Abstract
Introduction
Variability in surgical and pathological techniques in Western centers may lead to inconsistency in lymph node staging in patients with gastric adenocarcinoma. We hypothesize that ex vivo dissection (EVD) after gastrectomy for adenocarcinoma increases lymph node yield.
Methods
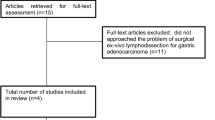
We retrospectively reviewed 222 consecutive patients who underwent gastrectomy with curative intent for adenocarcinoma between November 2010 and June 2014. In August of 2012, we began performing EVD of nodes in surgical specimens (EVD group, N = 111), as opposed to submitting specimens en bloc with lymph node basins attached to the specimen (No EVD group, N = 111). Primary end point was lymph node yield.
Results
The median number of lymph nodes procured was significantly higher in the EVD compared to that in the No EVD group (30 vs. 21 lymph nodes, respectively; P < 0.0001). Moreover, 28 % of the No EVD group were not adequately staged (defined by ≤15 nodes), compared to 5 % of the EVD group (P < 0.0001). Stage-for-stage overall survival was not significantly different.
Conclusion
EVD may be a useful tool to maximize lymph node yield. However, this had no impact on staging or survival. This is an interesting finding that warrants further investigation.



Similar content being viewed by others
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin 2011;61:69–90.
Pisters PWT, Kelsen DP, Tepper JE. Cancer of the Stomach. In: DeVita Jr VT, Lawrence TS, Rosenberg SA., editors. Cancer: Principles & Practice of Oncology. Philadelphia: Lippincott Williams & Wilkins; 2008. pp. 1043–1078.
D’Angelica M, Gonen M, Brennan MF, Turnbull AD, Bains M, Karpeh MS. Patterns of initial recurrence in completely resected gastric adenocarcinoma. Ann Surg 2004;240:808–816.
Paoletti X, Oba K, Burzykowski T, Michiels S, Ohashi Y, Pignon JP, Rougier P, Sakamoto J, Sargent D, Sasako M, et al. Benefit of adjuvant chemotherapy for resectable gastric cancer: a meta-analysis. JAMA 2010;303:1729–1737.
Wang J, Dang P, Raut CP, Pandalai PK, Maduekwe UN, Rattner DW, Lauwers GY, Yoon SS. Comparison of a lymph node ratio-based staging system with the 7th AJCC system for gastric cancer: analysis of 18,043 patients from the SEER database. Ann Surg 2012;255:478–485.
Nitti D, Marchet A, Olivieri M, Ambrosi A, Mencarelli R, Belluco C, et al. Ratio between metastatic and examined lymph nodes is an independent prognostic factor after D2 resection for gastric cancer: analysis of a large European monoinstitutional experience. Ann Surg Oncol 2003;10:1077–1085.
AJCC cancer staging manual. 7th edition ed. New York:Springer; 2010.
Degiuli M, Sasako M, Ponti A; Italian Gastric Cancer Study Group. Morbidity and mortality in the Italian Gastric Cancer Study Group randomized clinical trial of D1 versus D2 resection for gastric cancer. Br J Surg 2010;97:643–649.
Schmidt B, Chang KK, Maduekwe UN, Look-Hong N, Rattner DW, Lauwers GY, Mullen JT, Yang HK, Yoon SS. D2 lymphadenectomy with surgical ex vivo dissection into node stations for gastric adenocarcinoma can be performed safely in Western patients and ensures optimal staging. Ann Surg Oncol 2013;20:2991–2999.
Bouvier AM, Haas O, Pirad F, Roignot P, Bonithon-Kopp C, Faivre J. How many nodes must be examined to accurately stage gastric carcinomas? Results from a population based study. Cancer 2002;94:2862–6.
Smith DD, Schwarz RR, Schwarz RE. Impact of total lymph node count on staging and survival after gastrectomy for gastric cancer: data from a large US-population database. J Clin Oncol 2005;23:7114–7124.
Son T, Hyung WJ, Lee JH, Kim YM, Kim HI, An JY, Cheong JH, Noh SH. Clinical implication of an insufficient number of examined lymph nodes after curative resection for gastric cancer. Cancer 2012;118:4687–4693.
Candela FC, Urmacher C, Brennan MF. Comparison of the conventional method of lymph node staging with a comprehensive fat-clearing method for gastric adenocarcinoma. Cancer 1990;66:1828–1832.
Hanna GB, Amygdalos I, Ni M, Boshier PR, Mikhail S, Lloyd J, Goldin R. Improving the standard of lymph node retrieval after gastric cancer surgery. Histopathology 2013;63:316–324.
Lavy R, Hershkovitz Y, Kapiev A, et al. A comparative study on two different pathological methods to retrieve lymph nodes following gastrectomy. Int J Surg 2014;12:725–728.
Schoenleber SJ, Schnelldorfer T, Wood CM, Qin R, Sarr MG, Donohue JH. Factors influencing lymph node recovery from the operative specimen after gastrectomy for gastric adenocarcinoma. J Gastrointest Surg 2009;13:1233–1237.
