Abstract
Background
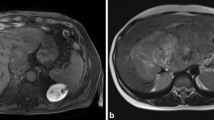
Complete caudate lobectomy using the anterior hepatic parenchymal transection approach is a proper but technically demanding operation for tumors situated in or involving the paracaval portion of the caudate lobe. This study was intended to share our experience on this operation.
Method
Forty-nine consecutive patients who received complete caudate lobectomy using the anterior hepatic parenchymal transection approach were studied. The clinicopathologic and perioperative data, complications, and survival were analyzed.
Results
Of the 49 patients, 15 (30.6 %) received isolated complete caudate lobectomy and 34 (69.4 %) received complete caudate lobectomy associated with segmentectomy IV. The median tumor size was 7.3 cm (2.4–18.0 cm), the operating time was 200 min (120–370 min), and the operative blood loss was 700 ml (200–3000 ml). The postoperative complication rate was 36.7 %. There was no perioperative death. Patients in the associated complete caudate lobectomy group had larger tumors (P < 0.001), higher platelet counts (P = 0.033), shorter operation time (P = 0.004), and less patients with residual tumor (P = 0.03) than those in the isolated complete caudate lobectomy group. There were no significant differences in cirrhosis, surgical resection margin, blood loss, postoperative complications, and prognosis between the two groups.
Conclusion
Complete caudate lobectomy using the anterior hepatic parenchymal transection approach was technically feasible and safe for patients with tumors situated in or involving the paracaval portion of the caudate lobe. Associated resection of segment IV can be used to facilitate the surgery and decrease the chance of local residual tumor.



Similar content being viewed by others
References
Hawkins WG, DeMatteo RP, Cohen MS, Jarnagin WR, Fong Y, D’Angelica M, et al. Caudate hepatectomy for cancer: a single institution experience with 150 patients. J Am Coll Surg. 2005;200:345–52.
Hu JX, Miao XY, Zhong DW, Dai WD, Liu W. Anterior approach for complete isolated caudate lobectomy. Hepatogastroenterology. 2005;52:1641–4.
Yang JH, Gu J, Dong P, Chen L, Wu WG, Mu JS, et al. Isolated complete caudate lobectomy for hepatic tumor of the anterior transhepatic approach: surgical approaches and perioperative outcomes. World J Surg Oncol. 2013;11:197.
Yamamoto J, Kosuge T, Shimada K, Yamasaki S, Takayama T, Makuuchi M. Anterior transhepatic approach for isolated resection of the caudate lobe of the liver. World J Surg. 1999;23:97–101.
Sasada A, Ataka K, Tsuchiya K, Yamagishi H, Maeda H, Okada M. Complete caudate lobectomy: its definition, indications, and surgical approaches. HPB Surg. 1998;11:87–93; discussion -5.
Asahara T, Dohi K, Hino H, Nakahara H, Katayama K, Itamoto T, et al. Isolated caudate lobectomy by anterior approach for hepatocellular carcinoma originating in the paracaval portion of the caudate lobe. J Hepatobiliary Pancreat Surg. 1998;5:416–21.
Ishii H, Ogino S, Ikemoto K, Toma A, Nakamura K, Itoh T, et al. Mesohepatectomy with total caudate lobectomy of the liver for hepatocellular carcinoma. World J Surg Oncol. 2013;11:82.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-13.
Yang Y, Lai EC, Fu SY, Gu FM, Li PP, Lau WY, et al. A prospective randomized controlled trial to compare two methods of selective hepatic vascular exclusion in partial hepatectomy. Eur J Surg Oncol. 2012;39:125–30.
Fu SY, Lai EC, Li AJ, Pan ZY, Yang Y, Sun YM, et al. Liver resection with selective hepatic vascular exclusion: a cohort study. Ann Surg. 2009;249:624–7.
Chaib E, Ribeiro MA, Jr., Silva Fde S, Saad WA, Cecconello I. Caudate lobectomy: tumor location, topographic classification, and technique using right- and left-sided approaches to the liver. Am J Surg. 2008;196:245–51.
Peng SY, Li JT, Mou YP, Liu YB, Wu YL, Fang HQ, et al. Different approaches to caudate lobectomy with “curettage and aspiration” technique using a special instrument PMOD: a report of 76 cases. World J Gastroenterol. 2003;9:2169–73.
Wang Y, Zhang LY, Yuan L, Sun FY, Wei TG. Isolated caudate lobe resection for hepatic tumor: surgical approaches and perioperative outcomes. Am J Surg. 2010;200:346–51.
Liu P, Qiu BA, Bai G, Bai HW, Xia NX, Yang YX, et al. Choice of approach for hepatectomy for hepatocellular carcinoma located in the caudate lobe: isolated or combined lobectomy? World J Gastroenterol. 2012;18:3904–9.
Abdel Wahab M, Lawal AR, E ELH, Salah T, Hamdy E, Sultan AM. Caudate lobe resection: an Egyptian center experience. Langenbecks Arch Surg. 2009;394:1057–63.
Sakamoto Y, Nara S, Hata S, Yamamoto Y, Esaki M, Shimada K, et al. Prognosis of patients undergoing hepatectomy for solitary hepatocellular carcinoma originating in the caudate lobe. Surgery. 2011;150:959–67.
Thomas RL, Lordan JT, Devalia K, Quiney N, Fawcett W, Worthington TR, et al. Liver resection for colorectal cancer metastases involving the caudate lobe. Br J Surg. 2011;98:1476–82.
Khan AZ, Wong VK, Malik HZ, Stiff GM, Prasad KR, Lodge JP, et al. The impact of caudate lobe involvement after hepatic resection for colorectal metastases. Eur J Surg Oncol. 2009;35:510–4.
Takayama T, Makuuchi M, Watanabe K, Kosuge T, Takayasu K, Yamazaki S, et al. A new method for mapping hepatic subsegment: counterstaining identification technique. Surgery. 1991;109:226–9.
Funding
This study was funded by the following: The State Key Infection Diseases Project of China: 2012ZX10002010, 2012ZX10002016; the Science Fund for Creative Research Groups, NSFC, China: 81221061; the National Natural Science Foundation of China: 81372207, 81472285, 81402269, 31201025; and the initiating fund for younger from the Secondary Military Medical University: 2012QN19.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, ZG., Lau, W., Fu, SY. et al. Anterior Hepatic Parenchymal Transection for Complete Caudate Lobectomy to Treat Liver Cancer Situated in or Involving the Paracaval Portion of the Caudate Lobe. J Gastrointest Surg 19, 880–886 (2015). https://doi.org/10.1007/s11605-015-2793-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-2793-4