Abstract
Introduction
The purpose of this study was to compare rates and patterns of disease progression following percutaneous, image-guided radiofrequency ablation (RFA) and nonanatomic wedge resection for solitary colorectal liver metastases.
Methods
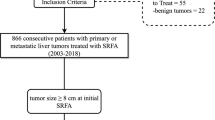
We identified 30 patients who underwent nonanatomic wedge resection for solitary liver metastases and 22 patients who underwent percutaneous RFA because of prior major hepatectomy (50%), major medical comorbidities (41%), or relative unresectability (9%). Serial imaging studies were retrospectively reviewed for evidence of local tumor progression.
Results
Patients in the RFA group were more likely to have undergone prior liver resection, to have a disease-free interval greater than 1 year, and to have had an abnormal carcinoembryonic antigen (CEA) level before treatment. Two-year local tumor progression-free survival (PFS) was 88% in the Wedge group and 41% in the RFA group. Two patients in the RFA group underwent re-ablation, and two patients underwent resection to improve the 2-year local tumor disease-free survival to 55%. Approximately 30% of patients in each group presented with distant metastasis as a component of their first recurrence. Median overall survival from the time of resection was 80 months in the Wedge group vs 31 months in the RFA group. However, overall survival from the time of treatment of the colorectal primary was not significantly different between the two groups.
Conclusions
Local tumor progression is common after percutaneous RFA. Surgical resection remains the gold standard treatment for patients who are candidates for resection. For patients who are poor candidates for resection, RFA may help to manage local disease, but close follow-up and retreatment are necessary to achieve optimal results.





Similar content being viewed by others
References
Scheele J, Altendorf-Hofmann A, Grube T, Hohenberger W, Stangl R, Schmidt K. Resection of colorectal liver metastases. What prognostic factors determine patient selection? Chirurg 2001;72(5):547–560.
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 1999;230(3):309–318; discussion 318–321.
Choti MA, Sitzmann JV, Tiburi MF, Sumetchotimetha W, Rangsin R, Schulick RD, et al. Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg 2002;235(6):759–766.
Jamison RL, Donohue JH, Nagorney DM, Rosen CB, Harmsen WS, Ilstrup DM. Hepatic resection for metastatic colorectal cancer results in cure for some patients. Arch Surg 1997;132(5):505–510; discussion 511.
Curley SA, Izzo F, Delrio P, Ellis LM, Granchi J, Vallone P, et al. Radiofrequency ablation of unresectable primary and metastatic hepatic malignancies: results in 123 patients. Ann Surg 1999;230(1):1–8.
Goldberg SN, Solbiati L, Hahn PF, Cosman E, Conrad JE, Fogle R, et al. Large-volume tissue ablation with radio frequency by using a clustered, internally cooled electrode technique: laboratory and clinical experience in liver metastases. Radiology 1998;209(2):371–379.
Solbiati L, Livraghi T, Goldberg SN, Ierace T, Meloni F, Dellanoce M, et al. Percutaneous radio-frequency ablation of hepatic metastases from colorectal cancer: long-term results in 117 patients. Radiology 2001;221(1):159–166.
Bleicher RJ, Allegra DP, Nora DT, Wood TF, Foshag LJ, Bilchik AJ. Radiofrequency ablation in 447 complex unresectable liver tumors: lessons learned. Ann Surg Oncol 2003;10(1):52–58.
Curley SA, Marra P, Beaty K, Ellis LM, Vauthey JN, MD, Abdalla EK, et al. Early and late complications after radiofrequency ablation of malignant liver tumors in 608 patients. Ann Surg 2004;239(4):450–458.
de Baere T, Elias D, Dromain C, El din MG, Kuoch V, Ducreux M, et al. Radiofrequency ablation of 100 hepatic metastases with a mean follow-up of more than 1 year. AJR Am J Roentgenol 2000;175(6):1619–1625.
Livraghi T, Solbiati L, Meloni F, Ierace T, Goldberg SN, Gazelle GS. Percutaneous radiofrequency ablation of liver metastases in potential candidates for resection: the “test-of-time approach”. Cancer 2003;97(12):3027–3035.
Scudamore CH, Lee SI, Patterson EJ, Buczkowski AK, July LV, Chung SW, et al. Radiofrequency ablation followed by resection of malignant liver tumors. Am J Surg 1999;177(5):411–417.
