Abstract
Background
Symptomatic walled-off pancreatic necrosis (WOPN) treated with dual modality endoscopic and percutaneous drainage (DMD) has been shown to decrease length of hospitalization (LOH) and use of radiological resources in comparison to standard percutaneous drainage (SPD).
Aim
The aim of this study is to demonstrate that as the cohort of DMD and SPD patients expand, the original conclusions are durable.
Methods
The database of patients receiving treatment for WOPN between January 2006 and April 2011 was analyzed retrospectively.
Patients
One hundred two patients with symptomatic WOPN who had no previous drainage procedures were evaluated: 49 with DMD and 46 with SPD; 7 were excluded due to a salvage procedure.
Results
Patient characteristics including age, sex, etiology of pancreatitis, and severity of disease based on computed tomographic severity index were indistinguishable between the two cohorts. The DMD cohort had shorter LOH, time until removal of percutaneous drains, fewer CT scans, drain studies, and endoscopic retrograde cholangiopancreatography (ERCPs; p < 0.05 for all). There were 12 identifiable complications during DMD, which were successfully treated without the need for surgery. The 30-day mortality in DMD was 4% (one multi-system organ failure and one out of the hospital with congestive heart failure). Three patients receiving SPD had surgery, and three (7%) died in the hospital.
Conclusion
DMD for symptomatic WOPN reduces LOH, radiological procedures, and number of ERCPs compared to SPD.



Similar content being viewed by others
Notes
Also referred to as combined modality therapy in previous publications by our group.
References
Banks PA, Freeman ML, Practice Parameters Committee of the American College of Gastroenterology. Practice Guidelines in Acute Pancreatitis. Am J Gastroenterol 2006; 101:2379–2400.
Whitcomb DC. Acute Pancreatitis. New Engl J Med 2006; 354;2142–2150.
Baron TH, Morgan De. Acute necrotizing pancreatitis. New Engl J Med 1999; 340:1412–1418.
AGA Institute. Technical review on acute pancreatitis. Gastroenterology 2007;132:2022–2044.
Ashley SW, Perez A, Pierce EA, Brooks DC, Moore FD, Jr., Whang EE, Banks PA, Zinner MJ. Necrotizing pancreatitis. Contemporary analysis of 99 consecutive cases. Ann Surg 2001;234:572–580.
Rau B, Bothe A, Beger HG. Surgical treatment of necrotizing pancreatitis by necrosectomy and closed lavage: changing patient characteristics and outcome in a 19-year, single-center series. Surgery 2005; 138;28–39.
Howard TJ, Patel JB, Zyromski N, Sandrasegaran K, Yu J, Nakeeb A, Pitt HA, Lillemoe DK. Declining morbidity and mortality rates in the surgical management of pancreatic necrosis. J Gastrointest Surg 2007; 11:43–49.
Van Santvoort HC, Besselink MG, Baker OJ, Hofker HS, Boermeester MA, Dejong CH, van Goor H, Schaapherder AF, van Eijck CH, Bollen TL, van Ramshorst B, Nieuwenhuijs VB, Timmer R, Lameris JS, Kruyt PM, Manusama ER, van der Harst E, van der Schelling GP, Karsten T, Hesselink EJ, van Laarhoven CJ, Rosman C, Bosscha K, de Wit RJ, Houdijk AP, van Leeuwen MS, Buskens E, Gooszen HG, Dutch Pancreatitis Study Group. A step-up approach or open necrosectomy for necrotizing pancreatitis. N Engl J Med 2010; 362:1491–502.
Parekh D. Laparoscopic-assisted pancreatic necrosectomy: a new surgical option for treatment of severe necrotizing pancreatitis. Arc Surg 2006; 141-895-903.
Carter CR, McKay CJ, Imrie CW. Percutaneous necrosectomy and sinus tract endoscopy in the management of infected pancreatic necrosis: an initial experience. Ann Surg 2000; 232:175–180.
Ammori BJ. Laparoscopic transgastric pancreatic necrosectomy for infected pancreatic necrosis. Surg Endosc 2002; 16:1362.
