Abstract
Objective
The long-term morphological changes induced by a single episode of alcoholic pancreatitis are not known. Our aim was to study these morphological changes in secretin-stimulated magnetic resonance cholangiopancreatography (S-MRCP) after the first episode of alcohol-associated acute pancreatitis and to evaluate the risk factors and possible protective factors potentially associated with later chronic findings. We have previously reported 2-year follow-up results in pancreatic morphology. This study extends the follow-up to 9 years.
Patients and Methods
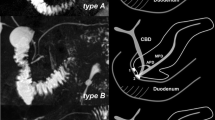
In this prospective follow-up study, S-MRCP imaging was performed for 44 (41 M, 3 F; mean age, 46 (25–68) years) patients after their first episode of alcohol-associated pancreatitis. Pancreatic morphology was evaluated at 3 months and at 2, 7, and 9 years after hospitalization. Recurrent attacks of pancreatitis were studied and pancreatic function was monitored by laboratory tests. Patients’ alcohol consumption was evaluated with questionnaires, laboratory markers, and self-estimated alcohol consumption via interview. Smoking and body mass index were annually recorded.
Results
At 3 months, 32 % of the patients had normal findings in S-MRCP, 52 % had acute, and 16 % had chronic changes. At 7 years, S-MRCP was performed on 36 patients with normal findings in 53 %, the rest (47 %) having chronic findings. Pancreatic cyst was present in 36 %, parenchymal changes in 28 %, and atrophy in 28 % of the cases. There were no new changes in the pancreas in the attending patients between 7 and 9 years (18 patients). Of the patients with only acute findings at 3 months, 60 % resolved to normal in 7 years, but the rest (40 %) showed chronic changes later on. The initial attack was mild in 65 %, moderate in 25 %, and severe in 10 % of the patients. Patients with mild first attack had fewer chronic changes at 7 years compared to patients with moderate or moderate and severe together (p = 0.03, p = 0.01). Of the patients in the seventh year of S-MRCP, 22 % had suffered a recurrent episode of acute pancreatitis (mean, 22 (2–60) months) and 11 % had a clinical diagnosis of chronic pancreatitis. At 7 years, 88 % of the patients with recurrences had chronic findings in S-MRCP versus 36 % with nonrecurrent pancreatitis (p = 0.02). Six (17 %) patients abstained from alcohol throughout follow-up (mean, 8.7 (7–9.1) years), but even one of these developed pancreatic atrophy. Out of the non-abstinent patients who did not suffer recurrences, 4/22 (18 %) had developed new findings during at follow-up S-MRCP (NS). In univariate analysis, heavy smoking showed no correlation with increased chronic changes compared to nonsmoking.
Conclusions
Morphological pancreatic changes increase with recurrent episodes of acute pancreatitis. Patients with mild first attack have fewer chronic changes in the pancreas in the long term. However, even a single episode of acute alcoholic pancreatitis may induce chronic morphological changes in long-term follow-up.

Similar content being viewed by others
References
Apte MV, Pirola RC, Wilson JS. Mechanisms of alcoholic pancreatitis. Journal of Gastroenterology & Hepatology 2010;25:1816–26.
Lankisch PG, Breuer N, Bruns A, Weber-Dany B, Lowenfels AB, Maisonneuve P. Natural history of acute pancreatitis: a long-term population-based study. Am J Gastroenterol 2009;104:2797–805.
Yadav D, O’Connell M, Papachristou GI. Natural history following the first attack of acute pancreatitis. Am J Gastroenterol 2012;107:1096–103.
Yadav D, Lowenfels AB: Trends in the epidemiology of the first attack of acute pancreatitis: a systematic review. Pancreas 2006;33:323–30.
Lankisch PG, Assmus C, Maisonneuve P, Lowenfels AB. Epidemiology of pancreatic diseases in Lüneburg County. Pancreatology 2002;2:469–77.
Kristiansen L, Gronbaek M, Becker U, Tolstrup JS. Risk of pancreatitis according to alcohol drinking habits: a population based cohort study. Am J Epidemiol 2008;168:932–7.
Irving HM, Samokhvalov AV, Rehm J. Alcohol as a risk factor for pancreatitis. A systematic review and meta-analysis. JOP 2009;10:387–92.
Frossard JL, Steer ML, Pastor CM. Acute pancreatitis. Lancet 2008;371:143–52.
Pelli H, Sand J, Laippala P, Nordback I. Long-term follow-up after the first episode of acute alcoholic pancreatitis: time course and risk factors for recurrence. Scand J Gastroenterol 2000;35:552–5.
