Abstract
Purpose:
To examine clinical features and outcome of patients who underwent hepatic resection for colorectal liver metastases (LM) involving the caudate lobe.
Patients and Methods:
Consecutive patients who underwent hepatic resection for LM from May 1990 to September 2004 were analyzed from a multicenter database. Demographics, operative data, pathologic margin status, recurrence, and survival were analyzed.
Results:
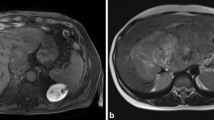
Of 580 patients, 40 (7%) had LM involving the caudate. Six had isolated caudate LM and 34 had LM involving the caudate plus one or more other hepatic segments. Patients with caudate LM were more likely to have synchronous primary colorectal cancer (63% vs. 36%; P = 0.01), multiple LM (70% vs. 51%; P = 0.02) and required extended hepatic resection more often than patients with non-caudate LM (60% vs. 18%; P < 0.001). Only four patients with caudate LM underwent a vascular resection; three at first operation, one after recurrence of a resected caudate tumor. All had primary repair (vena cava, n = 3; portal vein, n = 1). Perioperative complications (43% vs. 28%) and 60-day operative mortality (0% vs. 1%) were similar (caudate vs. non-caudate LM, both P > 0.05). Pathological margins were positive in 15 (38%) patients with caudate LM and in 43 (8%) with non-caudate LM (P < 0.001). At a median follow-up of 40 months, 25 (64%) patients with caudate LM recurred compared with 219 (40%) patients with non-caudate LM (P = 0.01). Patients with caudate LM were more likely to have intrahepatic disease as a component of recurrence (caudate: 51% vs. non-caudate: 25%; P = 0.001). No patient recurred on the vena cava or portal vein. Patients with caudate LM had shorter 5-year disease-free and overall survival than patients with non-caudate LM (disease-free: 24% vs. 44%; P = 0.02; overall: 41% vs. 58%; P = 0.02).
Conclusions:
Patients who undergo hepatic resection for caudate LM often present with multiple hepatic tumors and tumors in proximity to the major hepatic veins. Extended hepatectomy is required in the majority, although vascular resection is not frequently necessary; when performed, primary repair is usually possible. Despite resection in this population of patients with multiple and bilateral tumors, and despite close-margin and positive-margin resection in a significant proportion, recurrence on the portal vein or vena cava was not observed, and long-term survival is accomplished (41% 5-year overall survival).




Similar content being viewed by others
References
Abdalla EK, Adam R, Bilchik AJ, Jaeck D, Vauthey JN, Mahvi D. Improving resectability of hepatic colorectal metastases: Expert Consensus Statement. Ann Surg Oncol 2006 13(10), 1271–1280.
Choti MA, Sitzmann JV, Tiburi MF, Sumetchotimetha W, Rangsin R, Schulick RD, Lillemoe KD, Yeo CJ, Cameron JL. Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg 2002;235:759–766.
Abdalla EK, Vauthey JN, Ellis LM, Ellis V, Pollock R, Broglio KR, Hess K, Curley SA. Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg 2004;239:818–25; discussion 825–827.
Fernandez FG, Drebin JA, Linehan DC, Dehdashti F, Siegel BA, Strasberg SM. Five-year survival after resection of hepatic metastases from colorectal cancer in patients screened by positron emission tomography with F-18 fluorodeoxyglucose (FDG-PET). Ann Surg 2004;240:438–47; discussion 447–450.
Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C, Curley SA, Loyer EM, Muratore A, Mentha G, Capussotti L, Vauthey JN. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg 2005;241:715–722.
Aloia TA, Vauthey JN, Loyer EM, Ribero D, Ahrar K, Pawlik TM, Zorzi D, Abdalla EK. Solitary colorectal liver metastasis: resection determines outcome. Arch Surg 2006;141:460–467.
Kumon M. Anatomy of the caudate lobe with special reference to portal vein and bile duct. Acta Hepatol Jpn 1985;26:1193–1199.
Kogure K, Kuwano H, Fujimaki N, Makuuchi M. Relation among portal segmentation, proper hepatic vein, and external notch of the caudate lobe in the human liver. Ann Surg 2000;231:223–228.
Abdalla EK, Vauthey JN, Couinaud C. The caudate lobe of the liver: implications of embryology and anatomy for surgery. Surg Oncol Clin N Am 2002;11:835–848.
Yanaga K, Matsumata T, Hayashi H, Shimada M, Urata K, Sugimachi K. Isolated hepatic caudate lobectomy. Surgery 1994;115:757–761.
Bartlett D, Fong Y, Blumgart LH. Complete resection of the caudate lobe of the liver: technique and results. Br J Surg 1996;83:1076–1081.
Sasada A, Ataka K, Tsuchiya K, Yamagishi H, Maeda H, Okada M. Complete caudate lobectomy: its definition, indications, and surgical approaches. HPB Surg 1998;11:87–93.
