Abstract
Triplet repeat diseases (TRDs) refer to a group of diseases caused by three nucleotide repeats elongated beyond a pathologic threshold. TRDs are divided into the following four groups depending on the pathomechanisms, although the pathomechanisms of several diseases remain unelucidated: polyglutamine disorders, caused by a pathologic repeat expansion of CAG (coding the amino acid glutamine) located within the exon; loss-of-function repeat disorders, characterized by the common feature of a loss of function of the gene within which they occur; RNA gain-of-function disorders, involving the production of a toxic RNA species; and polyalanine disorders, caused by a pathologic repeat expansion of GCN (coding the amino acid alanine) located within the exon. Many of these TRDs manifest through neurologic symptoms; moreover, neuroimaging, especially brain magnetic resonance imaging, plays a pivotal role in the detection of abnormalities, differentiation, and management of TRDs. In this article, we reviewed the clinical and neuroimaging features of TRDs. An early diagnosis of TRDs through clinical and imaging approaches is important and may contribute to appropriate medical intervention for patients and their families.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
More than half of the human genome consists of repetitive DNA sequences, a large number of which lie within genes and their regulatory regions [1]. There are over 1 million discrete loci for short tandem repeats (1–6 base pair motifs) in the human genome, accounting for approximately 3% of genomic DNA [2]. These repetitive DNAs of various lengths provide evolutionary plasticity to adapt to different environments in humans. However, when the repetition exceeds a pathologic threshold, the gene expression and/or function of the gene product is altered, resulting in undesired conditions.
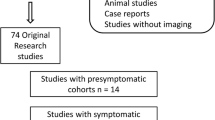
Triplet repeat diseases (TRDs) refer to a group of diseases caused by three nucleotide repeats elongated beyond a pathologic threshold [3]. In 1991, two different research groups successively discovered a CAG expansion in the exon of the androgen receptor gene in X-linked spinal and bulbar muscular atrophy (SBMA) [4] and a CGG expansion in the 5’ untranslated region of the fragile X mental retardation 1 (FMR1) gene in fragile X syndrome (FXS) [5]. In 2019, three diseases (neuronal intranuclear inclusion disease [NIID], oculopharyngeal myopathy with leukoencephalopathy [OPML], and oculopharyngodistal myopathy-1 [OPDM1]) were newly recognized as TRDs [6], and now there are more than 20 TRDs with frequent abnormal neuroimaging findings. TRDs are divided into the following four groups, depending on the pathomechanisms, although the pathomechanisms of several diseases remain unelucidated [7]:
-
Polyglutamine (polyQ) disorders: all diseases of this group share the common feature of being caused by pathologic repeat expansion of CAG (coding the amino acid glutamine) located within the exon.
-
Loss-of-function repeat disorders: this group includes disorders with different combinations of nucleotide repeats in various gene locations, but shares the common feature of a loss of function of the gene within which they occur.
-
RNA gain-of-function disorders: all diseases of this group share the common feature of involvement in the production of a toxic RNA species.
-
Polyalanine (polyA) disorders: all diseases of this group share the common feature of being caused by pathologic repeat expansion of GCN (coding the amino acid alanine) located within the exon.
Many of these TRDs manifest through neurologic symptoms, and neuroimaging, especially brain magnetic resonance imaging (MRI), plays a pivotal role in the detection of abnormalities, differentiation, and management of TRDs. TRD diagnosis is often challenging without genetic testing, due to the unspecific imaging findings; moreover, various degrees of clinical and imaging overlaps exist between TRDs or non-TRDs. Nevertheless, some patients with TRDs present pathognomonic imaging features and/or clinical pictures. In this article, we reviewed the clinical and neuroimaging characteristics of TRDs.
PolyQ disorders
PolyQ disorders include the following diseases: Huntington disease, dentatorubural-pallidoluysian atrophy (DRPLA), spinocerebellar ataxia type 1 (SCA1), SCA2, SCA3/Machado-Joseph disease (MJD), SCA6, SCA7, SCA17, and SBMA. Although the pathogenetic mechanism of PolyQ disorders has not been fully understood, most evidence suggests that abnormally elongated CAG repeats generate mutant proteins with abnormally elongated polyglutamates, which cause neurotoxicity through an abnormal conformation and misfold [7, 8]. With the exception of X-linked SBMA, the inheritance pattern of PolyQ disorders is autosomal dominant, and many polyQ disorders display “anticipation”, which is defined as more enhanced disease severity in successive generations of patients with more elongated CAG repeats and earlier disease onset [9].
