Abstract
Background
Endoscopic and interventional techniques are currently the mainstay of management of bleeding duodenal ulcer. As well, for patients with perforated duodenal ulcer, laparoscopic simple closure is nowadays usually performed. Although indications for emergency antroduodenectomy have declined, this procedure is still necessary as a salvage option when conservative management has failed or is not practicable. Our study aimed to evaluate indications and results of antroduodenectomy with gastroduodenal anastomosis in current practice and to examine the factors that predict operative outcomes.
Methods
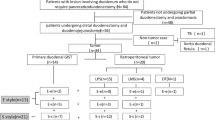
All patients who underwent emergency antroduodenectomy with gastroduodenal anastomosis in two surgical care departments specialized in emergency digestive surgery were studied from 2000 to 2015.
Results
Thirty-five patients (27 males, 77 %) with a median age of 68 years (20–90) underwent emergency antroduodenectomy with gastroduodenal anastomosis. Indications were bleeding and perforated duodenal ulcer in 24 and 11 patients, respectively. The overall complication rate was 69 %, especially because of a high rate of medical complications (57 %). Only two patients (6 %) required reoperation for anastomotic leakage. The overall mortality rate was 40 % (n = 14). According to the univariate analysis, age >70, >3 comorbidities, ASA score >2, and postoperative medical complications were associated with an increased risk of in-hospital mortality. In the multivariate analysis, age and ASA score remained independent risk factors. No recurrence of complicated duodenal disease was observed.
Conclusion
Antroduodenectomy with gastroduodenal anastomosis is a safe and effective long-term strategy, with a low and acceptable rate of surgical complications, for complicated duodenal ulcer not responding to conservative measures.


Similar content being viewed by others
References
Paimela H, Oksala NK, Kivilaakso E. Surgery for peptic ulcer today. A study on the incidence, methods and mortality in surgery for peptic ulcer in Finland between 1987 and 1999. Dig Surg 2004;21:185–91.
Svanes C. Trends in perforated peptic ulcer: incidence, etiology, treatment, and prognosis. World J Surg 2000;24:277–83.
Millat B, Hay JM, Valleur P, Fingerhut A, Fagniez PL. Emergency surgical treatment for bleeding duodenal ulcer: oversewing plus vagotomy versus gastric resection, a controlled randomized trial. French Associations for Surgical Research. World J Surg. 1993 Sep-Oct;17(5):568–73;
Poxon VA, Keighley MR, Dykes PW, Heppinstall K, Jaderberg M. Comparison of minimal and conventional surgery in patients with bleeding peptic ulcer: a multicentre trial. Br J Surg. 1991 Nov;78(11):1344–5
Dousset B, Suc B, Boudet MJ, Cherqui D, Rotman N, Julien M, Fagniez PL. Surgical treatment of severe ulcerous hemorrhages: predictive factors of operative mortality. Gastroenterol Clin Biol. 1995 Mar;19(3):259–65.
Imhof M, Epstein S, Ohmann C, Röher HD. Poor late prognosis of bleeding peptic ulcer. Langenbecks Arch Surg. 2007 Sep;392(5):587–91.
Nahon S, Pariente A; group of investigators of the ANGH (Association Nationale des Gastroentérologues des Hôpitaux Généraux). Impact of comorbidity on mortality in patients with peptic ulcer bleeding: confirmative data of a French prospective study. Am J Gastroenterol. 2013 Sep;108(9):1532–3.
