Abstract
Objective
The objective of this study was to explore volume–outcome associations after major hepatectomy for hepatocellular carcinoma (HCC).
Methods
This population-based cohort study retrospectively analyzed 23,107 major hepatectomies for HCC patients from 1998 to 2009. Relationships between hospital/surgeon volume and patient outcome were analyzed by propensity score matching (PSM). Five-year overall survival (OS) was estimated by Kaplan–Meier method, and differences were compared by log-rank test.
Results
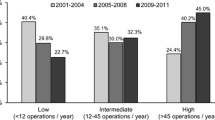
The mean length of stay (LOS) after major hepatectomy was 18.1 days, and the mean hospital cost was US$5,088.2. After PSM, the mean OS in high- and low-volume hospitals was 71.1 months (standard deviation (SD) 0.7 months) and 68.6 months (SD 0.6 months), respectively; the mean OS in high- and low-volume surgeons was 78.5 months (SD 0.7 months) and 66.9 months (SD 0.7 months), respectively. The PSM analysis showed that treatment by high-volume hospitals and treatment by high-volume surgeons were both associated with significantly shorter LOS, lower hospital cost, and longer survival compared to their low-volume counterparts (P < 0.001).
Conclusions
The results of this nationwide study support the regionalization of HCC treatment by hospital volume and by surgeon volume. High surgeon volume revealed both short- and long-term benefits. The applicability of PSM in volume–outcome analysis may also be confirmed.



Similar content being viewed by others
References
Richardson AJ, Pang TC, Johnston E, Hollands MJ, Lam VW, Pleass HC. The volume effect in liver surgery—a systematic review and meta-analysis. J Gastrointest Surg 2013;17(11):1984-1996.
Hyder O, Sachs T, Ejaz A, Spolverato G, Pawlik TM. Impact of hospital teaching status on length of stay and mortality among patients undergoing complex hepatopancreaticobiliary surgery in the USA. J Gastrointest Surg 2013;17(12):2114-2122.
Shi HY, Lee KT, Wang JJ, Sun DP, Lee HH, Chiu CC. Artificial neural network model for predicting 5-year mortality after surgery for hepatocellular carcinoma: a nationwide study. J Gastrointest Surg 2012;16:2126-2131.
Shi HY, Lee KT, Lee HH, Ho WH, Sun DP, Wang JJ, Chiu CC. Comparison of artificial neural network and logistic regression models for predicting in-hospital mortality after primary liver cancer surgery. PLoS One 2012;7:e35781.
Farges O, Goutte N, Bendersky N, Falissard B; ACHBT-French Hepatectomy Study Group. Incidence and risks of liver resection: an all-inclusive French nationwide study. Ann Surg 2012;256(5):697-704.
Shetty GS, You YK, Choi HJ, Na GH, Hong TH, Kim DG. Extending the limitations of liver surgery: outcomes of initial human experience in a high-volume center performing single-port laparoscopic liver resection for hepatocellular carcinoma. Surg Endosc 2012;26:1602-1608.
Tschuor Ch, Croome KP, Sergeant G, Cano V, Schadde E, Ardiles V, Slankamenac K, Clariá RS, de Santibaňes E, Hernandez-Alejandro R, Clavien PA. Salvage parenchymal liver transection for patients with insufficient volume increase after portal vein occlusion – an extension of the ALPPS approach. Eur J Surg Oncol 2013;39(11):1230-1235.
McKay A, You I, Bigam D, Lafreniere R, Sutherland F, Ghali W, Dixon E. Impact of surgeon training on outcomes after resective hepatic surgery. Ann Surg Oncol 2008;15:1348-1355.
Ramacciato G, D'Angelo F, Baldini R, Petrucciani N, Antolino L, Aurello P, Nigri G, Bellagamba R, Pezzoli F, Balesh A, Cucchetti A, Cescon M, Del Gaudio M,Ravaioli M, Pinna AD. Hepatocellular carcinomas and primary liver tumors as predictive factors for postoperative mortality after liver resection: a meta-analysis of more than 35,000 hepatic resections. Am Surg 2012;78:456-467.
Mishra A, Otgonsuren M, Venkatesan C, Afendy M, Erario M, Younossi ZM. The inpatient economic and mortality impact of hepatocellular carcinoma from 2005 to 2009: analysis of the US nationwide inpatient sample. Liver Int 2013;33:1281-1286.
Saxena A, Chua TC, Perera M, Chu F, Morris DL. Surgical resection of hepatic metastases from neuroendocrine neoplasms: a systematic review. Surg Oncol 2012;21(3):e131-141.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992;45:613-619.
Sudan R, Bennett KM, Jacobs DO, Sudan DL. Multifactorial analysis of the learning curve for robot-assisted laparoscopic biliopancreatic diversion with duodenal switch. Ann Surg 2012;255(5):940-945.
Joffe MM, Rosenbaum PR. Invited commentary: propensity scores. Am J Epidemiol 1999;150:327-333.