Pelli H, Lappalainen-Lehto R, Piironen A, Sand J, Nordback I. Risk factors for recurrent acute alcohol-associated pancreatitis: a prospective analysis. Scand J Gastroenterol 2008;43:614–21.
Takeyama Y. Long-term prognosis of acute pancreatitis in Japan. Clin Gastroenterol Hepatol 2009;7:15–7.
Nikkola J, Räty S, Laukkarinen J, Seppänen H, Lappalainen-Lehto R, Järvinen S, Nordback I, Sand J. Abstinence after first acute alcohol-associated pancreatitis protects against recurrent pancreatitis and minimizes the risk of pancreatic dysfunction. Alcohol Alcohol 2013;doi: 10.1093/alcalc/agt019.
Sadr-Azodi O, Andrén-Sandberg Å, Orsini N, Wolk A. Cigarette smoking, smoking cessation and acute pancreatitis: a prospective population-based study. Gut 2012;61:262–7.
Sand J, Nordback I. Acute pancreatitis: risk of recurrence and late consequences of the disease. Nat Rev Gastroenterol Hepatol. 2009;6:470–7.
Braganza JM, Lee Sh, McCloy RF, McMahon MJ. Chronic pancreatitis. Lancet 2011;377:1184–97.
Whitcomb DC, LaRusch J, Krasinskas AM, Klei L, Smith JP, Brand RE, Neoptolemos JP, Lerch MM, Tector M, Sandhu BS, Guda NM, Orlichenko L; Alzheimer’s Disease Genetics Consortium, Alkaade S, Amann ST, Anderson MA, Baillie J, Banks PA, Conwell D, Coté GA, Cotton PB, DiSario J, Farrer LA, Forsmark CE, Johnstone M, Gardner TB, Gelrud A, Greenhalf W, Haines JL, Hartman DJ, Hawes RA, Lawrence C, Lewis M, Mayerle J, Mayeux R, Melhem NM, Money ME, Muniraj T, Papachristou GI, Pericak-Vance MA, Romagnuolo J, Schellenberg GD, Sherman S, Simon P, Singh VP, Slivka A, Stolz D, Sutton R, Weiss FU, Wilcox CM, Zarnescu NO, Wisniewski SR, O’Connell MR, Kienholz ML, Roeder K, Barmada MM, Yadav D, Devlin B. Common genetic variants in the CLDN2 and PRSS1-PRSS2 loci alter risk for alcohol-related and sporadic pancreatitis. Nat Genet. 2012;44:1349–54.
Tukiainen E, Kylänpää ML, Kemppainen E, Nevanlinna H, Paju A, Repo H, Stenman UH, Puolakkainen P. Pancreatic secretory trypsin inhibitor (SPINK1) gene mutations in patients with acute pancreatitis. Pancreas 2005;30:239–42.
Pelli H, Lappalainen-Lehto R, Piironen A, Järvinen S, Sand J, Nordback I. Pancreatic damage after the first episode of acute alcoholic pancreatitis and its association with the later recurrence rate. Pancreatology 2009;9:245–51.
Nordback I, Pelli H, Lappalainen-Lehto R, Järvinen S, Räty S, Sand J. The recurrence of acute alcohol-associated pancreatitis can be reduced: a randomized controlled trial. Gastroenterology 2009;136:848–55.
Nordback I, Sand J, Andrén-Sandberg Å. Criteria for alcoholic pancreatitis—results of an international workshop in Tampere, Finland, June 2006. Pancreatology 2007;7:100–4.
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus. Gut 2013;62:102–11.
Lankisch PG, Weber-Dany B, Maisonneuve P, Lowenfels AB. Pancreatic pseudocysts: prognostic factors for their development and their spontaneous resolution in the setting of acute pancreatitis. Pancreatology 2012;12:85–90.
Balci NC. MRI assessment of chronic pancreatitis. Diagn Interv Radiol 2011;17:249–54.
Mariani A, Arcidiacono PG, Curioni S, Giussani A, Testoni PA. Diagnostic yield of ERCP and secretin-enhanced MRCP and EUS in patients with acute recurrent pancreatitis of unknown aetiology. Digestive and Liver Disease 2009;41:753–8.
Thevenot A, Bournet B, Otal P, Canevet G, Moreau J, Buscail L. Endoscopic ultrasound and magnetic resonance cholangiopancreatography in patients with idiopathic acute pancreatitis. Dig Dis Sci 2013;doi:10.1007/s10620-013-2632-y.
Czakó L. Diagnosis of early-stage chronic pancreatitis by secretin-enhanced magnetic resonance cholangiopancreatography. J Gastroenterol 2007;42:113–7.
