Abstract
Background
Laparoscopic ileal pouch-anal anastomosis (L-IPAA) has been increasingly adopted over the last decade due to short-term patient-related benefits. Several studies have shown L-IPAA to be equivalent to open IPAA in terms of safety and short-term outcomes. However, few L-IPAA studies have examined long-term functional outcomes. We aimed to evaluate the long-term functional outcomes of L-IPAA as compared to open IPAA.
Methods
A previous case-matched cohort study at our institution compared short-term outcomes between L-IPAA and open IPAA from 1998 to 2004. For this study, we selected all patients from this case-matched cohort study with chronic ulcerative colitis (CUC) who had follow-up functional data of greater than 1 year. Functional data was obtained through prospective surveys, which were sent annually to all IPAA patients postoperatively.
Results
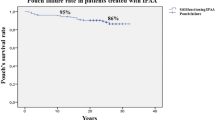
One hundred and forty-nine patients (58 L-IPAA, 91 open IPAA) with a median 8-year duration of follow-up were identified. There were no differences in demographics and long-term surgical outcomes between groups. Stapled anastomosis was more common in the laparoscopic group (91.4 versus 54.9%, p < 0.001). Stool frequency during daytime (>6 stools, L-IPAA 32.8%, open 49.4%, p = 0.048) and nighttime (>2 stools, L-IPAA 13.8%, open 30.6%; p = 0.024) was significantly lower in the L-IPAA group. Ability to differentiate gas from stool was not different (p = 0.13). Rate of complete continence was similar in L-IPAA and open groups (L-IPAA 36.2%, open 21.8%, p = 0.060). There was no difference in use of medication to control stools, perianal skin irritation, voiding difficulty, sexual problems, and occupational change between groups. Subgroup analysis to evaluate for any group differences attributable to anastomotic technique demonstrated only that stapled anastomoses lead to more perianal skin irritation in the L-IPAA group (L-IPAA = 60.4% versus open IPAA = 38.8%; p = 0.031).
Conclusion
Overall, L-IPAA has comparable functional results to the open approach with slightly lower daytime and nighttime stool frequency. This difference may be attributed to a greater number of stapled anastomoses performed in the laparoscopic cohort.
Similar content being viewed by others
References
Parks AG, Nicholls RJ. Proctocolectomy without ileostomy for ulcerative colitis. Br Med J. 1978;2(6130):85–88.
Pandey S, Luther G, Umanskiy K, et al. Minimally invasive pouch surgery for ulcerative colitis: is there a benefit in staging? Dis Colon Rectum. 2011;54(3):306–310.
Larson DW, Cima RR, Dozois EJ, et al. Safety, feasibility, and short-term outcomes of laparoscopic ileal-pouch-anal anastomosis: a single institutional case-matched experience. Ann Surg. 2006;243(5):667–670.
Linden BC, Bairdain S, Zurakowski D, Shamberger RC, Lillehei CW. Comparison of laparoscopic-assisted and open total proctocolectomy and ileal pouch anal anastomosis in children and adolescents. J Pediatr Surg. 2013;48(7):1546–1550.
Wu XJ, He XS, Zhou XY, Ke J, Lan P. The role of laparoscopic surgery for ulcerative colitis: systematic review with meta-analysis. Int J Colorectal Dis. 2010;25(8):949–957.
Fleming FJ, Francone TD, Kim MJ, Gunzler D, Messing S, Monson JR. A laparoscopic approach does reduce short-term complications in patients undergoing ileal pouch-anal anastomosis. Dis Colon Rectum. 2011;54(2):176–182.
Polle SW, Dunker MS, Slors JF, et al. Body image, cosmesis, quality of life, and functional outcome of hand-assisted laparoscopic versus open restorative proctocolectomy: long-term results of a randomized trial. Surg Endosc. 2007;21(8):1301–1307.
Baek SJ, Dozois EJ, Mathis KL, et al. Safety, feasibility, and short-term outcomes in 588 patients undergoing minimally invasive ileal pouch-anal anastomosis: a single-institution experience. Tech Coloproctol. 2016;20(6):369–374.