Connor S, Ghaneh P, Raraty M, Sutton R, Rosso E, Garvey CJ, Hughes ML, Evans JC, Rowlands P, Neoptolemos JP. Minimally invasive retroperitoneal pancreatic necrosectomy. Dig Surg 2003; 20:270–277.
Horvath K, Freeny P, Escallon J, Heagerty P, Comstock B, Glickerman DJ, Bulger E, Sinanan M, Langdale L, Kolokythas O, Andrews RT. Safety and efficacy of video-assisted retroperitoneal debridement for infected pancreatic collections. A multi-center, prospective, single-arm phase 2 study. Arch Surg 2010;145:817–825.
Freeny PC, Hauptmann E, Althaus SJ, Traverso LW, Sinanan M. Percutaneous CT-guided catheter drainage of infected acute necrotizing pancreatitis: techniques and results. AJR Am J Roentgenol 1998; 170;969–975.
Fotoohi M, Traverso LW. Management of severe pancreatic necrosis. Curr Treat Options Gastroenterol 2007; 10:341–346.
Fotoohi M, Traverso LW. Pancreatic necrosis: paradigm of a multidisciplinary team. Adv Surg 2006; 40:107–118.
Endlicher E, Volk M, Feuerbach S, Scholmerich J, Schuffler A, Messmann H. Long-term follow-up of patients with necrotizing pancreatitis treated by percutaneous necrosectomy. Hepato-Gastroenterol 2003; 50:2225–2228.
VanSonnenberg E, Wittich GR, Chon KS, D’Agostino HB, Casola G, Easter D, Morgan RG, Walser EM, Nealon WH, Goodacre B, Stabile BE. Percutaneous radiologic drainage of pancreatic abscesses. AJR 1997; 168:979–984.
Papachristou GI, Takahashi N, Chahal P, Sarr MG, Baron TD. Peroral endoscopic drainage/debridement of walled-off pancreatic necrosis. Ann Surg 2007; 245:843–951.
Gardner TB, Chahal P, Papachristou GI, Vege SS, Petersen BT, Gostout CJ, Topazian MD, Takahashi N, Sarr MG, Baron TH. A comparison of direct endoscopic necrosectomy with transmural endoscopic drainage for the treatment of walled-off pancreatic necrosis. Gastrointest Endosc 2009; 69:1085–1094.
Gardner TB, Coelho-Prabhu N, Gordon Sr, Gelrud A, Maple JT, Papachristou GI, Freeman ML, Topazian MD, Attam R, Mackenzie TA, Baron TH. Direct endoscopic necrosectomy for the treatment of walled-off pancreatic necrosis; results from a multicenter U.S. series. Gastrointest Endosc 2011; 73:718–726.
Seifert H, Biermer M, Schmitt W, Jurgensen C, Will U, Gerlach R, Kreitmair C, Meining A, Wehrmann T, Rosch T. Transluminal endoscopic necrosectomy after acute pancreatitis: a multicentre study with long-term follow-up (the GEPARD Study). Gut 2009; 58:1260–1266.
Morgan DE, Ragheb CM, Lockhart ME, Cary B, Fineberg NS, Berland LL. Acute pancreatitis: computed tomography utilization and radiation exposure are related to severity but not patient age. Clin Gastroenterol Hepatol 2010; 8:303–308.
Fagenholz PJ, Fernandez-del Castillo C, Harris NS, Pelletier AJ, Camargo CA, Jr. Direct medical costs of acute pancreatitis hospitalizations in the United States. Pancreas 2007; 35:302–307.
Shaheen NJ, Hansen RA, Morgan DR, Gangarosa LM, Ringel Y, Thiny MT, Russo MW, Sandler RS. The burden of gastrointestinal and liver diseases, 2006. Am J Gastroenterol 2006; 101:2128–2138.
Ross A, Gluck M, Irani S, Hauptmann E, Fotoohi M, Siegal J, Robinson D, Crane R, Kozarek R. Combined endoscopic and percutaneous drainage of organized pancreatic necrosis. Gastrointest Endosc 2009; 71:79–84.
