Abstract
Background
Securing the surgical margin is the most essential and important task in curative surgery. However, it is difficult to accurately identify the tumor location during laparoscopic surgery for gastric cancer, and existing methods, such as preoperative endoscopic marking with tattooing and clipping, have multiple disadvantages.
Aims
We investigated the feasibility and safety of indocyanine green (ICG) fluorescence marking for determining the tumor location during laparoscopic gastrectomy.
Methods
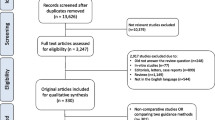
We retrospectively analyzed preoperative and perioperative data from consecutive patients with gastric cancer undergoing planned laparoscopic distal gastrectomy. Data was maintained in a prospectively compiled surgical database, and patients were categorized into ICG (n = 84) or non-ICG (n = 174) groups based on whether they underwent preoperative endoscopic mucosal ICG injection. One-to-one propensity score matching (PSM) was performed to compare outcomes between the two groups.
Results
We included 84 patient pairs after PSM, and there were no significant differences in preoperative patient characteristics. The ICG group had shorter procedure time (p < 0.001), lower estimated blood loss (p = 0.005), and significantly shorter postoperative hospital stay (p < 0.001). Positive resection margins were confirmed in five cases (6.0%) in the non-ICG group, whereas there were none in the ICG group (p = 0.008). Real-time confirmation was possible during laparoscopy, and the injected ICG did not affect the surgical procedure or result in adverse events.
Conclusion
ICG fluorescence imaging is feasible and safe and can potentially be used as a tumor-marking agent for determining the surgical resection line.



Similar content being viewed by others
References
Hachisu T, Miyazaki S, Hamaguchi K. Endoscopic clip-marking of lesions using the newly developed HX-3L clip. Surg Endosc. 1989;3(3):142–7.
Kojima F, Sato T, Tsunoda S, Takahata H, Hamaji M, Komatsu T et al. Development of a novel marking system for laparoscopic gastrectomy using endoclips with radio frequency identification tags: feasibility study in a canine model. Surg Endosc. 2014;28(9):2752–9. https://doi.org/10.1007/s00464-014-3501-2.
Ohdaira T, Nagai H, Shibusawa H. Intraoperative localization of early-stage gastrointestinal tumors using a marking clip detector system. Surgical Technology International. 2005;14:79–83.
Matsuda T, Iwasaki T, Hirata K, Tsugawa D, Sugita Y, Ishida S et al. Simple and reliable method for tumor localization during totally laparoscopic gastrectomy: intraoperative laparoscopic ultrasonography combined with tattooing. Gastric Cancer. 2017;20(3):548–52. https://doi.org/10.1007/s10120-016-0635-z.
Qi XD. [Gastroscopic mucosal biopsy and carbon ink injection marking for determination of resection line on the gastric wall in stomach cancer]. Zhonghua zhong liu za zhi [Chinese Journal of Oncology]. 1989;11(2):136–8.
Tokuhara T, Nakata E, Tenjo T, Kawai I, Satoi S, Inoue K et al. A novel option for preoperative endoscopic marking with India ink in totally laparoscopic distal gastrectomy for gastric cancer: a useful technique considering the morphological characteristics of the stomach. Molecular and clinical oncology. 2017;6(4):483–6. https://doi.org/10.3892/mco.2017.1191.
Kawakatsu S, Ohashi M, Hiki N, Nunobe S, Nagino M, Sano T. Use of endoscopy to determine the resection margin during laparoscopic gastrectomy for cancer. Br J Surg. 2017;104(13):1829–36. https://doi.org/10.1002/bjs.10618.
Park SI, Genta RS, Romeo DP, Weesner RE. Colonic abscess and focal peritonitis secondary to india ink tattooing of the colon. Gastrointestinal endoscopy. 1991;37(1):68–71.
Singh S, Arif A, Fox C, Basnyat P. Complication after pre-operative India ink tattooing in a colonic lesion. Digestive Surgery. 2006;23(5–6):303. https://doi.org/10.1159/000096245.