Shaheen NJ, Kim HP, Bulsiewicz WJ, Lyday WD, Triadafilopoulos G, Wolfsen HC, Komanduri S, Chmielewski GW, Ertan A, Corbett FS, Camara DS, Rothstein RI, Overholt BF. Prior fundoplication does not improve safety or efficacy outcomes of radiofrequency ablation: results from the U.S. RFA Registry. J Gastrointest Surg 2013;17(1):21-28.
Lorenzo CS, Limm WM, Lurie F, Wong LL. Factors affecting outcome in liver resection. HPB 2005;7:226-230.
Lutjens LR. Determinants of hospital length of stay. J Nurs Adm 1993;23:14-18.
Rosenthal GE, Harper DL, Quinn LM, Cooper GS. Severity-adjusted mortality and length of stay in teaching and nonteaching hospitals. Results of a regional study. JAMA 1997;278:485-490.
Fortney JC, Booth BM, Smith GR. Variation among VA hospitals in length of stay for treatment of depression. Psychiatr Serv 1996;47:608-613.
Hsia CY, Chau GY, King KL, Loong CC, Lui WY, Wu CW. Factors for prolonged length of stay after elective hepatectomy for hepatocellular carcinoma. The surgeon's role in the managed care era. Hepatogastroenterology 2003;50:798-804.
Kim WR, Gores GJ, Benson JT, Therneau TM, Melton LJ 3rd. Mortality and hospital utilization for hepatocellular carcinoma in the United States. Gastroenterology 2005;129:486-493.
Lin HC, Tung YC, Chen CC, Tang CH. Relationships between length of stay and hospital characteristics under the case-payment system in Taiwan: using data for vaginal delivery patients. Chang Gung Med J 2003;26:259-268.
Chiu HC, Lee LJ, Hsieh HM, Mau LW. Inappropriate hospital utilization for long-stay patients in southern Taiwan. Kaohsiung J Med Sci 2003;19:225-232.
Chuang KY, Wu SC, Dai YT, Ma AH. Post-hospital care of stroke patients in Taipei: use of services and policy implications. Health Policy 2007;82:28-36.
Lee SD. Exploring policy and financing options for long term care in Taiwan. J Aging Soc Policy 2001;13:203-216.
Lee HC, Chang KC, Lan CF, Hong CT, Huang YC, Chang ML. Factors associated with prolonged hospital stay for acute stroke in Taiwan. Acta Neurol Taiwan 2008;17:17-25.
Hsieh CI, Chung KP, Yang MC, Li TC. Association of treatment and outcomes of doctor-shopping behavior in patients with hepatocellular carcinoma. Patient Prefer Adherence 2013;7:693-701.
Wang MJ, Lin SP. Study on doctor shopping behavior: insight from patients with upper respiratory tract infection in Taiwan. Health Policy 2010;94:61-67.
Cheng SH, Song HY. Physician performance information and consumer choice: a survey of subjects with the freedom to choose between doctors. Qual Saf Health Care 2004;13:98-101.
Robinson JC, Luft HS, McPhee SJ, Hunt SS. Hospital competition and surgical length of stay. JAMA 1988;259:696-700.
Chowdhury MM, Dagash H, Pierro A. A systematic review of the impact of volume of surgery and specialization on patient outcome. Br J Surg 2007;94:145-161.
Livingston EH, Cao J. Procedure volume as a predictor of surgical outcomes. JAMA 2010;304:95-97.
Tol JA, van Gulik TM, Busch OR, Gouma DJ. Centralization of highly complex low-volume procedures in upper gastrointestinal surgery. A summary of systematic reviews and meta-analyses. Dig Surg 2012;29:374-383.
Derogar M, Sadr-Azodi O, Johar A, Lagergren P, Lagergren J. Hospital and surgeon volume in relation to survival after esophageal cancer surgery in a population-based study. J Clin Oncol 2013;31:551-557.
Boudourakis LD, Wang TS, Roman SA, Desai R, Sosa JA. Evolution of the surgeon-volume, patient-outcome relationship. Ann Surg 2009;250:159-165.
Nathan H, Cameron JL, Choti MA, Schulick RD, Pawlik TM. The volume-outcomes effect in hepato-pancreato-biliary surgery: hospital versus surgeon contributions and specificity of the relationship. J Am Coll Surg 2009;208:528-538.
Acknowledgement
This work was supported in part by the Chi Mei Medical Center and Kaohsiung Medical University Cooperation Program, Taiwan, R.O.C., under Grant Numbers 102CM-KMU-01.
Conflict of interest
The authors have no conflicts of interest in the publication of this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Chih-Cheng Lu and Chong-Chi Chiu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Lu, CC., Chiu, CC., Wang, JJ. et al. Volume–Outcome Associations after Major Hepatectomy for Hepatocellular Carcinoma: a Nationwide Taiwan Study. J Gastrointest Surg 18, 1138–1145 (2014). https://doi.org/10.1007/s11605-014-2513-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2513-5