Gluck M, Ross A, Irani S, Lin O, Hauptmann E, Siegal J, Fotoohi M, Crane R, Robinson D, Kozarek RA. Endoscopic and percutaneous drainage of symptomatic walled-off pancreatic necrosis reduces hospital stay and radiographic resources. Clin Gastroenterol Hepatol 2010; 8:1083–1088.
Balthazar EJ, Freeny PC, VanSonnenberg E. Imaging and intervention in acute pancreatitis. Radiology 1994; 193:297–306.
Balthazar EJ. Acute pancreatitis: assessment of severity with clinical and CT evaluation. Radiology 2002; 223:603–613.
Beger HG, Buchler M, Bittner R, Oettinger W, Block S, Nevalainen T. Necrosectomy and postoperative local lavage in patients with necrotizing pancreatitis: results of a prospective clinical trial. World J Surg 1988; 12:255–262.
Traverso L W, Kozarek RA. Pancreatic necrosectomy: definitions and technique. J Gastrointest Surg 2005; 9:435–439.
Fernandez-del Castillo C, Rattner DW, Makary MA, Mostafavi A, McGrath D, Warshaw AL. Debridement and closed packing for the treatment of necrotizing pancreatitis. Ann Surg 1998; 228:676–684.
Connor S, Raraty MGT, Neoptolemos JP, Layer P, Runzi M. Does infected pancreatic necrosis require immediate of emergency debridement? Pancreas 2006; 33:128–134.
Fotoohi M, D’Agostino HB, Wollman B, Chon K, Shahrokni S, VanSonnenberg E. Persistent pancreatocutaneous fistula after percutaneous drainage of pancreatic fluid collections: role of cause and severity of pancreatitis. Radiology 1999; 213:373–578.
Mier J, Luque-de Leon E, Castillo A, Robledo F, Blanco R. Early versus late necrosectomy in severe necrotizing pancreatitis. Am j Surg 1997; 173:71–75.
Besselink MGH, Verwer TJ, Schoenmaeckers EJP, Buskens E, Ridwan BU, Visser MR, Nieuwenhuijs VB, Gooszen HG. Timing of surgical intervention of necrotizing pancreatitis. Arch Surg 2007; 142:1194–1201.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussant
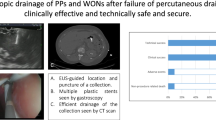
Dr. Todd Baron (Rochester, MN): Use of irrigation in the management of pancreatic necrosis was initially described when specific open necrosectomy approaches were used. Irrigation became vital in the percutaneous approach as established by the Virginia Mason group. The initial series of successful endoscopic drainage of pancreatic necrosis employed aggressive irrigation through a single transmural tract using a nasobiliary tube inserted alongside internally placed stents. Subsequently, some authors reported using irrigation provided through placement of a jejunal extension tube through a PEG tube that was then passed through the transmural site into the collection; this also avoids external fistula.
The present study by Dr. Gluck and colleagues uses less intensive endoscopic and percutaneous approaches than when either is used alone. I believe this dual modality drainage (DMD) therapy could potentially be reproducible and particularly useful in community centers where endoscopic techniques for transmural placement of stents as for pseudocyst drainage and percutaneous techniques as for abscess drainage are now commonly available.
Questions:
1.What was the volume and type of irrigant used in the DMD group?
2.Your patients had primarily central pancreatic necrosis. Can you comment on how many patients had large paracolic gutter extensions (unilateral and bilateral)? These are patients traditionally difficult to treat using endoscopic transmural techniques alone.
3.What was the outcome of those in disconnected ducts in whom transmural stents remained long term? How long did those stents remain in place?
4.Can you comment as to why you think the pseudoaneurysm rate was much lower in the DMD group?
Closing Discussant
Dr. Michael Gluck:
1. What was the volume and type of irrigant used in the DMD group?
We used 20 mL of sterile normal saline, infused three times daily through each percutaneous drain. This was the same quantity and type of fluid as used in the SPD group. As the cavities closed, we decreased the volume until the drains were removed.
2. Your patients had primarily central pancreatic necrosis. Can you comment on how many patients had large paracolic gutter extensions (unilateral and bilateral)? These are patients traditionally difficult to treat using endoscopic transmural techniques alone.
