Abstract
Background
Organ/space surgical site infections (OSIs) constitute an important postoperative metric. We sought to assess the impact of a previously described air leak test (ALT) on the incidence of OSI following major hepatectomies.
Methods
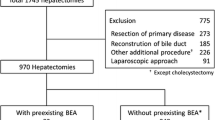
A single-institution hepatobiliary database was queried for patients who underwent a major hepatectomy without biliary-enteric anastomosis between January 2009 and June 2015. Demographic, clinicopathologic, and intraoperative data—including application of ALT—were analyzed for associations with postoperative outcomes, including OSI, hospital length of stay (LOS), morbidity and mortality rates, and readmission rates.
Results
Three hundred eighteen patients were identified who met inclusion criteria, of whom 210 had an ALT. ALT and non-ALT patients did not differ in most disease and treatment characteristics, except for higher rates of trisegmentectomy among ALT patients (53 vs. 34 %, p = 0.002). ALT patients experienced lower rates of OSI and 90-day morbidity than non-ALT patients (5.2 vs. 13.0 %, p = 0.015 and 24.8 vs. 40.7 %, p = 0.003, respectively). In turn, OSI was the strongest independent predictor of longer LOS (OR = 4.89; 95 % CI, 2.80–6.97) and higher rates of 30- (OR = 32.0; 95 % CI, 10.9–93.8) and 45-day readmissions (OR = 29.4; 95 % CI, 10.2–84.6).
Conclusions
The use of an intraoperative ALT significantly reduces the rate of OSI following major hepatectomy and may contribute to lower post-discharge readmission rates.


Similar content being viewed by others
References
Dimick JB, Wainess RM, Cowan JA, Upchurch GR Jr, Knol JA, Colletti LM. National trends in the use and outcomes of hepatic resection. J Am Coll Surg 2004;199:31–38.
Cescon M, Vetrone G, Grazi GL, Ramacciato G, Ercolani G, Ravaioli M, Del Gaudio M, Pinna AD. Trends in perioperative outcome after hepatic resection: analysis of 1500 consecutive unselected cases over 20 years. Ann Surg 2009;249:995–1002.
Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, Corvera C, Weber S, Blumgart LH. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg 2002;236:397–406.
Minagawa M, Makuuchi M, Takayama T, Kokudo N. Selection criteria for repeat hepatectomy in patients with recurrence hepatocellular carcinoma. Ann Surg 2003;238:703–710.
Horan TC, Gaynes Rp, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol 1992;13:606–608.
Panni RZ, Hall BL, Chapman WC, Strasberg SM. Standardizing a control group for comparing open with laparoscopic major liver resection in observational studies: reducing the need for correction of clinical heterogeneity. J Am Coll Surg 2014;219:1124–1133.
Zimmitti G, Vauthey JN, Shindoh J, Tzeng CW, Roses RE, Ribero D, Capussotti L, Giuliante F, Nuzzo G, Aloia TA. Systematic use of an intraoperative air leak test at the time of major liver resection reduces the rate of postoperative biliary complications. J Am Coll Surg 2013;217:1028–1037.
Sadamori H, Yagi T, Shinoura S, Umeda Y, Yoshida R, Satoh D, Nobuoka D, Utsumi M, Fujiwara T. Risk factors for major morbidity after liver resection for hepatocellular carcinoma. Br J Surg 2013;100:122–129.
Ribero D, Chun YS, Vauthey JN. Standardized liver volumetry for portal vein embolization. Semin Intervent Radiol 2008;25:104–109.
Madoff DC, Abdalla EK, Vauthey JN. Portal vein embolization in preparation for major hepatic resection: evolution of a new standard of care. J Vasc Interv Radiol 2005;16:779–790.
Shindoh J, Truty MJ, Aloia TA, Curley SA, Zimmitti G, Huang SY, Mahvash A, Gupta S, Wallace MJ, Vauthey JN. Kinetic growth rate after portal vein embolization predicts posthepatectomy outcomes: toward zero liver-related mortality in patients with colorectal liver metastases and small future liver remnant. J Am Coll Surg 2013;216:201–209.
Chang SB, Palavecino M, Wray CJ, Kishi Y, Pisters PW, Vauthey JN. Modified Makuuchi incision for foregut procedures. Arch Surg 2010;145:281–284.
Aloia TA, Zorzi D, Abdalla EK, Vauthey JN. Two-surgeon technique for hepatic parenchymal transection of the noncirrhotic liver using saline-linked cautery and ultrasonic dissection. Ann Surg 2005;242:172–177.
