Abstract
Purpose
The purpose of this study is to determine whether methicillin-resistant Staphylococcus aureus (MRSA) colonization affects surgical site infections (SSI) after major gastrointestinal (GI) operations.
Methods
We retrospectively reviewed the charts of all patients undergoing major GI surgery from December 2007 to August 2009. All patients were tested for MRSA colonization and grouped according to results (MRSA+, methicillin-sensitive S. aureus [MSSA]+, and negative). Data analyzed included demographics, incidence of SSI, and wound culture results.
Results
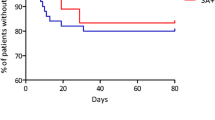
A total of 1,137 patients were identified; 78.9 % negative, 14.7 % MSSA+, and 6.4 % MRSA+. The mean age was 59.5 years, 44.5 % of the patients were men, and 47.9 % of the patients underwent colorectal operation. SSI was identified in 101 (8.9 %) patients and was higher in the MRSA+ group than the negative and MSSA+ groups (13.7 vs. 9.4 vs. 4.2 %; p < 0.05). Although MRSA colonization had an odds ratio of 1.43 for developing an SSI, it was not a significant independent risk factor. However, the MRSA+ group was strongly associated with MRSA cultured from the wound when SSI was present (70 vs. 8.5 %; p < 0.0001).
Conclusions
MRSA colonization is not an independent risk factor for SSI following major GI operations; however, it is strongly predictive of MRSA-associated SSI in these patients. Preoperative MRSA nasal swab test with decolonization may reduce the incidence of MRSA-associated SSI after major GI surgery.
Similar content being viewed by others
References
Engemann JJ, Carmeli Y, Cosgrove SE, Fowler VG, Bronstein MZ, Trivette SL, Briggs JP, Sexton DJ, Kaye KS. Adverse clinical and economic outcomes attributable to methicillin resistance among patients with Staphylococcus aureus surgical site infection. Clin Infect Dis. 2003; 36:592–8.
Anderson DJ, Kaye KS, Chen LF, Schmader KE, Choi Y, Sloane R, Sexton DJ. Clinical and financial outcomes due to methicillin resistant Staphylococcus aureus surgical site infection: a multi-center matched outcomes study. PLoS One. 2009;4:e8305.
Scott RD. The direct medical costs of heathcare-associated infections in U.S. hospitals and the benefits of prevention. Atlanta, GA: Division of Healthcare Quality Promotion National Center for Preparedness, Detection, and Control of Infectious Diseases; Coordinating Center for Infectious Diseases; Centers for Disease Control and Prevention.
Jarvis WR, Jarvis AA, Chinn RY. National prevalence of methicillin-resistant Staphylococcus aureus in inpatients at United States health care facilities, 2010. Am J Infect Control. 2012;40:194–200.
Klevens RM, Morrison MA, Nadle J, Petit S, Gershman K, Ray S, Harrison LH, Lynfield R, Dumyati G, Townes JM, Craig AS, Zell ER, Fosheim GE, McDougal LK, Carey RB, Fridkin SK. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA 2007;298:1763–1771.
Pofahl WE, Goettler CE, Ramsey KM, Cochran MK, Nobles DL, Rotondo MF. Active surveillance screening of MRSA and eradication of the carrier state decreases surgical-site infections caused by MRSA. J Am Coll Surg. 2009;208:981–6.
Price CS, Williams A, Philips G, Dayton M, Smith W, Morgan S. Staphylococcus aureus nasal colonization in preoperative orthopaedic outpatients. Clin Orthop Relat Res. 2008;466:2842–7.
Tom TS, Kruse MW, Reichman RT. Update: Methicillin-resistant Staphylococcus aureus screening and decolonization in cardiac surgery. Ann Thorac Surg. 2009;88:695–702.
Cowie SE, Ma I, Lee SK, Smith RM, Hsiang YN. Nosocomial MRSA infection in vascular surgery patients: impact on patient outcome. Vasc Endovascular Surg. 2005;39:327–34.
Baum SE, Dooley DP. Preventing methicillin-resistant Staphylococcus aureus infection in cardiovascular surgery patients: can we do any better? Clin Infect Dis 2004;38:1561–3.
Davis KA, Stewart JJ, Crouch HK, Florez CE, Hospenthal DR. Methicillin-resistant Staphylococcus aureus (MRSA) nares colonization at hospital admission and its effect on subsequent MRSA infection. Clin Infect Dis. 2004;39:776–82.
Harbarth S, Fankhauser C, Schrenzel J, Christenson J, Gervaz P, Bandiera-Clerc C, Renzi G, Vernaz N, Sax H, Pittet D. Universal screening for methicillin-resistant Staphylococcus aureus at hospital admission and nosocomial infection in surgical patients. JAMA. 2008;299:1149–57.
Trautmann M, Stecher J, Hemmer W, Luz K, Panknin HT. Intranasal mupirocin prophylaxis in elective surgery. A review of published studies. Chemotherapy. 2008; 54:9–16.
Awad SS, Palacio CH, Subramanian A, Byers PA, Abraham P, Lewis DA, Young EJ. Implementation of a methicillin-resistant Staphylococcus aureus (MRSA) prevention bundle results in decreased MRSA surgical site infections. Am J Surg. 2009;198:607–10.
Robicsek A, Beaumont JL, Paule SM, Hacek DM, Thomson RB Jr, Kaul KL, King P, Peterson LR. Universal surveillance for methicillin-resistant Staphylococcus aureus in 3 affiliated hospitals. Ann Intern Med. 2008;148:409–18.
Malde DJ, Hardern L, Welch M. Is it possible to predict outcome in MRSA positive patients undergoing arterial reconstruction? Int Angiol. 2006;25:78–83.