Goldberg SN, Gazelle GS, Compton CC, Mueller PR, Tanabe KK. Treatment of intrahepatic malignancy with radiofrequency ablation: radiologic–pathologic correlation. Cancer 2000;88(11):2452–2463.
Mulier S, Ni Y, Jamart J, Ruers T, Marchal G, Michel L. Local recurrence after hepatic radiofrequency coagulation: multivariate meta-analysis and review of contributing factors. Ann Surg 2005;242(2):158–171.
van Duijnhoven FH, Jansen MC, Junggeburt JM, van Hillegersberg R, Rijken AM, van Coevorden F, et al. Factors influencing the local failure rate of radiofrequency ablation of colorectal liver metastases. Ann Surg Oncol 2006; 13:651–658
Machi J, Uchida S, Sumida K, Limm WM, Hundahl SA, Oishi AJ, et al. Ultrasound-guided radiofrequency thermal ablation of liver tumors: percutaneous, laparoscopic, and open surgical approaches. J Gastrointest Surg 2001;5(5):477–489.
Grobmyer SR, Fong Y, D’Angelica M, Dematteo RP, Blumgart LH, Jarnagin WR. Diagnostic laparoscopy prior to planned hepatic resection for colorectal metastases. Arch Surg 2004;139(12):1326–1330.
Elias D, Sideris L, Pocard M, de Baere T, Dromain C, Lassau N, et al. Incidence of unsuspected and treatable metastatic disease associated with operable colorectal liver metastases discovered only at laparotomy (and not treated when performing percutaneous radiofrequency ablation). Ann Surg Oncol 2005;12(4):298–302.
Chung MH, Wood TF, Tsioulias GJ, Rose DM, Bilchik AJ. Laparoscopic radiofrequency ablation of unresectable hepatic malignancies. A phase 2 trial. Surg Endosc 2001;15(9):1020–1026.
Oshowo A, Gillams A, Harrison E, Lees WR, Taylor I. Comparison of resection and radiofrequency ablation for treatment of solitary colorectal liver metastases. Br J Surg 2003;90(10):1240–1243.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40(5):373–383.
Aloia TA, Vauthey JN, Loyer E, Ribero D, Pawlik TM, Wei SH, et al. Solitary colorectal liver metastasis: resection determines outcome. Arch Surg 2006;141(5):460–467.
Lencioni R, Crocetti L, Cioni D, Della Pina C, Bartolozzi C. Percutaneous radiofrequency ablation of hepatic colorectal metastases: technique, indications, results, and new promises. Invest Radiol 2004;39(11):689–697.
Petrowsky H, Gonen M, Jarnagin W, Lorenz M, Dematteo R, Heinrich S, et al. Second liver resections are safe and effective treatment for recurrent hepatic metastases from colorectal cancer: a bi-institutional analysis. Ann Surg 2002;235(6):863–871.
Berber E, Pelley R, Siperstein AE. Predictors of survival after radiofrequency thermal ablation of colorectal cancer metastases to the liver: a prospective study. J Clin Oncol 2005;23(7):1358–1364.
Abdalla EK, Vauthey JN, Ellis LM, Ellis V, Pollock R, Broglio KR, et al. Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg 2004;239(6):818–825; discussion 825–827.
Allen PJ, Kemeny N, Jarnagin W, DeMatteo R, Blumgart L, Fong Y. Importance of response to neoadjuvant chemotherapy in patients undergoing resection of synchronous colorectal liver metastases. J Gastrointest Surg 2003;7(1):109–115; discussion 116–117.
Lambert LA, Colacchio TA, Barth RJ, Jr. Interval hepatic resection of colorectal metastases improves patient selection. Arch Surg 2000;135(4):473–479; discussion 479–480.
Adam R, Pascal G, Castaing D, Azoulay D, Delvart V, Paule B, et al. Tumor progression while on chemotherapy: a contraindication to liver resection for multiple colorectal metastases? Ann Surg 2004;240(6):1052–1061; discussion 1061–1064.
Author information
Authors and Affiliations
Corresponding author
Additional information
White and Avital contributed equally.
Rights and permissions
About this article
Cite this article
White, R.R., Avital, I., Sofocleous, C.T. et al. Rates and Patterns of Recurrence for Percutaneous Radiofrequency Ablation and Open Wedge Resection for Solitary Colorectal Liver Metastasis. J Gastrointest Surg 11, 256–263 (2007). https://doi.org/10.1007/s11605-007-0100-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-007-0100-8