Chung JW, Seo KW, Jung K, Park MI, Kim SE, Park SJ et al. A promising method for tumor localization during total laparoscopic distal gastrectomy: preoperative endoscopic clipping based on negative biopsy and selective intraoperative radiography findings. Journal of Gastric Cancer. 2017;17(3):220–7. https://doi.org/10.5230/jgc.2017.17.e25.
Daskalaki D, Fernandes E, Wang X, Bianco FM, Elli EF, Ayloo S et al. Indocyanine green (ICG) fluorescent cholangiography during robotic cholecystectomy: results of 184 consecutive cases in a single institution. Surgical Innovation. 2014;21(6):615–21. https://doi.org/10.1177/1553350614524839.
Spinoglio G, Priora F, Bianchi PP, Lucido FS, Licciardello A, Maglione V et al. Real-time near-infrared (NIR) fluorescent cholangiography in single-site robotic cholecystectomy (SSRC): a single-institutional prospective study. Surg Endosc. 2013;27(6):2156–62. https://doi.org/10.1007/s00464-012-2733-2.
Luo S, Zhang E, Su Y, Cheng T, Shi C. A review of NIR dyes in cancer targeting and imaging. Biomaterials. 2011;32(29):7127–38. https://doi.org/10.1016/j.biomaterials.2011.06.024.
Namikawa T, Sato T, Hanazaki K. Recent advances in near-infrared fluorescence-guided imaging surgery using indocyanine green. Surg Today. 2015;45(12):1467–74. https://doi.org/10.1007/s00595-015-1158-7.
Alander JT, Kaartinen I, Laakso A, Patila T, Spillmann T, Tuchin VV et al. A review of indocyanine green fluorescent imaging in surgery. International Journal of Biomedical Imaging. 2012;2012:940585. https://doi.org/10.1155/2012/940585.
Goto O, Takeuchi H, Kawakubo H, Matsuda S, Kato F, Sasaki M et al. Feasibility of non-exposed endoscopic wall-inversion surgery with sentinel node basin dissection as a new surgical method for early gastric cancer: a porcine survival study. Gastric Cancer. 2015;18(2):440–5. https://doi.org/10.1007/s10120-014-0358-y.
Kim M, Son SY, Cui LH, Shin HJ, Hur H, Han SU. Real-time Vessel Navigation Using Indocyanine Green Fluorescence during Robotic or Laparoscopic Gastrectomy for Gastric Cancer. Journal of Gastric Cancer. 2017;17(2):145–53. https://doi.org/10.5230/jgc.2017.17.e17.
Tajima Y, Murakami M, Yamazaki K, Masuda Y, Kato M, Sato A et al. Sentinel node mapping guided by indocyanine green fluorescence imaging during laparoscopic surgery in gastric cancer. Ann Surg Oncol. 2010;17(7):1787–93. https://doi.org/10.1245/s10434-010-0944-0.
Takahashi N, Nimura H, Fujita T, Mitsumori N, Shiraishi N, Kitano S et al. Laparoscopic sentinel node navigation surgery for early gastric cancer: a prospective multicenter trial. Langenbecks Arch Surg. 2017;402(1):27–32. https://doi.org/10.1007/s00423-016-1540-y.
Yano K, Nimura H, Mitsumori N, Takahashi N, Kashiwagi H, Yanaga K. The efficiency of micrometastasis by sentinel node navigation surgery using indocyanine green and infrared ray laparoscopy system for gastric cancer. Gastric Cancer. 2012;15(3):287–91. https://doi.org/10.1007/s10120-011-0105-6.
Ozawa Y, Murakami M, Watanabe M, Yoshizawa S, Goto S, Otsuka K et al. Preoperative colonic cancer tattooing using the near-infrared fluorescence laparoscopic imaging system. Asian J Endosc Surg. 2016;9(4):340–3. https://doi.org/10.1111/ases.12306.