Fan J, Wu ZQ, Tang ZY, Zhou J, Qiu SJ, Ma ZC, Zhou XD, Yu YQ. Complete resection of the caudate lobe of the liver with tumor: technique and experience. Hepato-Gastroenterology 2001;48:808–811.
Abdalla EK, Barnett CC, Doherty D, Curley SA, Vauthey JN. Extended hepatectomy in patients with hepatobiliary malignancies with and without preoperative portal vein embolization. Arch Surg 2002;137:675-680; discussion 680–681.
Vauthey JN, Chaoui A, Do KA, Bilimoria MM, Fenstermacher MJ, Charnsangavej C, Hicks M, Alsfasser G, Lauwers G, Hawkins IF, Caridi J. Standardized measurement of the future liver remnant prior to extended liver resection: Methodology and clinical associations. Surgery 2000;127:512–519.
Strasberg SM. Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg 2005;12:351–355.
Strasberg SM. International Hepato-Pancreato-Biliary Association Terminology Committee Survey: the Brisbane 2000 Terminology of Liver Anatomy and Resections. HPB 2000;2:333–339.
Elias D, Lasser PH, Desruennes E, Mankarios H, Detroz B. Surgical approaches to segment I for malignant tumors (20 cases). J Chir (Paris) 1993;130:335–342.
Morise Z, Yamafuji K, Asami A, Takeshima K, Hayashi N, Baba H, Endo T, Hattori T, Ito Y, Tokura Y. Hepatectomy following transarterial chemotherapy for a metastasis in the caudate lobe. Hepato-Gastroenterology 2004;51:583–585.
Yamamoto H, Nagino M, Kamiya J, Hayakawa N, Nimura Y. Surgical treatment for colorectal liver metastases involving the paracaval portion of the caudate lobe. Surgery 2005;137:26–32.
Hawkins WG, DeMatteo RP, Cohen MS, Jarnagin WR, Fong Y, D'Angelica M, Gonen M, Blumgart LH. Caudate hepatectomy for cancer: a single institution experience with 150 patients. J Am Coll Surg 2005;200:345–352.
Tanaka K, Shimada H, Matsuo K, Nagano Y, Togo S. Surgical outcome of solitary colorectal metastasis to the hepatic caudate lobe. Br J Surg. 2005;92:847–848.
Kosuge T, Yamamoto J, Takayama T, Shimada K, Yamasaki S, Makuuchi M, Hasegawa H. An isolated, complete resection of the caudate lobe, including the paracaval portion, for hepatocellular carcinoma. Arch Surg 1994;129:280–284.
Asahara T, Dohi K, Hino H, Nakahara H, Katayama K, Itamoto T, E. O, Moriwaki K, Yuge O, Nakanishi T, Kitamoto M. Isolated caudate lobectomy by anterior approach for hepatocellular carcinoma originating in the paracaval portion of the caudate lobe. J Hepatobiliary Pancreat Surg 1998;5:416–421.
Yamamoto J, Kosuge T, Shimada K, Yamasaki S, Takayama T, Makuuchi M. Anterior transhepatic approach for isolated resection of the caudate lobe of the liver. World J Surg 1999;23:97–101.
Sarmiento JM, Que FG, Nagorney DM. Surgical outcomes of isolated caudate lobe resection: a single series of 19 patients. Surgery 2002;132:697–708; discussion 708–709.
Vauthey JN, Pawlik TM, Ribero D, Wu T, Zorzi D, Hoff PM, Xiong HQ, Eng C, Lauwers GY, Mino-Kenudson M, Risio M, Muratore A, Capussotti L, Curley SA, Abdalla EK. Chemotherapy regimen predicts steatohepatitis and an increase in 90-Day mortality after surgery for hepatic colorectal metastases. J Clin Oncol 2006;24:2065–2072.
Vauthey JN, Pawlik TM, Abdalla EK, Arens JF, Nemr RA, Wei SH, Kennamer DL, Ellis LM, Curley SA. Is extended hepatectomy for hepatobiliary malignancy justified? Ann Surg 2004;239:722–730; discussion 730–732.
Okada Y, Nagino M, Kamiya J, Yamamoto H, Hayakawa N, Nimura Y. Diagnosis and treatment of inferior vena caval invasion by hepatic cancer. World J Surg 2003;27:689–694.
Nardo B, Ercolani G, Montalti R, Bertelli R, Gardini A, Beltempo P, Puviani L, Pacile V, Vivarelli M, Cavallari A. Hepatic resection for primary or secondary malignancies with involvement of the inferior vena cava: is this operation safe or hazardous? J Am Coll Surg 2005;201:671–679.
Venook A. Critical evaluation of current treatments in metastatic colorectal cancer. Oncologist 2005;10:250–261.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abdalla, E.K., Ribero, D., Pawlik, T.M. et al. Resection of Hepatic Colorectal Metastases Involving the Caudate Lobe: Perioperative Outcome and Survival. J Gastrointest Surg 11, 66–72 (2007). https://doi.org/10.1007/s11605-006-0045-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-006-0045-3