Abstract
Introduction
Introduction of total mesorectal excision (TME) surgery for rectal cancer decreased local recurrence dramatically. Additional neoadjuvant chemoradiation (nCR) is frequently given in UICC II and III tumors based on TNM staging which is of limited accuracy. We aimed to evaluate determination of circumferential margin by magnetic resonance imaging (mrCRM) as an alternative criterium for nCR.
Methods
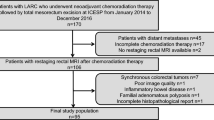
Multicenter prospective cohort study which enrolled 642 patients in 13 centers with non-metastasized rectal adenocarcinoma. Patients with T4 tumors or patients with a mrCRM of 1 mm or less were treated by neoadjuvant chemoradiation. All others proceeded directly to surgery when inclusion criteria and no exclusion criteria were met. Quality of TME and accuracy of mrCRM determination were assessed during pathology workup.
Results
TME was complete in 381 of 389 patients after surgery without nCR (97.9 %) and in 245 of 253 patients (96.8 %) after nCR. Negative pathology circumferential margins (pCRM) were seen in 97.4 % without nCR and in 89 % of patients after nCR. Negative pCRM was predicted by negative mrCRM in 98.3 % of rectal cancers. NCR was given to 253 of 642 patients (39.5 %). Lymph node count was 23 (range 7–79; median/range) for surgery without nCR and 19 (range 2–56) for surgery after nCR.
Conclusions
Surgical quality determined by pathology workup of specimen was very good in this study. Magnetic resonance imaging guided indication for nCR allows to achieve superb results concerning surrogate parameters for good oncological outcome. Thus, use of neoadjuvant chemoradiation with its potential detrimental side effects may be substantially reduced in selected patients.


Similar content being viewed by others
References
Kaul S, Diamond GA. Good enough: a primer on the analysis and interpretation of non-inferiority trials. Ann Intern Med 2006; 145: 62–69.
Pox C, Aretz S, Bischoff SC, Graeven U, Hass M, Heußner P, Hohenberger W, Holstege A, Hübner J, Kolligs F, Kreis M, Lux P, Ockenga J, Porschen R, Post S, Rahner N, Reinacher-Schick A, Riemann JF, Sauer R, Sieg A, Scheppach W, Schmitt W, Schmoll HJ, Schulmann K, Tannapfel A, Schmiegel W. S3-Guideline colorectal cancer version 1.0. Z Gastroenterol 2013; 51: 753–854.
Enker WE. Designing the optimal surgery for rectal carcinoma. Cancer 1996; 78: 1847–1850.
Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R, Martus P, Tschmelitsch J, Hager E, Hess CF, Karstens JH, Liersch T, Schmidberger H, Raab R; Preoperative versus postoperative chemoradiotherapy for rectal cancer. German Rectal Cancer Study Group. N Engl J med 2004; 351: 1731–40.
Sebag-Montefiore D, Stephens RJ, Steele R, Monson J, Grieve R, Khanna S, Quirke P, Couture J, de Metz C, Myint AS, Bessell E, Griffiths G, Thompson LC, Parmar M. Preoperative radiotherapy versus slelective posopterative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomized trial. Lancet 2009; 373: 811–20.
Junginger T, Hermanek P, Oberholzer K, Schmidberger H. Rektumkarzinom: Behandeln wir zu häufig neoadjuvant? Vorschläge zu einer selektiveren, MRT-basierten Indikation. Zbl Chir 2006; 131: 275–284.
Carne PW, Nelson H. Are we overtreating rectal cancer: time for another trial? Ann Surg Oncol 2004; 11: 124–126.
Hermanek P, Merkel S, Fietkau R, Rödel C, Hohenberger W. Regional lymph node metastasis and locoregional recurrence of rectal carcinoma in the era of TNM surgery. Implications for treatment decisions. Int J Colorectal Dis 2010; 25: 359–68.
Bipat S, Glas AS, Slors FJ, Zwinderman AH, Bossuyt PM, Stoker J. Rectal cancer: local staging and assessment of lymph node involvement with endoluminal US, CT, and MR imaging – a meta analysis. Radiology 2004; 232: 773–83.
Ptok H, Ruppert R, Strassburg J, Maurer CA, Oberholzer K, Junginger T, Merkel S, Hermanek P. Pretherapeutic MRI for decision-making regarding selective neoadjuvant radiochemotherapy for rectal carcinoma: interim analysis of a multicentric prospective observational study. J Magn Reson Imaging 2013; 37: 1122–8.
Kornmann M, Henne-Bruns D. Qualität der Datengrundlage zu Evidence-based Medicine. Rektumkarzinom und präoperative 5x5-Bestrahlung. Zbl Chir 2008; 133: 20–34.