Fichera A, Silvestri MT, Hurst RD, Rubin MA, Michelassi F. Laparoscopic restorative proctocolectomy with ileal pouch anal anastomosis: a comparative observational study on long-term functional results. J Gastrointest Surg. 2009;13(3):526–532.
Dunker MS, Bemelman WA, Slors JF, van Duijvendijk P, Gouma DJ. Functional outcome, quality of life, body image, and cosmesis in patients after laparoscopic-assisted and conventional restorative proctocolectomy: a comparative study. Dis Colon Rectum. 2001;44(12):1800–1807.
Michelassi F, Lee J, Rubin M, et al. Long-term functional results after ileal pouch anal restorative proctocolectomy for ulcerative colitis: a prospective observational study. Ann Surg. 2003;238(3):433–441.
Carmon E, Keidar A, Ravid A, Goldman G, Rabau M. The correlation between quality of life and functional outcome in ulcerative colitis patients after proctocolectomy ileal pouch anal anastomosis. Colorectal Dis. 2003;5(3):228–232.
Lichtenstein GR, Cohen R, Yamashita B, Diamond RH. Quality of life after proctocolectomy with ileoanal anastomosis for patients with ulcerative colitis. J Clin Gastroenterol. 2006;40(8):669–677.
Meagher AP, Farouk R, Dozois RR, Kelly KA, Pemberton JH. J ileal pouch-anal anastomosis for chronic ulcerative colitis: complications and long-term outcome in 1310 patients. Br J Surg. 1998;85(6):800–803.
Foley EF, Schoetz DJ, Jr., Roberts PL, et al. Rediversion after ileal pouch-anal anastomosis: causes of failures and predictors of subsequent pouch salvage. Dis Colon Rectum. 1995;38(8):793–798.
Korsgen S, Keighley MR. Causes of failure and life expectancy of the ileoanal pouch. Int J Colorectal Dis. 1997;12(1):4–8.
MacRae HM, McLeod RS, Cohen Z, O’Connor BI, Ton EN. Risk factors for pelvic pouch failure. Dis Colon Rectum. 1997;40(3):257–262.
Gemlo BT, Wong WD, Rothenberger DA, Goldberg SM. Ileal pouch-anal anastomosis: patterns of failure. Arch Surg. 1992;127(7):784–786.
Setti-Carraro P, Ritchie JK, Wilkinson KH, Nicholls RJ, Hawley PR. The first 10 years’ experience of restorative proctocolectomy for ulcerative colitis. Gut. 1994;35(8):1070–1075.
Remzi FH, Church JM, Bast J, et al. Mucosectomy vs. stapled ileal pouch-anal anastomosis in patients with familial adenomatous polyposis: functional outcome and neoplasia control. Dis Colon Rectum. 2001;44(11):1590–1596.
Kirat HT, Remzi FH, Kiran RP, Fazio VW. Comparison of outcomes after hand-sewn versus stapled ileal pouch-anal anastomosis in 3,109 patients. Surgery. 2009;146(4):723–729.
Lovegrove RE, Constantinides VA, Heriot AG, et al. A comparison of hand-sewn versus stapled ileal pouch anal anastomosis (IPAA) following proctocolectomy: a meta-analysis of 4183 patients. Ann Surg. 2006;244(1):18–26.
Hahnloser D, Pemberton JH, Wolff BG, Larson DR, Crownhart BS, Dozois RR. Results at up to 20 years after ileal pouch-anal anastomosis for chronic ulcerative colitis. Br J Surg. 2007;94(3):333–340.
Authors’ Contributions
All authors listed meet all four criteria for authorship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Baek, SJ., Lightner, A.L., Boostrom, S.Y. et al. Functional Outcomes Following Laparoscopic Ileal Pouch-Anal Anastomosis in Patients with Chronic Ulcerative Colitis: Long-Term Follow-up of a Case-Matched Study. J Gastrointest Surg 21, 1304–1308 (2017). https://doi.org/10.1007/s11605-017-3411-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-017-3411-4