Abstract
Purpose
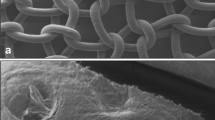
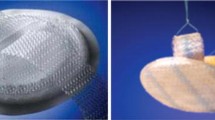
To evaluate two bioprostheses derived from bovine pericardium, one cross-linked (Peri-Guard®) and the other non-cross-linked (Veritas®), and to compare them with Alloderm® and Permacol® for abdominal wall repair.
Methods
The four prostheses were tested in acute and chronic hernia models. Prostheses were either sutured to the edge of the abdominal wall defect (inlay) or secured as an underlay with surgical tacks. Evaluation at 3 and 6 months included adhesion formation, defect area size and thickness, tensile strength, and histology.
Results
Mean adhesion coverage area ranged from 25 to 31%. The two cross-linked materials, Permacol and Peri-Guard, showed greater tensile strength. Significant defect contraction followed repair with Veritas, whereas Alloderm stretched. All prostheses had cellular ingrowth and neovascularization by 3 months. No significant differences were found in prosthesis to abdominal wall breaking strength. Operative site infection occurred in six animals (5 Peri-Guard, 1 Veritas), and overlying skin ulceration in six others (6 Peri-Guard).
Conclusions
Permacol provided a strong and durable repair for up to six months. Peri-Guard was equally strong but prone to infection and to skin ulceration. With time, Veritas and Alloderm lost tensile strength associated with marked thinning and with hernia-like bulging in the case of Alloderm.







Similar content being viewed by others
References
Mudge M, Hughes LE. Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg 1985;72:70–71.
Regnard JF, Hay JM, Rea S. Ventral incisional hernias: incidence, date of recurrence, localization and risk factors. Ital J Surg Sci 1988;18:259–265.
Luijendijk RW, Hop WC, van den Tol MP, de Lange DC, Braaksma MM, IJzermans JN, Boelhouwer RU, de Vries BC, Salu MK, Wereldsma JC, Bruijninckx CM, Jeekel J. A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 2000;343:392–398.
Bucknall TE, Cox PJ, Ellis H. Burst abdomen and incisional hernia: a prospective study of 1129 major laparotomies. BMJ 1982;284:931–933.
Anthony T, Bergen PC, Kim LT, Henderson M, Fahey T, Rege RV, Turnage RH. Factors affecting recurrence following incisional herniorrhaphy. World J Surg 2000;24:95–100.
Burger JW, Luijendijk RW, Hop WC. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 2004;240:578–583.
Basoglu M, Yildirgan MI, Yilmaz I, Balik A, Celebi F, Atamanalp SS, Polat KY, Oren D. Late complications of incisional hernias following prosthetic mesh repair. Acta Chir Belg 2004;104:425–428.
Leber GE, Garb JL, Alexander AI, Reed WP. Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg 1998;133:378–382.
Luijendijk RW, Lemmen MH, Hop WC, Wereldsma JC. Incisional hernia recurrence following “vest-over-pants” or vertical Mayo repair of primary hernias of the midline. World J Surg 1997;21:62–65.
Clagett GP, Bowers BL, Lopez-Viego MA, Rossi MB, Valentine RJ, Myers SI, Chervu A. Creation of a neo-aortoiliac system from lower extremity deep and superficial veins. Ann Surg 1993;218:239–248.
Usher FC. Hernia repair with Marlex mesh. An analysis of 541 cases. Arch Surg 1962;84:325–328.
Mathes SJ, Steinwald PM, Foster RD, Hoffman WY, Anthony JP. Complex abdominal wall reconstruction: a comparison of flap and mesh closure. Ann Surg 2000;232:586–596.
Ramirez OM, Ruas E, Dellon AL. “Component separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg 1990;86:519–526.
de Vries Reilingh TS, van Goor H, Rosman C, Bemelmans MH, de Jong D, van Nieuwenhoven EJ, van Engeland MI, Bleichrodt RP. “Component separation technique” for the repair of large abdominal wall hernias. J Am Coll Surg 2003;196:32–37.