Peeters KC, van de Velde CJ, Leer JW, Martijn H, Junggeburt JM, Kranenbarg EK, Steup WH, Wiggers T, Rutten HJ, Marijnen CA. Late side effects of short-course preoperative radiotherapy combined with total mesorectal excision for rectal cancer: increased bowel dysfunction in irradiated patients--a Dutch colorectal cancer group study. J Clin Oncol 2005; 23: 6199–206.
Pollack J, Holm T, Cedermark B, Holmström B, Mellgren A. Long-term effect of preoperative radiation therapy on anorectal function. Dis Colon Rectum 2006; 49: 345–52.
Gervaz P, Rotholtz N, Pisano M, Kaplan E, Secic M, Coucke P, Pikarsky A, Efron J, Weiss E, Wexner S. Quantitative short-term study of anal sphincter function after chemoradiation for rectal cancer. Arch Surg 2001; 136: 192–6.
Ammann K, Kirchmayr W, Klaus A, Mühlmann G, Kafka R, Oberwalder M, De Vries A, Ofner D, Weiss H. Impact of neoadjuvant chemoradiation on anal sphincter function in patients with carcinoma of the midrectum and low rectum. Arch Surg 2003; 138: 257–61.
Birbeck KF, Macklin CP, Tiffin NJ, Parsons W, Dixon MF, Mapstone NP, Abbott CR, Scott N, Finan PJ, Johnston D, Quirke P. Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann Surg 2002; 35: 449–457.
Bittner R, Burghardt J, Gross E, Grundmann RT, Hermanek P, Isbert C, Junginger T, Köckerling F, Merkel S, Möslein G, Raab HR, Roder J, Ruf G, Schwenk W, Strassburg J, Tannapfel A, de Vries A, Zühlke H. Report on the workshop “workflow rectal cancer II”. Zentralbl Chir 2007; 132: 85–94.
Glynne-Jones R, Mawdsley S, Pearce T, Buyse M. Alternative clinical end points in rectal cancer - are we getting closer? Ann Oncol 2006; 17: 1239–1242.
Mawdsley S, Glynne-Jones R, Grainger J, Richman P, Makris A, Harrison M, Ashford R, Harrison RA, Osborne M, Livingstone JI, MacDonald P, Mitchell IC, Meyrick-Thomas J, Northover JM, Windsor A, Novell R, Wallace M. Can histopathologic assessment of circumferential margin after preoperative pelvic clearance therapy for T3-T4 rectal cancer predict for 3-year disease-free survival? Int J Radiat Oncol Biol Phys 2005; 63: 745–750.
Strassburg J, Junginger T, Trinh T, Püttcher O, Oberholzer K, Heald RJ, Hermanek P. Magnetic resonance imaging (MRI)-based indication for neoadjuvant treatment of rectal carcinoma and the surrogate endpoint CRM status. Int J Colorect Dis 2008; 23: 1099–1107.
Eriksen MT, Wibe A, Haffner J, Wiig JN; Norwegian Rectal Cancer Group. Prognostic groups in 1,676 patients with T3 rectal cancer treated without preoperative radiotherapy. Dis Colon Rectum 2007; 50: 156–67.
Nagtegaal ID, Marijnen CAM, Kranenberg EK, van de Velde CJ, van Krieken JH; Pathology Review Committee; Cooperative Clinical Investigators. Circumferential margin involvement is still an important predictor of local recurrence in rectal carcinoma. Am J Surg Pathol 2002; 26: 350–357.
Brown G, Daniels IR. Preoperative staging of rectal cancer: the MERCURY research project. Recent Results Cancer Research 2005; 165: 58–74
MERCURY Study Group. Diagnostic accuracy of preoperative magnetic resonance imaging in predictiong curative resection of rectal cancer: prospective observational study. Br Med J 2003; 333: 779–784.
Crawshaw A, Hennigan R, Smedley FH, Leslie MD. Perioperative radiotherapy for rectal cancer: the case for a selective pre-operative approach – the third way. Colorectal Disease 2006; 5: 367–372.
Burton S, Brown G, Daniels IR, Normann AR, Mason B, Cunningham D; Royal Marsden Hospital, Colorectal Cancer Network. MRI directed multidisciplinary team preoperative treatment strategy: the way to eliminate positive circumferential margins? Br J Cancer 2006; 94: 351–357.
Engelen S, Lahaye MJ, Beets-Tan RG. Tailored treatment of primary rectal cancer based on MRI: does it reduce the number of incomplete resections? Abstract. Ann Oncol 2008; 19, Suppl 1: i 17.