Cichowitz A, Burton P, Brown W, Smith A, Shaw K, Slamowicz R, Nottle PD. Ex vivo dissection increases lymph node yield in oesophagogastric cancer. ANZ J Surg 2015;85:80–84.
Nathan H, Shore AD, Anders RA, Wick EC, Gearhart SL, Pawlik TM. Variation in lymph node assessment after colon cancer resection: patient, surgeon, pathologist, or hospital? J Gastrointest Surg 2011;15:471–479.
Valsecchi ME, Leighton J Jr, Trester W. Modifiable factors that influence colon cancer lymph node sampling and examination. Clin Colorectal Cancer 2010;9:162–167.
Noda N, Sasko M, Tamaguchi N, Nakanishi Y. Ignoring small lymph nodes can be a major cause of staging error in gastric cancer. Br J Surg 1998;85:831–834.
Lee HK, Yang HK, Kim WH, Lee KU, Choe KJ, Kim JP. Influence of the number of lymph nodes examined on staging of gastric cancer. Br J Surg 2001;88:1408–1412.
Karpeh MS, Leon L, Klimstra D, Brennan MF. Lymph node staging in gastric cancer: is location more important than number? An analysis of 1,038 patients. Ann Surg 2000;232:362–371.
Altorki NK, Zhou XK, Stiles B, Port JL, Paul S, Lee PC, Mazumdar M. Total number of resected lymph nodes predicts survival in esophageal cancer. Ann Surg 2008;248:221–226.
Acknowledgments
We would like to personally thank Dr. Murray Brennan for his careful review of our manuscript. We would also like to thank Marianne Beninati for her help with data collection.
Author contributions
CA: Participated in research design, performance of the research, data analysis, and writing of the paper.
AL: Participated in research design, performance of the research, data analysis, and writing of the paper.
LS: Participated in research design and critical revision of the paper, and approving the final version of manuscript.
GK: Participated in research design and critical revision of the paper, and approving final version of manuscript.
SSY: Participated in research design and critical revision of the paper, and approving final version of manuscript.
LT: Participated in research design and critical revision of the paper, and approving final version of manuscript.
DC: Participated in research design and critical revision of the paper, and approving final version of manuscript.
VES: Participated in research design, data analysis and critical revision of the paper, and approving final version of manuscript.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Primary Discussant
John T. Mullen, MD (Boston, MA): Thank you Dr. Afaneh for your excellent presentation. As you know, over the years there has been much debate as to the proper extent of lymph node dissection for patients with gastric cancer, and there has been much published about the frequent problem of understaging in the West owing to low numbers of examined lymph nodes, including many proposals for new staging systems (e.g., using lymph node ratios, log odds of metastatic lymph nodes, etc.) designed to compensate for these low nodal yields. You and your co-authors are to be congratulated for adopting a technique known to significantly improve lymph node yields which has long been employed in Asia and has also been employed at my institution over the past several years—ex-vivo dissection (EVD). Surprisingly, though you demonstrated much higher lymph node yields with EVD than without EVD, there were no differences in either the stage-specific stratification of the patients or in overall survival. I have two questions for you:
1. The first and most obvious question is how can you explain the fact that examining 12 more lymph nodes in the EVD group than in the non-EVD group led to absolutely zero difference in nodal staging? The percentages of patients in each of the N groupings (i.e., N0, N1, etc.) are virtually identical (there isn’t even a trend!), and the P value is 1.0.
2. In light of your findings, will you and your colleagues continue to take the extra time to do ex vivo dissections as you currently do on patients with gastric cancer, will you modify the procedure in some way to achieve even higher nodal yields (e.g., dissect out individual lymph nodes as opposed to entire packets), or will you abandon it altogether?
Closing Discussant
Dr. Afaneh:
1. Dr. Mullen, thank you taking the time to carefully review our manuscript. I think you raise an important question. I believe the reason we found no difference in nodal staging is twofold. First, at baseline, we are performing an extended lymphadenectomy (D2). The additive effect of ex vivo dissection may be less substantial in these patients. The number of patients undergoing a D1 lymphadenectomy was small and therefore we are unable to make any conclusions in those patients. In hospitals where the median lymph node yield is often below 8–10 nodes, the effect may be more demonstrable. Second, our follow-up is relatively short. The current study has a follow-up period of less than 3 years; therefore, it may be difficult to assess any impact on stage distribution or even survival. The true staging of those patients with inadequate nodal dissection will never really be known.
2. This is an important question given the negative finding of our study. It may be premature to fully abandon this technique as our colleagues in the East have clearly demonstrated a benefit of ex vivo dissection. Reviewing the data at 3 years would be necessary to assess any impact on survival. Other techniques we are currently considering include submitting the lymph node stations as they are removed in vivo as separate nodal stations or having the pathologists take additional slides of the packets submitted.
Rights and permissions
About this article
Cite this article
Afaneh, C., Levy, A., Selby, L. et al. Ex Vivo Lymphadenectomy During Gastrectomy for Adenocarcinoma Optimizes Lymph Node Yield. J Gastrointest Surg 20, 165–171 (2016). https://doi.org/10.1007/s11605-015-2948-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-2948-3