Abstract
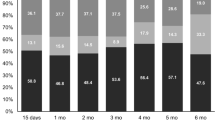
In pancreatic cancer patients, survival and palliation of symptoms should be balanced with social and functional impairment, and for this reason, health-related quality of life measurements could play an important role in the decision-making process. The aim of this work was to evaluate the quality of life and survival in 92 patients with different stages of pancreatic adenocarcinoma who underwent surgical and/or medical interventions. Patients were evaluated with the Functional Assessment of Cancer Therapy questionnaires at diagnosis and follow-up (3 and 6 months). At diagnosis, 28 patients (30.5%) had localized disease (group 1) and underwent surgical resection, 34 (37%) had locally advanced (group 2), and 30 (32.5%) metastatic disease (Group 3). Improvement in quality of life was found in group 1, while in group 3, it decreased at follow-up (p = 0.03). No changes in quality of life in group 2 were found. Chemotherapy/chemoradiation seems not to significantly modify quality of life in groups 2 and 3. Median survival time for the entire cohort was 9.8 months (range, 1–24). One-year survival was 74%, 30%, and 16% for groups 1, 2, and 3 respectively (p = 0.001). Pancreatic cancer prognosis is still dismal. In addition to long-term survival benefits, surgery impacts favorably quality of life.





Similar content being viewed by others
References
Jemal A, Murray T, Ward E, Samuels A, Tiwari RC, Ghafoor A, Feuer EJ, Thun MJ. Cancer Statistics, 2005 CA. Cancer J Clin 2005;55:10–30.
Yeo CJ, Cameron JL, Lillemoe KD, Sohn TA, Campbell KA, Sauter PK, Coleman J, Abrams RA, Hruban RH. Pancreaticoduodenectomy with or without distal gastrectomy and extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma, part 2: randomized controlled trial evaluating survival, morbidity and mortality. Ann Surg 2002;236:355–366.
Ferrone CR, Finkelstein DM, Thayer SP, Muzikansky A, Fernandez-del Castillo C, Warshaw AL. Perioperative CA19-9 levels can predict stage and survival in patients with resectable pancreatic adenocarcinoma. J Clin Oncol 2006;24:2897–2902.
Sener SF, Fremgen A, Menck HR, Winchester DP. Pancreatic caner: a report of treatment and survival trends for 100,313 patients diagnosed from 1985–1995, using the national cancer database. J Am Coll Surg 1999;189:1–7.
Talamonti MS, Small W, Mulcahy MF, Wayne JD, Attaluri V, Coletti LM, Zalupski MM, Hoffman JP, Freedman GM, Kinsella TJ, Philip PA, McGrinn CJ. A multi-institutional phase II trial of preoperative full-dose gemcitabine and concurrent radiation for patients with potentially resectable pancreatic carcinoma. Ann Surg Oncol 2006;13:150–158.
Yip D, Karapetis C, Strickland A, Steer CB, Goldstein D. Chemotherapy and radiotherapy for inoperable advanced pancreatic cancer. Cochrane Database Syst Rev 2006;19:CD00093.
Ko AH, Dito E, Schillinger B, Venook AP, Bergsland EK, Tempero MA. Phase III study of fixed dose rate gemcitabine with cisplatin for metastatic adenocarcinoma of the pancreas. J Clin Oncol 2006;24:379–385.
Lillemoe KD, Pitt HA. Palliation. Surgical and otherwise. Cancer 1996;78:605–614.
Lillemoe KD, Cameron JL, Hardacre JM, Sohn TA, Sauter PK, Coleman J, Pitt HA, Yeo CJ. Is prophylactic gastrojejunostomy indicated for unresectable periampullary cancer? A prospective randomized trial. Ann Surg 1999;230:322–328.
Mortenson MM, Ho HS, Bold RJ. An analysis of cost and clinical outcome in palliation for advanced pancreatic cancer. Am J Surg 2005;190:406–411.
Labori KJ, Hjermstad MJ, Wester T, Buanes T, Loge JH. Symptom profiles and palliative care in advanced pancreatic cancer: a prospective study. Support Care Cancer 2006;14:1126–1133.
Artifon EL, Sakai P, Cunha JE, Dupont A, Filho FM, Hondo FY, Ishioka S, Raju GS. Surgery or endoscopy for palliation of biliary obstruction due to metastatic pancreatic cancer. Am J Gastroenterol 2006;101:2031–2037.