Konishi T, Watanabe T, Kishimoto J, Nagawa H. Elective colon and rectal surgery differ in risk factors for wound infection: results of prospective surveillance. Ann Surg. 2006;244:758–63.
Walz JM, Paterson CA, Seligowski JM, Heard SO. Surgical site infection following bowel surgery: a retrospective analysis of 1446 patients. Arch Surg. 2006;141:1014–8.
Smith RL, Bohl JK, McElearney ST, Friel CM, Barclay MM, Sawyer RG, Foley EF. Wound infection after elective colorectal resection. Ann Surg. 2004;239:599–605.
de Oliveira AC, Ciosak SI, Ferraz EM, Grinbaum RS. Surgical site infection in patients submitted to digestive surgery: risk prediction and the NNIS risk index. Am J Infect Control. 2006;34:201–7.
Parvez N, Jinadatha C, Fader R, Huber TW, Robertson A, Kjar D, Cornelius LK. Universal MRSA nasal surveillance: characterization of outcomes at a tertiary care center and implications for infection control. South Med J. 2010;103:1084–91.
Program Specifics. ACS NSQIP. Available at: http://www.acsnsqip.org/main/aboutacs/about_overview.jsp. Accessed June 12, 2012.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20:250–78.
Mest DR, Wong DH, Shimoda KJ, Mulligan ME, Wilson SE. Nasal colonization with methicillin-resistant Staphylococcus aureus on admission to the surgical intensive care unit increases the risk of infection. Anesth Analg. 1994;78:644–50.
Levy BF, Rosson JW, Blake A. MRSA in patients presenting with femoral fractures. Surgeon. 2004;2:171–2.
Boyce JM, Jackson MM, Pugliese G, Batt MD, Fleming D, Garner JS, Hartstein AI, Kauffman CA, Simmons M, Weinstein R, et al. Methicillin-resistant Staphylococcus aureus (MRSA): a briefing for acute care hospitals and nursing facilities. The AHA Technical Panel on Infections Within Hospitals. Infect Control Hosp Epidemiol. 1994;15:105–15.
Berenguer CM, Ochsner MG, Lord SA, Senkowski CK. Improving surgical site infections: using National Surgical Quality Improvement data to institutie surgical care improvement project protocols in improving surgical outcomes. J Am Coll Surg 2010;210:737–743.
Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol. 1999;20:725–730.
Ammerlaan HS, Kluytmans JA, Wertheim HF, Nouwen JL, Bonten MJ. Eradication of methicillin-resistant Staphylococcus aureus carriage: a systematic review. Clin Infect Dis 2009;48:922–30.
Coates T, Bax R, Coates A. Nasal decolonization of Staphylococcus aureus with mupirocin: strengths, weakness and future prospects. J Antimicrob Chemother 2009;64:9–15.
Grant Support
No financial support was received for this study
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussant
Dr. Mark P. Callery (Boston, MA): Congratulations on providing us this first evaluation of how MRSA colonization impacts surgical site infections (SSIs) after elective gastrointestinal surgery. While case numbers are small and dwarfed compared to the reported infections caused by the usual pathogens of GI surgery, they do reveal that MRSA colonization strongly predicts MRSA-associated SSIs.
Did any of those infections occur in a cluster of any sort, such as across a tight time period, or perhaps related to a certain ward or other healthcare facility?
Going forward, should we alter our prevention and treatment strategies for SSIs in GI surgery based on these data? Beyond higher suspicions for MRSA, should we broaden prophylactic antibiotics, or open wounds sooner? Is uniform surveillance for patients or healthcare personnel for that matter needed, and if so, worth it from a cost standpoint? What if we were more compliant with hand hygiene to retard transmission, would that be enough? How have you changed your own practice?
Closing Discussant
Dr. Harry T. Papaconstantinou: Thank you Dr. Callery for your thoughtful review, comments, and questions. First, we did not identify any clustering of infections in terms of time period, ward, or healthcare provider. In terms of how we move forward given our study and data, I think we need to consider altering how we manage MRSA-colonized patients preoperatively. Although we do not do preoperative testing at our facility, I do review the chart to determine if the patient has had a previous MRSA infection or has had a previous positive nasal swab test. In those patients, I include vancomycin in the perioperative antibiotic prophylaxis and have a lower threshold for opening a wound I suspect is infected. I cannot comment on how this has affected outcomes. I have not reviewed our experience.
Uniform surveillance and isolation for patients with MRSA colonization as been implemented at many institutions including our own. Its success is dependent on minimizing the exposure and patient to patient transmission. Given that many hospital-acquired infections can carry a hefty cost, many studies have shown it is cost-effective. As for surveillance of healthcare personnel, I am not familiar with the data and cannot comment. Hand hygiene, on the other hand, is very important. It also decreases patient to patient transmission and has been shown to decrease hospital-acquired infections. Its success, however, is dependent upon completing the task. Many hospitals that survey hand washing (hand hygiene) report compliance rates much <100 %. I would hope that we, healthcare professionals, can do a better job in this respect.
It is clear that antibiotic-resistant organisms will play a significant role in surgical care. Our study provides knowledge on how MRSA colonization affects SSI following major GI surgery. If nasal colonization of MRSA is a strong predictor of organisms involved in SSI following these operations, we must investigate whether managing (eradicating) nasal colonization will have an impact. In our current healthcare climate, any study like that must include a comprehensive cost–benefit analysis to determine if implementation is cost-effective.
Rights and permissions
About this article
Cite this article
Ramirez, M.C., Marchessault, M., Govednik-Horny, C. et al. The Impact of MRSA Colonization on Surgical Site Infection Following Major Gastrointestinal Surgery. J Gastrointest Surg 17, 144–152 (2013). https://doi.org/10.1007/s11605-012-1995-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-012-1995-2