Lowe JB 3rd, Lowe JB, Baty JD, Garza JR. Risks associated with “component separation” for closure of complex abdominal wall defects. Plast Reconstr Surg 2003;111:1276–1283.
Abolhoda A, Yu S, Oyarzun JR, McCormick JR, Bogden JD, Gabbay S. Calcification of bovine pericardium: glutaraldehyde versus no-react biomodification. Ann Thorac Surg 1996;62:169–174.
Courtman DW, Errett BF, Wilson GJ. The role of crosslinking in modification of the immune response elicited against xenogenic vascular acellular matrices. J Biomed Mater Res 2001;55:576–586.
Mazuji MK, Kalambaheti K, Pawar B. Prevention of adhesions with polyvinylpyrrolidone. Arch Surg 1964;89:1011–1015.
Gecim IE, Kocak S, Ersoz S, Bumin C, Aribal D. Recurrence after incisional hernia repair: results and risk factors. Surg Today 1996;26:607–609.
Park A, Birch DW, Lovrics P. Laparoscopic and open incisional hernia repair: a comparison study. Surgery 1998;124:816–821.
Rios A, Rodriguez JM, Munitiz V, Alcaraz P, Perez Flores D, Parrilla P. Antibiotic prophylaxis in incisional hernia repair using a prosthesis. Hernia 2001;5:148–152.
Heniford BT, Park A, Ramshaw BJ, Voeller G. Laparoscopic repair of ventral hernias: nine years experience with 850 consecutive hernias. Ann Surg 2003;238:391–399.
LeBlanc KA, Booth WV, Whitaker JM, Bellanger DE. Laparoscopic incisional and ventral herniorraphy: our initial 100 patients. Hernia 2001;5:41–45.
Klinge U, Junge K, Spellerberg B, Piroth C, Klosterhalfen B, Schumpelick V. Do multifilament alloplastic meshes increase the infection rate? Analysis of the polymeric surface, the bacteria adherence, and the in vivo consequences in a rat model. J Biomed Mater Res 2002;63:765–771.
Harrell AG, Novitsky YW, Kercher KW, Foster M, Burns JM, Kuwada TS, Heniford BT. In vitro infectability of prosthetic mesh by methicillin-resistant Staphylococcus aureus. Hernia 2006;10:120–124.
Jansen B, Schumacher-Perdreau F, Peters G, Pulverer G. New aspects in the pathogenesis and prevention of polymer-associated foreign-body infections caused by coagulase-negative staphylococci. J Invest Surg 1989;2:361–380.
Bleichrodt RP, Simmermacher RK, van der Lei B, Schakenraad JM. Expanded polytetrafluoroethylene patch versus polypropylene mesh for the repair of contaminated defects of the abdominal wall. Surg Gynecol Obstet 1993;176:18–24.
Brown GL, Richardson JD, Malangoni MA, Tobin GR, Ackerman D, Polk HC Jr. Comparison of prosthetic materials for abdominal wall reconstruction in the presence of contamination and infection. Ann Surg 1985;201:705–711.
Demirer S, Gecim IE, Aydinuraz K, Ataoglu H, Yerdel MA, Kuterdem E. Affinity of Staphylococcus epidermidis to various prosthetic graft materials. J Surg Res 2001;99:170–174.
Malaisrie SC, Malekzadeh S, Biedlingmaier JF. In vivo analysis of bacterial biofilm formation on facial plastic bioimplants. Laryngoscope 1998;108:1733–1738.
Matthews BD, Pratt BL, Pollinger HS, Backus CL, Kercher KW, Sing RF, Heniford BT. Assessment of adhesion formation to intra-abdominal polypropylene mesh and polytetrafluoroethylene mesh. J Surg Res 2003;114:126–132.
