Abstract
Background
Current National Comprehensive Cancer Network guidelines for resectable small bowel neuroendocrine tumors (NETs) recommend regional lymphadenectomy. However, no consensus exists on the optimal nodal harvest.
Methods
The National Cancer Database was queried for patients with resectable small bowel NETs (1998–2013). Patients with metastatic disease and missing lymph node harvest data were excluded. We performed logistic regression of factors determining nodal positivity and multivariable survival analyses.
Results
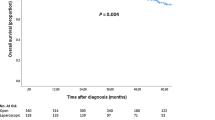
Of 11,852 patients, 81.8% underwent lymphadenectomy. 79.3% were node positive (N+) and 46.9% of patients had tumors < 1 cm. Independent predictors of N+ were large tumor size, ileal location, and neuroendocrine carcinoma histology. Logistic regression found no difference between observed and expected proportions of N+ patients with lymphadenectomy greater than or equal to eight nodes. Lower metastatic node ratio predicted improved survival on multivariable analysis and is associated with high-volume institutions.
Conclusion
Small bowel NETs have high rates of nodal metastasis, even in patients with small tumors, and many patients do not undergo lymphadenectomy despite the clear benefit. Lymphadenectomy of eight nodes is optimal to identify N+ patients. Additionally, minimizing metastatic node ratio with complete regional lymphadenectomy is associated with improved survival in these patients.



Similar content being viewed by others
References
Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008; 26 (18):3063–72.
Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003; 97(4):934–59.
National Comprehensive Cancer Network. Neuroendocrine tumor (Version 2.2017). https://www.nccn.org/professionals/physician_gls/PDF/neuroendocrine.pdf. Accessed April 9, 2017.
Moertel CG, Weiland LH, Nagorney DM, Dockerty MB. Carcinoid tumor of the appendix: treatment and prognosis. N Engl J Med. 1987; 317 (27):1699–701.
Soga J. Carcinoids of the rectum: an evaluation of 1271 reported cases. Surg Today. 1997; 27(2):112–9.
Walsh JC, Schaeffer DF, Kirsch R, Pollett A, Manzoni M, Riddell RH et al. Ileal “carcinoid” tumors-small size belies deadly intent: high rate of nodal metastasis in tumors </=1 cm in size. Hum Pathol. 2016;56:123–7.
Watzka FM, Fottner C, Miederer M, Weber MM, Schad A, Lang H et al. Surgical treatment of NEN of small bowel: a retrospective analysis. World J Surg. 2016; 40(3):749–58.
Marchet A, Mocellin S, Ambrosi A, Morgagni P, Garcea D, Marrelli D et al. The ratio between metastatic and examined lymph nodes (N ratio) is an independent prognostic factor in gastric cancer regardless of the type of lymphadenectomy: results from an Italian multicentric study in 1853 patients. Ann Surg. 2007; 245(4):543–52.
Wang J, Dang P, Raut CP, Pandalai PK, Maduekwe UN, Rattner DW et al. Comparison of a lymph node ratio-based staging system with the 7th AJCC system for gastric cancer: analysis of 18,043 patients from the SEER database. Ann Surg. 2012; 255(3):478–85.
Bilimoria KY, Stewart AK, Winchester DP, Ko CY. The National Cancer Data Base: a powerful initiative to improve cancer care in the United States. Ann Surg. Oncol. 2008; 15(3):683–690.
Miller R, Siegmund D. Maximally selected chi square statistics. Biometrics. 1982; 38(4):1011–6.
Smith DD, Schwarz RR, Schwarz RE. Impact of total lymph node count on staging and survival after gastrectomy for gastric cancer: data from a large US-population database. J Clin. Oncol. 2005; 23 (28):7114–24.
Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. Journal of the American Statistical Association. 1958;53(282):457–81.
Truong C, Wong JH, Lum SS, Morgan JW, Roy-Chowdhury S. The impact of hospital volume on the number of nodes retrieved and outcome in colorectal cancer. Am Surg. 2008;74(10):944–947.
Kulke MH, Mayer RJ. Carcinoid tumors. N Engl J Med. 1999;340(11):858–868.
Norlen O, Stalberg P, Oberg K, et al. Long-term results of surgery for small intestinal neuroendocrine tumors at a tertiary referral center. World J Surg. 2012;36:1419–1431.
Landry CS, Lin HY, Abdalla EK, et al. Resection of at-risk mesenteric lymph nodes is associated with improved survival in patients with small bowel neuroendocrine tumors. World J Surg. 2013;37(7) 1695–700.
Pasquer A, Walter T, Hervieu V, et al. Surgical management of small bowel neuroendocrine tumors: specific requirements and their impact on staging and prognosis. Ann Surg Oncol. 2015;(March):742–749.
Asch SM, Kerr EA, Keesey J, et al. Who is at greatest risk for receiving poor-quality health care? N Engl J Med. 2006;354(11):1147–1156.
Celie K-B, Jackson C, Agrawal S, et al. Socioeconomic and gender disparities in anal cancer diagnosis and treatment. Surg Oncol. 2017;26(2):212–217.
Al-Refaie WB, Gay G, Virnig BA, et al. Variations in gastric cancer care: a trend beyond racial disparities. Cancer. 2010;116(2):465–475.
Ayanian JZ, Kohler BA, Abe T, Epstein AM. The relation between health insurance coverage and clinical outcomes among women with breast cancer. N Engl J Med. 1993;329(5):326–331.
Acknowledgements
The authors acknowledge Jill J. Jurgensen for editing assistance.
The authors acknowledge I’sis N. Perry for providing administrative support.
Author information
Authors and Affiliations
Contributions
Study conception and design: Salo, Hill, and Motz.
Acquisition of data: Salo, Motz, and Boselli.
Analysis and interpretation of data: Salo, Motz, Boselli, and Lorimer.
Drafting of manuscript: Motz, Lorimer, Salo, and Boselli.
Critical revision: Motz, Lorimer, Salo, and Hill.
Approval of final version to be submitted: all authors.
Corresponding author
Rights and permissions
About this article
Cite this article
Motz, B.M., Lorimer, P.D., Boselli, D. et al. Optimal Lymphadenectomy in Small Bowel Neuroendocrine Tumors: Analysis of the NCDB. J Gastrointest Surg 22, 117–123 (2018). https://doi.org/10.1007/s11605-017-3524-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-017-3524-9