Testoni PA, Mariani A, Curioni A, Giussani A, Masci E. Pancreatic ductal abnormalities documented by secretin-enhanced MRCP in asymptomatic subjects with chronic pancreatic hyperenzymemia. Am J Gastroenterol 2009;104:1780–6.
Choueiri NA, Balci NC, Alkaade S, Burton FR. Advanced imaging of chronic pancreatitis. Curr Gastroenterol Rep 2010;12:114–20.
Appelros S, Borgstrom A. Incidence, aetiology and mortality rate of acute pancreatitis over 10 years in a defined urban population in Sweden. Br J Surg 1999;86:465–70.
Gislason H, Horn A, Hoem D, Andrén-Sandberg Å, Imsland AK, Søreide O, Viste A. Acute pancreatitis in Bergen, Norway. A study on incidence, etiology and severity. Scandinavian Journal of Surgery 2004;93:29–33.
Lund H, Tonnesen H, Tonnesen MH, Olsen O. Long-term recurrence and death rates after acute pancreatitis. Scand J Gastroenterol 2006;41:234–8.
Gullo L, Migliori M, Oláh A, Farkas G, Levy P, Arvanitakis C, Lankisch P, Beger H. Acute pancreatitis in five European countries: etiology and mortality. Pancreas 2002;24:223–7.
Gullo L, Migliori M, Pezzilli R, Oláh A, Farkas G, Levy P, Arvanitakis C, Lankisch P, Beger H. An update on recurrent acute pancreatitis: data from five European countries. Am J Gastroenterol 2002;97:1959–62.
Bradley EL III. A clinically based classification system for acute pancreatitis. Summary of the International Symposium on Acute Pancreatitis, Atlanta, GA, September 11 through 13, 1992. Arch Surg 1993;128:586–90.
Ammann RW, Muellhaupt B. Progression of alcoholic acute to chronic pancreatitis. Gut 1994;35:552–6.
Nojgaard C, Becker U, Matzen P, Andersen JR, Holst C, Bendtsen F. Progression from acute to chronic pancreatitis. Pancreas 2011;40:1195–200.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussant
Dr. Nicholas Zyromski (Indianapolis, Indiana): Pancreatic morphological changes in a long-term follow-up after first episode of acute alcoholic pancreatitis.
Nikkola, et al.
These Finnish authors provide a strong contribution to our knowledge of acute alcoholic pancreatitis natural history. The major strength of this study lies in the diligent, long-term (9 years!) follow-up of an extremely challenging patient population. The authors found that a primary episode of severe pancreatitis (as opposed to mild or moderate severity) was accompanied by recurrent pancreatitis episodes and pancreatic morphologic changes.
Questions:
1. Did morphologic changes seen on secretin-stimulated MRCP correlate with clinical exocrine and endocrine insufficiency rates?
How does this knowledge influence clinical practice (are you more likely to offer decompression of pseudocyst prior to symptom development)?
Closing Discussant
Dr. Jussi Nikkola: Patients who had normal pancreatic morphology at seven years had not developed chronic pancreatitis in follow-up, while 24 % (4/17) of patients with chronic changes at seven years had developed clinically significant pancreatic exocrine insufficiency (p = 0.04). These patients had all gone through a recurrent episode or episodes of pancreatitis.
Seventen percent (3/18) of patients who had normal morphology at seven years had developed new diabetes. Among patients with chronic findings at seven years 42 % (5/12) had a new diagnose of diabetes during follow-up (NS) (patients with diabetes diagnosed before or during hospitalization excluded). One patient who had chronic pancreatitis didn’t develop diabetes but the rest three did.
Pseudocyst at two years was noted as a risk factor for recurrences as Pelli et al. previously reported. Occurrence of persistent pseudocyst, even asymptomatic, should thus probably favor active drainage. No additional risk factors were found in this study. We managed to report important observations of long-term changes in pancreatic morphology during natural course of acute alcoholic pancreatitis. Main findings were that recurrent episodes are connected to increased pancreatic damage and patients with mild first attack have less chronic changes during follow-up. Attention should be paid to decrease recurrences in alcoholic pancreatitis. Nordback et al. have demonstrated that active interventions with six-months intervals decrease recurrences effectively.
This study has been selected for the following plenary sessions: 21.11.2012 Operatiiviset päivät 2012 (National Surgical Meeting), Helsinki, Finland. 19.5.2013 Digestive Disease Week 2013, Orlando, FL, USA
Rights and permissions
About this article
Cite this article
Nikkola, J., Rinta-Kiikka, I., Räty, S. et al. Pancreatic Morphological Changes in Long-Term Follow-Up after Initial Episode of Acute Alcoholic Pancreatitis. J Gastrointest Surg 18, 164–171 (2014). https://doi.org/10.1007/s11605-013-2279-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-013-2279-1