Gibbons RJ, MacDonald JB. Degradation of collagenous substrates by Bacteroides melaninogenicus. J Bacteriol 1961;81:614–621.
Waldvogel FA, Swartz MN. Collagenolytic activity of bacteria. J Bacteriol 1969;98:662–667.
Oliver RF, Grant RA, Cox RW, Hulme MJ, Mudie A. Histological studies of subcutaneous and intraperitoneal implants of trypsin-prepared dermal collagen allografts in the rat. Clin Orthop Relat Res 1976;115:291–302.
Oliver RF, Barker H, Cooke A, Grant RA. Dermal collagen implants. Biomaterials 1982;3:38–40.
Helton WS, Fisichella PM, Berger R, Horgan S, Espat NJ, Abcarian H. Short-term outcomes with small intestinal submucosa for ventral abdominal hernia. Arch Surg 2005;140:549–560.
Ueno T, Pickett LC, de la Fuente SG, Lawson DC, Pappas TN. Clinical application of porcine small intestinal submucosa in the management of infected or potentially contaminated abdominal defects. J Gastrointest Surg 2004;8:109–112.
Petter-Puchner AH, Fortelny RH, Mittermayr R, Walder N, Ohlinger W, Redl H. Adverse effects of porcine small intestine submucosa implants in experimental ventral hernia repair. Surg Endosc 2006;20:942–946.
Carbonell AM, Matthews BD, Dreau D, Foster M, Austin CE, Kercher KW, Sing RF, Heniford BT. The susceptibility of prosthetic biomaterials to infection. Surg Endosc 2005;19:430–435.
Konstantinovic ML, Lagae P, Zheng F, Verbeken EK, De Ridder D, Deprest JA. Comparison of host response to polypropylene and non-cross-linked porcine small intestine serosal-derived collagen implants in a rat model. BJOG 2005;112:1554–1560.
Badylak S, Kokini K, Tullius B, Simmons-Byrd A, Morff R. Morphologic study of small intestinal submucosa as a body wall repair device. J Surg Res 2002;103:190–202.
Soiderer EE, Lantz GC, Kazacos EA, Hodde JP, Wiegand RE. Morphologic study of three collagen materials for body wall repair. J Surg Res 2004;118:161–175.
Badylak SF, Kropp B, McPherson T, Liang H, Snyder PW. Small intestional submucosa: a rapidly resorbed bioscaffold for augmentation cystoplasty in a dog model. Tissue Eng 1998;4:379–387.
Badylak SF, Park K, Peppas N, McCabe G, Yoder M. Marrow-derived cells populate scaffolds composed of xenogeneic extracellular matrix. Exp Hematol 2001;29:1310–1318.
Clarke KM, Lantz GC, Salisbury SK, Badylak SF, Hiles MC, Voytik SL. Intestine submucosa and polypropylene mesh for abdominal wall repair in dogs. J Surg Res 1996;60:107–114.
Company brochure. Tissue Science 2006.
Silverman RP, Li EN, Holton LH 3rd, Sawan KT, Goldberg NH. Ventral hernia repair using allogenic acellular dermal matrix in a swine model. Hernia 2004;8(4):336–342.
Harper JR. Tissue regeneration using human acellular tissue matrix: a histological perspective. LifeCell Clinical Monograph Series (2005).
Gupta A, Zahriya K, Mullens PL, Salmassi S, Keshishian A. Ventral herniorrhaphy: experience with two different biosynthetic mesh materials, Surgisis and Alloderm. Hernia 2006;10:419–425.
Cobb WS, Burns JM, Kercher KW, Matthews BD, James Norton H, Todd Heniford B. Normal intraabdominal pressure in healthy adults. J Surg Res 2005;129:231–235.
Franklin ME Jr, Gonzalez JJ Jr, Glass JL. Use of porcine small intestinal submucosa as a prosthetic device for laparoscopic repair of hernias in contaminated fields: 2-year follow-up. Hernia 2004;8:186–189.
