbell DA. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg. 2004;199(4):531-537. doi:https://doi.org/10.1016/j.jamcollsurg.2004.05.276
Healy MA, Mullard AJ, Campbell DA, Dimick JB. Hospital and Payer Costs Associated With Surgical Complications. JAMA Surg. 2016;151(9):823-830. doi:https://doi.org/10.1001/jamasurg.2016.0773
Thomas-Henkel C, Schulman M. Screening for Social Determinants of Health in Populations with Complex Needs: Implementation Considerations. Center for Health Care Stradegies Inc.; 2017:10. http://www.chcs.org/media/SDOH-Complex-Care-Screening-Brief-102617.pdf
Funding
Dr. Diaz receives funding from the University of Michigan Institute for Healthcare Policy and Innovation Clinician Scholars Program and salary support from the Veterans Affairs Office of Academic Affiliations during the time of this study
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
This does not necessarily represent the views of the United States Government or Department of Veterans Affairs.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Diaz, A., Barmash, E., Azap, R. et al. Association of County-Level Social Vulnerability with Elective Versus Non-elective Colorectal Surgery. J Gastrointest Surg 25, 786–794 (2021). https://doi.org/10.1007/s11605-020-04768-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04768-3