Chau I, Brown G, Cunningham D, Tait D, Wotherspoon A, Norman AR, Tebbutt N, Hill M, Ross PJ, Massey A, Oates J. Adjuvant capecitabine and oxaliplatin followed by synchronous chemoradiation and total mesorectal excision in magnetic resonance imaging-defined poor-risk rectal cancer. J Clin Oncol 2006; 24: 668–674.
Taylor FG, Quirke P, Heald RJ, Moran BJ, Blomqvist L, Swift IR, Sebag-Montefiore D, Tekkis P, Brown G; Magnetic Resonance Imaging in Rectal Cancer European Equivalence Study Group. Preoperative magnetic resonance imaging assessment of circumferential resection margin predicts disease-free survival and local recurrence: 5-year follow-up results of the MERCURY study. J Clin Oncol. 2014 Jan 1;32(1):34–43.
Battersby NJ, How P, Moran B, Stelzner S, West NP, Branagan G, Strassburg J, Quirke P, Tekkis P, Pdersen BG, Gudgeon M, Heald B, Brown G – on behalf of the MERCURY II Study Group. Prospective validation of a low rectal cancer magnetic resonance imaging staging system and development of a local recurrence risk stratification model. The MERCURY II Study. 2015; March 27th (epub ahead of print).
Strassburg J, Ruppert R, Ptok H et al. MRI-based indications for neoadjuvant radiochemotherapy in rectal cancer: Interim results of a prospective multicenter observational study. Ann Surg Oncol 2011; 18: 2790–2799.
Compton CC. Colorectal carcinoma: diagnostic, prognostic and molecular features. Mod Pathol 2003; 16: 376–385.
Hermanek P, Junginger T. The circumferential margin in rectal carinoma surgery. Tech Coloproctol 2003; 9: 193–200.
Berufsverband deutscher Pathologen und Deutsche Gesellschaft für Pathologie (2007) Anleitungen zur pathologisch-anatomischen Diagnostik des kolorektalen Karzinoms. Vers. 2.0. Berufsverband Deutscher Pathologen, Gelsenkirchen, http://www.bv-pathologie.de.
Quirke P, Steele R, Monson J, Grieve R, Khanna S, Couture J, O’Callaghan C, Myint AS, Bessell E, Thompson LC, Parmari M, Stephens RJ, Sebag-Montefiore D, on behalf of the MRC CR07/NCIC-CTG CO16 trial investigators, and the NCRI colorectal cancer study group. Lancet 2009; 373: 821–828.
Habr-Gama A, Sao Juliao GP, Perez RO. Nonoperative management of rectal cancer: identifying the ideal patient. Hematol Oncol Clin North Am 2015; 29: 135–51.
Acknowledgments
The study received no external funding and was only supported by commitment of surgeons in different centers in Germany and Switzerland.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Primary Discussant
Scott A. Strong, M.D. (Chicago, IL)
1. Guidelines developed by the National Comprehensive Cancer network that are used by many US centers define rectal cancer as tumors within 12 cm of the anal verge because these cancers of the more proximal rectum tend to behave like tumors of the sigmoid colon rather than the more distal rectum. Why were tumors 12–16 cm from the anal verge included in your study?
2. Your overall incidence of negative CRM as predicted by MRI was 64 % whereas the rate in the MERCURY trial was much higher at nearly 80 %. Can you explain the discrepancy?
3. Did the quality of surgery as defined by negative pathologic CRM, lymph node harvest, and completeness of TME vary between the high- and low-volume centers?
Closing Discussant
Dr. Kreis
1. In European studies on rectal cancer, the rectum is defined from 0 to 16 cm from the anal verge. We aimed to render our study results primarily comparable to other European studies, so that this definition was chosen. Furthermore, the UICC defined the rectum in this way (0–16 cm; Wittekind C, Meyer HJ: TNM Klassifikation maligner Tumoren, 7. Auflage. Wiley-VCH, Weinheim 2010).
2. The MERCURY trial included T1 tumors that were not included in our study. As T1 tumors never threaten CRM, patients with this tumor stage will increase the rate of mrCRM negative patients. This and other differences in patient population may explain this discrepancy.
3. We did not observe a difference as regards negative pathologic CRM and completeness of TME. There was a difference between centers concerning lymph node harvest which was, however, not related to hospital volume.
Kreis and Ruppert both shared co-first authorship.
Rights and permissions
About this article
Cite this article
Kreis, M.E., Ruppert, R., Ptok, H. et al. Use of Preoperative Magnetic Resonance Imaging to Select Patients with Rectal Cancer for Neoadjuvant Chemoradiation—Interim Analysis of the German OCUM Trial (NCT01325649). J Gastrointest Surg 20, 25–33 (2016). https://doi.org/10.1007/s11605-015-3011-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-3011-0