Maire F, Hammel P, Ponsot P, Aubert A, O’Toole D, Hentic O, Levy P, Ruszniewski P. Long-term outcome of biliary and duodenal stents in palliative treatment of patients with unresectable adenocarcinoma of the head of the pancreas. Am J Gastroenterol 2006;101:735–742.
Yan BM, Myers RP. Neurolytic celiac plexus block for pain control in unresectable pancreatic cancer. Am J Gastroenterol 2007;102:430–438.
Lillemoe KD, Cameron JL, Kaufman HS, Yeo CJ, Pitt HA, Sauter PK. Chemical splanchnicectomy in patients with unresectable pancreatic cancer. A prospective randomized trial. Ann Surg 1993;217:447–455.
Kuhlmann KF, de Castro SM, Wesseling JG, ten Kate FJ, Offerhaus GJ, Busch OR, van Gulik TM, Obertop H, Gouma DJ. Surgical treatment of pancreatic adenocarcinoma; actual survival and prognostic factors in 343 patients. Eur J Cancer 2004;40:549–558.
Velanovich V. Using quality-of-life measurements in clinical practice. Surgery 2007;141:127–133.
Huang JJ, Yeo CJ, Sohn TA, Lillemoe KD, Sauter PK, Coleman J, Hruban RH, Cameron JL. Quality of life and outcomes after pancreaticoduodenectomy. Ann Surg 2000;231:890–898.
Velanovich V. Using quality-of-life instruments to assess surgical outcomes. Surgery 1999;126:1–4.
Testa MA, Simonson D. Assessment of quality of life outcomes. N Engl J Med 1996;334:835–840.
Nieveen van Dijkum EJ, Kuhlmann KF, Terwee CB, Obertop H, de Haes JC, Gouma DJ. Quality of life after curative or palliative surgical treatment of pancreatic and periampullary carcinoma. Br J Surg 2005;92:471–477.
Billings BJ, Christein JD, Harmsen WS, Harrington JR, Chari ST, Que FG, Farnell MB, Nagorney DM, Sarr MG. Quality-of-life after total pancreatectomy: is it really that bad on long-term follow-up? J Gastrointest Surg 2005;9:1059–1066.
Nguyen TC, Sohn TA, Cameron JL, Lillemoe KD, Campbell KA, Coleman J, Sauter K, Abrams RA, Hruban RH, Yeo CJ. Standard vs. radical pancreaticoduodenectomy for periampullary adenocarcinoma: a prospective, randomized trial evaluating quality of life in pancreaticoduodenectomy survivors. J Gastrointest Surg 2003;7:1–9.
Farnell MB, Pearson RK, Sarr MG, DiMagno EP, Burgart LJ, Dahl TR, Foster N, Sargent DJ, Pancreas Cancer Working Group. A prospective randomized trial comparing standard pancreaticoduodenectomy with pancreaticoduodenectomy with extended lymphadenectomy in resectable pancreatic head adenocarcinoma. Surgery 2005;138:618–628.
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, Silberman M, Yellen SB, Winicour P, Brannon J. The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol 1993;11:570–579.
Heffernan N, Cella DF, Webster K, Odom L, Martone M, Passik S, Bookbinder M, Fong Y, Jarnagin W, Blumgart L. Measuring health-related quality of life in patients with hepatobiliary cancers: the functional assessment of cancer therapy—hepatobiliary questionnaire. J Clin Oncol 2002;20:2229–2239.
Steel JL, Eton DT, Cella D, Olek MC, Carr BI. Clinically meaningful differences in health-related quality of life in patients diagnosed with hepatobiliary carcinoma. Ann Oncol 2006;17:304–312.
Brożek JL, Guyatt HG, Schünemann HJ. How a well-grounded minimal important difference can enhance transparency of labeling claims and improve interpretation of a patient reported outcome measure. Health Qual Life Outcomes 2006;4:1–7.
Morrow M, Hilaris B, Brennan MF. Comparison of conventional surgical resection, radioactive implantation, and bypass procedure for exocrine carcinoma of the pancreas 1975–1980. Ann Surg 1984;199:1–5.
Trede M, Schwall G, Saeger HD. Survival after pancreaticoduodenectomy: 118 consecutive resections without mortality. Ann Surg 1990;211:430–438.
Yeo CJ, Cameron JL, Sohn TA, Lillemoe KD, Pitt HA, Talamini MA, Hruban RH, Ord SE, Sauter PK, Coleman J, Zahurak ML, Grochow LB, Abrams RA. Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s: pathology, complications, outcomes. Ann Surg 1997;226:248–260.