Leontiadis GI, Molloy-Bland M, Moayyedi P et al. Effect of comorbidity on mortality in patients with peptic ulcer bleeding: systematic review and meta analysis . Am J Gastroenterol 2013; 108 : 331 – 45
De la Fuente SG, Khuri SF, Schifftner T, Henderson WG, Mantyh CR, Pappas TN. Comparative analysis of vagotomy and drainage versus vagotomy and resection procedures for bleeding peptic ulcer disease: results of 907 patients from the Department of Veterans Affairs National Surgical Quality Improvement Program database. J Am Coll Surg. 2006 Jan;202(1):78–86
Dubois F (1971) Gastrectomy and gastroduodenal anastomosis for post-bulbar ulcers and peptic ulcers of the second part of the duodenum. J Chir 101:177–186
Loffroy R. Management of duodenal ulcer bleeding resistant to endoscopy: surgery is dead! World J Gastroenterol. 2013 Feb 21;19(7):1150–1
Wu X, Zen D, Xu S, Zhang L, Wang P. A modified surgical technique for the emergent treatment of giant ulcers concomitant with hemorrhage in the posterior wall of the duodenal bulb. Am J Surg. 2002 Jul;184(1):41–4
Guinier D, Destrumelle N, Denue PO, Mathieu P, Heyd B, Mantion GA. Technique of antroduodenectomy without ulcer excision as a safe alternative treatment for bleeding chronic duodenal ulcers. World J Surg. 2009 May;33(5):1010–4
Oh SJ, Choi WB, Song J, Hyung WJ, Choi SH, Noh SH. Complications requiring reoperation after gastrectomy for gastric cancer: 17 years experience in a single institute. J Gastrointest Surg 2009; 13: 239–245
Takahashi T, Yamamura T, Utsunomiya J. Pathogenesis of acute cholecystitis after gastrectomy. Br J Surg 1990; 77:536–539
Yi S, Ohta T, Tsuchida A et al. (2007) Surgical anatomy of innervation of the gallbladder in humans and Suncus murinus with special reference to morphological understanding of gallstone formation after gastrectomy. World J Gastroenterol 13: 2066–2071
Gutierrez de la Pena C, Marquez R, Fakih F, Dominguez-Adame E, Medina J. Simple closure or vagotomy and pyloroplasty for the treatment of a perforated duodenal ulcer: comparison of results. Dig Surg 2000; 17: 225–228
Lee YT, Sung JJ, Choi CL, Chan FK, Ng EK, Ching JY et al. Ulcer recurrence after gastric surgery: is Helicobacter pylori the culprit? Am J Gastroenterol 1998; 93: 928–931
Lau JY, Sung JJ, Lam YH, et al. Endoscopic retreatment compared with surgery in patients with recurrent bleeding after initial endoscopic control of bleeding ulcers. N Engl J Med 1999;340:751–6.
So JB, Yam A, Cheah WK, Kum CK, Goh PM. Risk factors related to operative mortality and morbidity in patients undergoing emergency gastrectomy. Br J Surg 2000;87:1702–7.
Hunt PS, McIntyre RL. Choice of emergency operative procedure for bleeding duodenal ulcer. Br J Surg. 1990 Sep;77(9):1004–6.
Kumar K, Pai D, Srinivasan K, Jagdish S, Ananthakrishnan N. Factors contributing to releak after surgical closure of perforated duodenal ulcer by Graham’s Patch. Trop Gastroenterol 2002;23:190–2.
Sillakivi T, Lang A, Tein A, Peetsalu A. Evaluation of risk factors for mortality in surgically treated perforated peptic ulcer. Hepatogastroenterology 2000;47:1765–8.
Kocer B, Surmeli S, Solak C, et al. Factors affecting mortality and morbidity in patients with peptic ulcer perforation. J Gastroenterol Hepatol 2007;22:565–70.
Schwarze ML, Barnato AE, Rathouz PJ, Zhao Q, Neuman HB, Winslow ER, Kennedy GD, Hu YY, Dodgion CM, Kwok AC, Greenberg CC. Development of a list of high-risk operations for patients 65 years and older. JAMA Surg. 2015 Apr;150(4):325–31.
Quan S, Frolkis A, Milne K, Molodecky N, Yang H, Dixon E, Ball CG, Myers RP, Ghosh S, Hilsden R, van Zanten SV, Kaplan GG. Upper-gastrointestinal bleeding secondary to peptic ulcer disease: incidence and outcomes. World J Gastroenterol. 2014 Dec 14;20(46):17568–77
Rosenstock SJ, Møller MH, Larsson H, Johnsen SP, Madsen AH, Bendix J, Adamsen S, Jensen AG, Zimmermann-Nielsen E, Nielsen AS, Kallehave F, Oxholm D, Skarbye M, Jølving LR, Jørgensen HS, Schaffalitzky de Muckadell OB, Thomsen RW. Improving quality of care in peptic ulcer bleeding: nationwide cohort study of 13,498 consecutive patients in the Danish Clinical Register of Emergency Surgery. Am J Gastroenterol. 2013 Sep;108(9):1449–57
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Chereau, N., Chandeze, MM., Tantardini, C. et al. Antroduodenectomy with Gastroduodenal Anastomosis: Salvage Emergency Surgery for Complicated Peptic Ulcer Disease—Results of a Double Institution Study of 35 Patients. J Gastrointest Surg 20, 539–545 (2016). https://doi.org/10.1007/s11605-015-3050-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-3050-6