Watanabe M, Murakami M, Ozawa Y, Yoshizawa S, Matsui N, Aoki T. Intraoperative identification of colonic tumor sites using a near-infrared fluorescence endoscopic imaging system and indocyanine green. Digestive Surgery. 2017;34(6):495–501. https://doi.org/10.1159/000458450.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20(1):1–19. https://doi.org/10.1007/s10120-016-0622-4.
Hamabe A, Omori T, Tanaka K, Nishida T. Comparison of long-term results between laparoscopy-assisted gastrectomy and open gastrectomy with D2 lymph node dissection for advanced gastric cancer. Surg Endosc. 2012;26(6):1702–9. https://doi.org/10.1007/s00464-011-2096-0.
Kanaya S, Kawamura Y, Kawada H, Iwasaki H, Gomi T, Satoh S et al. The delta-shaped anastomosis in laparoscopic distal gastrectomy: analysis of the initial 100 consecutive procedures of intracorporeal gastroduodenostomy. Gastric Cancer. 2011;14(4):365–71. https://doi.org/10.1007/s10120-011-0054-0.
Kitagami H, Morimoto M, Nozawa M, Nakamura K, Tanimura S, Murakawa K et al. Evaluation of the delta-shaped anastomosis in laparoscopic distal gastrectomy: midterm results of a comparison with Roux-en-Y anastomosis. Surg Endosc. 2014;28(7):2137–44. https://doi.org/10.1007/s00464-014-3445-6.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Japanese Gastric Cancer A. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14(2):101–12. https://doi.org/10.1007/s10120-011-0041-5.
Squires MH, 3rd, Kooby DA, Pawlik TM, Weber SM, Poultsides G, Schmidt C et al. Utility of the proximal margin frozen section for resection of gastric adenocarcinoma: a 7-Institution Study of the US Gastric Cancer Collaborative. Ann Surg Oncol. 2014;21(13):4202–10. https://doi.org/10.1245/s10434-014-3834-z.
Kim MG, Lee JH, Ha TK, Kwon SJ. The distance of proximal resection margin dose not significantly influence on the prognosis of gastric cancer patients after curative resection. Annals of Surgical Treatment and Research. 2014;87(5):223–31. https://doi.org/10.4174/astr.2014.87.5.223.
Bissolati M, Desio M, Rosa F, Rausei S, Marrelli D, Baiocchi GL et al. Risk factor analysis for involvement of resection margins in gastric and esophagogastric junction cancer: an Italian multicenter study. Gastric Cancer. 2017;20(1):70–82. https://doi.org/10.1007/s10120-015-0589-6.
Hur H, Son SY, Cho YK, Han SU. Intraoperative gastroscopy for tumor localization in laparoscopic surgery for gastric adenocarcinoma. Journal of Visualized Experiments: JoVE. 2016(114). https://doi.org/10.3791/53170.
Xuan Y, Hur H, Byun CS, Han SU, Cho YK. Efficacy of intraoperative gastroscopy for tumor localization in totally laparoscopic distal gastrectomy for cancer in the middle third of the stomach. Surg Endosc. 2013;27(11):4364–70. https://doi.org/10.1007/s00464-013-3042-0.
Nimura H, Narimiya N, Mitsumori N, Yamazaki Y, Yanaga K, Urashima M. Infrared ray electronic endoscopy combined with indocyanine green injection for detection of sentinel nodes of patients with gastric cancer. Br J Surg. 2004;91(5):575–9. https://doi.org/10.1002/bjs.4470.
Kinami S, Oonishi T, Fujita J, Tomita Y, Funaki H, Fujita H et al. Optimal settings and accuracy of indocyanine green fluorescence imaging for sentinel node biopsy in early gastric cancer. Oncology Letters. 2016;11(6):4055–62. https://doi.org/10.3892/ol.2016.4492.
Miyashiro I, Kishi K, Yano M, Tanaka K, Motoori M, Ohue M et al. Laparoscopic detection of sentinel node in gastric cancer surgery by indocyanine green fluorescence imaging. Surg Endosc. 2011;25(5):1672–6. https://doi.org/10.1007/s00464-010-1405-3.