Brudvik KW, Mise Y, Conrad C, Zimmitti G, Aloia TA, Vauthey JN. Definition of readmission in 3,041 patients undergoing hepatectomy. J Am Coll Surg 2015;221:38–46.
Rubbia-Brandt L, Lauwers GY, Wang H, Majno PE, Tanabe K, Zhu AX, Brezault C, Soubrane O, Abdalla EK, Vauthey JN, Mentha G, Terris B. Sinusoidal obstruction syndrome and nodular regenerative hyperplasia are frequent oxaliplatin-associated liver lesions and partially prevented by bevacizumab in patients with hepatic colorectal metastasis. Histopathology 2010;56:430–439.
Anderson DJ, Podgorny K, Berrios-Torres SI, Bratzler DW, Dellinger EP, Greene L, Nyquist AC, Saiman L, Yokoe DS, Maragakis LL, Kaye KS. Strategies to prevent surgical site infections in acute care hospitals: 2014 updates. Infect Control Hosp Epidemiol 2014;35:606–627.
Stulberg JJ, Delaney CP, Neuhauser DV, Aron DC, Fu P, Koroukian SM. Adherence to surgical care improvement project measures and the association with postoperative infections. JAMA 2010;303:2472–2485.
Awad SS. Adherence to surgical care improvement project measures and post-operative surgical site infections. Surg Infect 2012;13:234–237.
Hawn MT, Vick CC, Richman J, Holman W, Deierhoi RJ, Graham LA, Henderson WG, Itani KM. Surgical site infection prevention: time to move beyond the surgical care improvement program. Ann Surg 2011;254:494–499.
Dua A, Desai SS, Seabrook GR, Brown KR, Lewis BD, Rossi PJ, Edmiston CE, Lee CJ. The effect of Surgical Care Improvement Project measures on national trends on surgical site infections in open vascular procedures. J Vasc Surg 2014;60:1635–1639.
Aloia TA, Fahy BN, Fischer CP, Jones SL, Duchini A, Galati J, Gaber AO, Ghobrial RM, Bass BL. Predicting poor outcome following hepatectomy: analysis of 2313 hepatectomies in the NSQIP database. HPB 2009;11:510–515.
Moreno Elola-Olaso A, Davenport DL, Hundley JC, Daily MF, Gedaly R. Predictors of surgical site infection after liver resection: a multicentre analysis using National Surgical Quality Improvement Program data. HPB 2012;14:136–141
Pitt HA, Kilbane M, Strasberg SM, Pawlik TM, Dixon E, Zyromski NJ, Aloia TA, Henderson JM, Mulvihill SJ. ACS-NSQIP has the potential to create an HPB-NSQIP option. HPB 2009;11:405–413.
Spolverato G, Ejaz A, Kim Y, Hall BL, Bilimoria K, Cohen M, Ko C, Pitt H, Pawlik TM. Patterns of care among patients undergoing hepatic resection: a query of the national Surgical Quality Improvement Program-targeted hepatectomy database. J Surg Res 2015;196:221–228.
Yamashita Y, Hamatsu T, Rikimaru T, Tanaka S, Shirabe K, Shimada M, Sugimachi K. Bile leakage after hepatic resection. Ann Surg 2001;233:45–50.
Zimmitti G, Roses RE, Andreou A, Shindoh J, Curley SA, Aloia TA, Vauthey JN. Greater complexity of liver surgery is not associated with an increased incidence of liver-related complications except for bile leak: an experience with 2,628 consecutive resections. J Gastrointest Surg 2013;17:57–64.
All authors have granted final approval of the version to be published and agree to be held accountable for all aspects of the work and its accuracy and integrity.
Author Contribution
Study concept and design: Tran Cao, Conrad, Aloia, Vauthey
Acquisition of data: Tran Cao, Phuoc, Ismael, Passot, Yamashita
Analysis and interpretation: Tran Cao, Vauthey
Drafting of manuscript: Tran Cao, Vauthey
Critical revisions: Tran Cao, Phuoc, Ismael, Denbo, Passot, Yamashita, Conrad, Aloia, Vauthey
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tran Cao, H.S., Phuoc, V., Ismael, H. et al. Rate of Organ Space Infection Is Reduced with the Use of an Air Leak Test During Major Hepatectomies. J Gastrointest Surg 21, 85–93 (2017). https://doi.org/10.1007/s11605-016-3209-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3209-9