Warshaw AL, Fernandez-del Castillo C. Pancreatic carcinoma. N Engl J Med 1992;326:455–465.
Nitecki SS, Sarr MG, Colby TV, van Heerden JA. Long-term survival after resection for ductal adenocarcinoma of the pancreas. Is it really improving? Ann Surg 1995;221:59–66.
Sohn TA, Yeo CJ, Cameron JL, Koniaris L, Kaushal S, Abrams RA, Sauter PK, Coleman J, Hruban RH, Lillemoe KD. Resected adenocarcinoma of the pancreas—616 patients: results, outcomes, and prognostic indicators. J Gastroint Surger 2000;4:567–579.
Riall TS, Nealon WH, Goodwin JS, Zhang D, Kuo YF, Townsend CM Jr, Freeman JL. Pancreatic cancer in the general population: improvements in survival over the last decade. J Gastrointest Surg 2006;10:1212–1224.
Masucco P, Capussotti L, Magnino A, Sperti E, Gatti M, Muratore A, Sgotto E, Gabriele P, Aglietta M. Pancreatic resections after chemoradiotherapy for locally advanced ductal adenocarcinoma: analysis of perioperative outcome and survival. Ann Surg Oncol 2006;13:1201–1208.
Schniewind B, Bestmann B, Henne-Bruns D, Faendrich F, Kremer B, Kuechler T. Quality of life after pancreaticoduodenectomy for ductal adenocarcinoma of the pancreatic head. Br J Surg 2006;93:1099–1107.
Revicki D. FDA draft guidance and health-outcomes research. Lancet 2007;369:540–542.
Holzner B, Bode RK, Hahn EA, Cella D, Kopp M, Sperner-Unterweger B, Kemmler G. Equating EORTC QLQ-C30 and FACT-G scores and its use in oncological research. Eur J Cancer 2006;42:3169–3177.
Wong GY, Schroeder DR, Carns PE, Wilson JL, Martin DP, Kinney MO, Mantilla CB, Warner DO. Effect of neurolytic celiac plexus block on pain relief, quality of life, and survival in patients with unresectable pancreatic cancer: a randomized controlled trial. JAMA 2004;291:1092–1099.
Acknowledgment
Dr. Crippa was supported by the International Hepato-Pancreato-Biliary Association (2007 Warren Fellowship Award). Dr. Domínguez was supported by the Fundacion Mexico en Harvard A.C.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussion
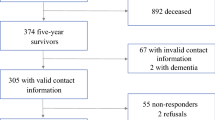
Thomas J. Howard, MD (Indianapolis, IN): This study is unique and what is unique about it is that they classified patients into three clinically relevant stages: Stage I is patients with localized cancer, stage II is patients with locally advanced cancer, and stage III is patients with metastatic cancer. They used a validated instrument to prospectively measure health-related quality of life, and they have an acceptable 59% response rate at 6 months. Their survival rates were as expected with a median survival of 9.8 months in the entire cohort and significant improvement in survival and health-related quality of life in those patients able to be resected. In contrast, patients with metastatic disease showed significant overall decline in health-related quality of life over time. These data fail to show the benefit of the use of chemotherapy or chemoradiotherapy in these patients, and I have several questions regarding this.
Question number one is, bias, in particular in studies with limited accrual, is a constant nemesis. I assume these patients represent a nonselected sampling of patients who were seen over this 16-month period at the MGH. Besides the 102 patients that were enrolled in your study, how many other patients with pancreatic adenocarcinoma were treated at your institution who declined to be part of this enrollment?
My second question is that the FACT-G questionnaire, as you know, covers multiple health dimensions expressed by four subscale measurements: physical, social, emotional, and functional well-being. Did you find any differences either within or between groups in these subscales rather than just the overall scale to explain the findings that you report?
And my last question is could you speculate to the reasons, e.g., perhaps lack of a control group, underpowered, or the use of combination therapy, that you failed to identify any clinical benefit response to the use of systemic chemotherapy in your cohort of patients with pancreatic cancer?