Tummers Q, Boogerd LSF, de Steur WO, Verbeek FPR, Boonstra MC, Handgraaf HJM et al. Near-infrared fluorescence sentinel lymph node detection in gastric cancer: a pilot study. World Journal of Gastroenterology. 2016;22(13):3644–51. https://doi.org/10.3748/wjg.v22.i13.3644.
Yoshida M, Kubota K, Kuroda J, Ohta K, Nakamura T, Saito J et al. Indocyanine green injection for detecting sentinel nodes using color fluorescence camera in the laparoscopy-assisted gastrectomy. Journal of Gastroenterology and Hepatology. 2012;27 Suppl 3:29–33. https://doi.org/10.1111/j.1440-1746.2012.07067.x.
Hiratsuka M, Miyashiro I, Ishikawa O, Furukawa H, Motomura K, Ohigashi H et al. Application of sentinel node biopsy to gastric cancer surgery. Surgery. 2001;129(3):335–40. https://doi.org/10.1067/msy.2001.111699.
Miyashiro I. What is the problem in clinical application of sentinel node concept to gastric cancer surgery? Journal of Gastric Cancer. 2012;12(1):7–12. https://doi.org/10.5230/jgc.2012.12.1.7.
Miyashiro I, Hiratsuka M, Kishi K, Takachi K, Yano M, Takenaka A et al. Intraoperative diagnosis using sentinel node biopsy with indocyanine green dye in gastric cancer surgery: an institutional trial by experienced surgeons. Ann Surg Oncol. 2013;20(2):542–6. https://doi.org/10.1245/s10434-012-2608-8.
Miyashiro I, Hiratsuka M, Sasako M, Sano T, Mizusawa J, Nakamura K et al. High false-negative proportion of intraoperative histological examination as a serious problem for clinical application of sentinel node biopsy for early gastric cancer: final results of the Japan Clinical Oncology Group multicenter trial JCOG0302. Gastric Cancer. 2014;17(2):316–23. https://doi.org/10.1007/s10120-013-0285-3.
McArthur CS, Roayaie S, Waye JD. Safety of preoperation endoscopic tattoo with india ink for identification of colonic lesions. Surg Endosc. 1999;13(4):397–400.
Author information
Authors and Affiliations
Contributions
Ushimaru designed the study and wrote the initial draft of the manuscript. Omori contributed to the interpretation of the data and to the critical revision of the manuscript for important intellectual content. All the other authors (Fujiwara, Yanagimoto, Sugimura, Yamamoto, Moon, Miyata, Ohue, and Yano) contributed to data collection and interpretation and critical review of the manuscript. All the authors have read and approved the final version of the manuscript and have agreed to the accountability of all aspects of the study, ensuring that any queries related to the accuracy or integrity of any part of the work are answerable.
Corresponding author
Ethics declarations
This study was approved by the Institutional Review Board of the Osaka International Cancer Institute. All patients signed a written informed consent. Data collection and analysis were performed in compliance with the Helsinki Declaration of 1975.
Disclosures
Drs. Yuki Ushimaru, Takeshi Omori, Yoshiyuki Fujiwara, Yoshitomo Yanagimoto, Keijiro Sugimura, Kazuyoshi Yamamoto, Jeong-Ho Moon, Hiroshi Miyata, Masayuki Ohue, and Masahiko Yano have no conflicts of interest or financial ties to declare.
Conflict of Interest
There are no funding sources for this study or any associated financial conflicts.
Rights and permissions
About this article
Cite this article
Ushimaru, Y., Omori, T., Fujiwara, Y. et al. The Feasibility and Safety of Preoperative Fluorescence Marking with Indocyanine Green (ICG) in Laparoscopic Gastrectomy for Gastric Cancer. J Gastrointest Surg 23, 468–476 (2019). https://doi.org/10.1007/s11605-018-3900-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3900-0