Diaz JJ Jr, Guy J, Berkes MB, Guillamondegui O, Miller RS. Acellular dermal allograft for ventral hernia repair in the compromised surgical field. Am Surg 2006;72:1181–1187.
Patton JH Jr, Berry S, Kralovich KA. Use of human acellular dermal matrix in complex and contaminated abdominal wall reconstructions. Am J Surg 2007;193:360–363.
Catena F, Ansaloni L, Gazzotti F, Gagliardi S, Di Saverio S, D’Alessandro L, Pinna AD. Use of porcine dermal collagen graft (Permacol) for hernia repair in contaminated fields. Hernia 2007;11:57–60.
Parker DM, Armstrong PJ, Frizzi JD, North JH Jr. Porcine dermal collagen (Permacol) for abdominal wall reconstruction. Curr Surg 2006;63:255–258.
Dayton MT. Use of absorbable mesh in repair of contaminated abdominal wall defects. In: Bendavid R, ed. Prostheses and abdominal wall hernias. Austin: RG Landes Co, 1994, pp 293–299.
Dayton MT, Buchele BA, Shirazi SS, Hunt LB. Use of an absorbable mesh to repair contaminated abdominal-wall defects. Arch Surg 1986;121:954–960.
Tyrell J, Silberman H, Chandrasoma P, Niland J, Shull J. Absorbable versus permanent mesh in abdominal operations. Surgery 1989;168:227–232.
Halm JA, de Wall LL, Steyerberg EW, Jeekel J, Lange JF. Intraperitoneal polypropylene mesh hernia repair complicates subsequent abdominal surgery. World J Surg 2007;31:423–429.
Kaufman Z, Engelberg M, Zager M. Fecal fistula: a late complication of Marlex mesh repair. Dis Colon Rectum 1981;24:543–544.
Miller K, Junger W. Ileocutaneous fistula formation following laparoscopic polypropylene mesh hernia repair. Surg Endosc 1997;11:772–773.
Seelig MH, Kasperk R, Tietze L, Schumpelick V. Enterocutaneous fistula after Marlex net implantation. A rare complication after incisional hernia repair. Chirurg 1995;66:739–741.
Molloy RG, Moran KT, Waldron RP, Brady MP, Kirwan WO. Massive incisional hernia: abdominal wall replacement with Marlex mesh. Br J Surg 1991;78:242–244.
Liakakos T, Karanikas I, Panagiotidis H, Dendrinos S. Use of Marlex mesh in the repair of recurrent incisional hernia. Br J Surg 1994;81:248–249.
Sugerman HJ, Kellum JM Jr, Reines HD, DeMaria EJ, Newsome HH, Lowry JW. Greater risk of incisional hernia with morbidly obese than steroid-dependent patients and low recurrence with prefascial polypropylene mesh. Am J Surg 1996;171:80–84.
Vrijland WW, Jeekel J, Steyerberg EW, Den Hoed PT, Bonjer HJ. Intraperitoneal polypropylene mesh repair of incisional hernia is not associated with enterocutaneous fistula. Br J Surg 2000;87:348–352.
Acknowledgement
The authors have no financial disclosures to declare. This experimental study was sponsored entirely by: Synovis Surgical Innovations, 2575 University Ave. W., St. Paul, MN 55114.
Author information
Authors and Affiliations
Corresponding author
Additional information
Accepted for oral presentation (Quick Shot) at the annual meeting of The Society for Surgery of the Alimentary Tract, Digestive Disease Week, Washington D.C., May 2007.
Rights and permissions
About this article
Cite this article
Gaertner, W.B., Bonsack, M.E. & Delaney, J.P. Experimental Evaluation of Four Biologic Prostheses for Ventral Hernia Repair. J Gastrointest Surg 11, 1275–1285 (2007). https://doi.org/10.1007/s11605-007-0242-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-007-0242-8