Stefano Crippa, MD (Boston, MA): Thank you for reviewing our manuscript in advance and for these excellent questions. The first question is whether our patients represent no selected sampling of patients seen at Mass General Hospital during the study period. Well, every year, approximately 250 patients are referred to our hospital with the diagnosis of pancreatic cancer, and of these, 15% will undergo surgical resection. They come through different routes. Some are referred to the department of surgery, basically patients with localized disease, but many others with advanced pancreatic cancer and metastatic pancreatic cancer are referred to the department of oncology just for a second opinion or to the department of gastroenterology to have a stent placed. Many patients with advanced pancreatic cancer after the workup at Mass General will be followed out in other hospitals outside MGH. Therefore, we first tried to enroll in this study those patients who were actually treated at our institution to have more specific and detailed data regarding their treatment, the need for readmission, stents, and so on. And I have to say that a few patients declined to participate in the study.
The second question regards differences in subscale analysis among the three groups. Actually, we did not perform a subscale analysis. We analyzed only the FACT-G and the FACT-Hep models and the TOI, the trial outcome index, which is the sum of the functional, physical, and disease-specific models. Basically, the TOI gives you a better idea on the functional and physiological status of these patients, and we found an improvement of the TOI in patients with localized disease who underwent surgery, and this was a surprise for us. As expected, a decrease of the physiological and functional status in patients with advanced and, in particular, metastatic pancreatic cancer was found.
Finally, why our study failed to show a clinical benefit in patients with metastatic cancer. I agree with you that our study is certainly underpowered and we have a small sample size for each group. However, when we talk about patients with metastatic cancer and we look at the studies reported in the literature, we have to consider that, in many cases, the clinical benefit is measured in terms of a few weeks of improved survival, and I am not sure that this data is perceived as important, meaningful, or whether relevant by the single patient. Therefore, I think that, in this subset of patients, probably more detailed quality of life studies are needed.
Jennifer F. Tseng, MD (Boston, MA): This is a very nicely presented work from a great center. I have a comment and a question. It is a truism in those people who study quality of life that all quality of life is relative and that, in fact, when they have done studies of people that have either (a) won the lottery or (b) had an amputation, 12 months later, those people’s quality of life is equivalent. Therefore, my question to you is about the arbitrary nature of time points at 0, 3, and 6 months, et cetera. Did resection occur at 0 months, and so then, the first data point was three months after presumably any complications?
Dr. Crippa: Yes.
Dr. Tseng: Can you stratify by people that actually had surgical complications and people that did not have surgical complications?
Dr. Crippa: We did not do that because we had only 29 patients who had surgical resection, 28 with localized disease and one with locally advanced. Sorry, I cannot answer.
Dr. Tseng: And then if you follow those patients out, it will be interesting if you can present this in a year or two and see actually if those patients who underwent resections quality of life also diminishes, as one would expect, to the same level as those who did not undergo resection.
Dr. Crippa: For this study, we decided to evaluate quality of life at 3 and 6 months because this study was not focused only on patients with localized pancreatic cancer who had resection but also on patients with locally advanced or metastatic pancreatic cancer. Therefore, we scheduled the questionnaire time at 3 and 6 months because the median survival of metastatic patients is only 6 months. This is why we chose also this particular time.
O. Joe Hines, M.D. (Los Angeles, CA): I enjoyed your talk. Although pancreatic cancer is a grim disease, there are some lights of hope, so I don’t absolutely agree with your comparison to data that is from the 1970s and 1980s. There are some groups of patients that are having significantly improved survivals over the past 5 years, upwards of 35% to 40% 5-year survivals. My question for you really relates to the way you grouped your patients. You chose to group them by a staging system that is something that you developed for your study, and so, when someone looks at your paper and reads your data, it is going to be difficult for them to compare it to their own experience. I wonder why it is that you used this grouping. And secondly, have you had the chance to use something like the AJCC staging system to compare the groups so that others can understand the information in your paper a little better?
Dr. Crippa: We did not use the AJCC system. We basically decided to classify the patients according to their status at presentation. Therefore, these patients had a CT scan, endoscopic ultrasound, a detailed imaging workup, and they were classified in localized disease and locally advanced if there was an encasement of the vessel or an infiltration of the retroperitoneum without evidence of metastatic disease, and finally, patients with metastatic disease. We decided to do that because that was the presentation of our patients, and we did not do a stratification according to the AJCC system, which is a pathological and not a clinical classification.
Rights and permissions
About this article
Cite this article
Crippa, S., Domínguez, I., Rodríguez, J.R. et al. Quality of Life in Pancreatic Cancer: Analysis by Stage and Treatment. J Gastrointest Surg 12, 783–794 (2008). https://doi.org/10.1007/s11605-007-0391-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-007-0391-9