Radiographs of all patients who had SPD and DMD were reviewed to determine if paracolic gutter extension existed on the day of percutaneous drainage. Sixty percent of SPD and 39% of DMD had evidence of left-sided, right-sided, or bilateral extension (p < 0.03). In the SPD group, 16 (35%) had bilateral extension compared to 10 (21%) in the DMD. Only two patients in the SPD cohort had solely right-sided involvement without left-sided as compared to none in the DMD cohort. As Dr. Baron mentioned, those patients with paracolic extension appear to have longer hospitalizations and duration of percutaneous drain tubes in both SPD and DMD. Comparing those with bilateral extension in both cohorts still demonstrates reduced hospital stays and number of radiological studies needed until discharge in the DMD cohort.
3. What was the outcome of those in disconnected ducts in whom transmural stents remained long term? How long did those stents remain in place?
Of the original 15 patients treated with DMD whose therapy was completed almost 3 years ago, 8 had disconnected ducts. Stents spontaneously passed in two. One developed a fluid collection that resolved with placement of a transpapillary stent. After removal of the transpapillary stent, the fluid collection recurred, but the patient is asymptomatic and has not required any new procedures. The other patient has no new fluid collection and is asymptomatic. Two fluid collections recurred in patients who had side branch leaks after transgastric stents were removed due to main branch strictures. Both fluid collections resolved with transpapillary stents, but as in the patients with disconnected ducts, the fluid collections recurred after stent removal. Both patients with new fluid collections remain asymptomatic. In all patients with side branch leaks, transgastric stents were removed at completion of therapy. For those eight with disconnected ducts, six patients have the transgastric stents in position currently without symptoms. We are aware of 1 other patient with a disconnected main pancreatic duct, not in the original cohort of 15, who developed a new symptomatic fluid collection adjacent to the ligament of Treitz 6 months after removal of percutaneous drains. The new collection was drained using endoscopic ultrasound. His previously placed transgastric stents are in position but not contiguous with the new fluid collection.
4. Can you comment as to why you think the pseudoaneurysm rate was much lower in the DMD group?
Although speculative, we think that pseudoaneurysms develop due to direct contact of arteries to the erosive effects of pancreatic secretions, inflammatory debris, and the mechanical trauma of percutaneous tube exchanges. The DMD cohort had fewer drains, fewer drain exchanges, smaller maximal drain size (18 French versus 28 French), and significantly shorter time to resolution of WOPN, decreasing exposure of the retroperitoneal vasculature to pancreatic secretions. The secretions preferentially drained into the stomach or duodenum and away from the WOPN.
Dr. Baron suggested that DMD could conceivably be instituted at community hospitals given that skilled endoscopic ultrasonographers place transgastric stents into pseudocysts and interventional radiologists commonly drain abscesses. In theory and with respect to skill level, we agree with him; however, we have cared for two patients who had DMD undertaken at community hospitals who then developed abscesses requiring further intensive management at our tertiary pancreatic center. Management of WOPN requires a team approach where there are an adequate number of committed interventional radiologists who cover one another, gastroenterologists who manage pancreatic diseases regularly, and surgeons who can and will operate on the pancreas if necessary. Until those teams are assembled, we recommend that management of WOPN be initiated and completed in centers with a substantial volume of patients with severe acute pancreatitis, expertise in minimally invasive techniques to treat WOPN, and a coordinated multidisciplinary approach for those patients.
All authors were involved in the design and analysis of study results and assisted in writing this paper.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
(MPG 13745 kb)
(WMV 14442 kb)
(MPG 26848 kb)
Rights and permissions
About this article
Cite this article
Gluck, M., Ross, A., Irani, S. et al. Dual Modality Drainage for Symptomatic Walled-Off Pancreatic Necrosis Reduces Length of Hospitalization, Radiological Procedures, and Number of Endoscopies Compared to Standard Percutaneous Drainage. J Gastrointest Surg 16, 248–257 (2012). https://doi.org/10.1007/s11605-011-1759-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-011-1759-4