Huntington disease
Huntington disease is an autosomal dominant disorder involving motor, cognitive, and psychiatric disturbances. Huntington disease is caused by an abnormal expansion of CAG repeats (full-penetrance pathogenic repeat number [same hereafter]: ≥ 39) in the Huntingtin (HTT) gene on 4p16.3 [10]. The mean age of onset is between 35 and 44 years, although the juvenile form with an early onset of symptoms (< 20 years) accounts for 5–10% of cases. The prevalence of Huntington disease is 5.7 per 100,000 and 0.4 per 100,000 in the Caucasian and Asian populations, respectively [11]. The characteristic motor symptoms include choreatic movements, hypokinesia, akinesia, and rigidity [12]. Cognitive decline can be seen long before the motor symptoms, while it can also be mild in later stages. Moreover, psychiatric symptoms, such as depression, anxiety, and irritability, are frequently present. Anticipation occurs more commonly in the paternal transmission of the mutated allele, with mean intergenerational expansions of CAG repeats of + 7.3 and + 0.7 with paternal and maternal transmissions, respectively [13]. On MRI, Huntington disease is characterized by progressive striatal (pallidum, putamen, and caudate) atrophy with T2 hyperintensity, which is the largest and earliest change in the subcortex (Fig. 1) [14], and correlates with the age of onset, disease duration, and CAG repeat length [15]. Other MRI findings include cortical thinning, which progresses from posterior to anterior cortical regions [15]. Altered dopamine signaling is demonstrated by reduced striatal dopamine transporter (DAT) binding on positron emission tomography (PET)/single photon emission computed tomography (SPECT) [15]. Inherited diseases with bilateral caudate atrophy, such as neuroacanthocytosis, McLeod syndrome, and SCA17 are imaging differential diagnoses of Huntington disease [10].
A 24-year-old man with Huntington disease. T2-weighted axial image a, FLAIR axial image b, and FLAIR coronal image c show hyperintensity and atrophy of the bilateral caudate nuclei and putamima, and atrophy of the globi pallidi (arrows). Decreased DAT uptake with a specific binding ratio of 2.12 (right striatum) and 2.09 (left striatum) is observed on DaTscan (d)
DRPLA
DRPLA is an autosomal dominant disorder caused by an abnormal expansion of CAG repeats (48–93) in the Atrophin 1 (ATN1) gene on 12p13.31 [16]. The mean age of onset is 31.5 years, and the clinical manifestations vary depending on the age of onset. The prevalence of DRPLA is 0.2–0.7 per 100,000 in the Japanese population, whereas it is rare in other countries [17]. The characteristic manifestations include ataxia, progressive myoclonus epilepsy, seizures, and progressive intellectual deterioration in patients with disease onset before 20 years of age, while ataxia, choreoathetosis, dementia, and psychiatric disturbance are present in those with disease onset after 20 years of age [16]. On MRI, only cerebellar atrophy can be seen in the early stages; however, as the disease progresses, atrophy of the brainstem (particularly the pontine tegmentum) and cerebrum accompanies it. The age at MRI and CAG repeat length correlates with the atrophic changes [16]. Hyperintensity on fluid-attenuated inversion recovery (FLAIR) images is observed in the cerebral white matter, cerebellar white matter, thalamus, and brainstem, in a decreasing order (Fig. 2) [18]. FLAIR hyperintensity in the cerebellar paravermal area, which was initially reported as the characteristic sign in NIID and fragile X-associated tremor/ataxia syndrome (FXTAS) [19, 20], can also be present in DRPLA [18].
A 53-year-old man with DRPLA. FLAIR axial images show hyperintensity in the supratentorial white matter (a, arrows), pons (b, arrow), and cerebellar white matter (c, arrows). FLAIR hyperintensity in the paravermal area is observed (c, arrowhead). T1-weighted sagittal image shows atrophic brainstem (d)
SCA1
SCA1 is an autosomal dominant disorder caused by an abnormal expansion of CAG repeats (≥ 39) in the Ataxin 1 (ATXN1) gene on 6p22.3 [21]. The onset is typically in the third or fourth decade of life, and gait ataxia is the initial symptom in 88% of cases; moreover, all patients eventually display cerebellar dysfunction [21, 22]. In addition to gait ataxia and dysarthria, SCA1, SCA2, and SCA3/MJD share clinical manifestations such as pyramidal involvement, peripheral neuropathy, and intellectual impairment [23]. Given the variety of common symptoms and varying degrees of severity, it is often challenging to distinguish SCA1 from other hereditary spinocerebellar degenerations without known significant family history. Computed tomography (CT) and MRI show atrophy in the cerebellum and brainstem, as well as gray matter atrophy in the supratentorial cortex, putamen, and caudate (Fig. 3) [24]. The hot cross bun sign, composed by hyperintensity of the cerebellar white matter, middle cerebellar peduncles, and pons on T2-weighted imaging (T2WI), while sparing the pyramidal tracts and medial lemnisci, has been infrequently reported in SCA1 [25,26,27]. Cerebellar atrophy predominantly involves the sensorimotor lobules (V, VI, and VIII) and the high-order cognitive processing lobules (VI, crus II, VIIB, and VIIIA) during the early symptomatic phase [24].
A 48-year-old man with SCA1. FLAIR axial image a and FLAIR coronal image b show cerebellar atrophy including superior cerebellar peduncles (arrows) and a vertical hyperintense line reflecting pontine atrophy (an incomplete hot cross bun sign) (a, arrowhead). T1-weighted sagittal image shows an atrophy of the brainstem and cerebellum (c)
SCA2
SCA2 is an autosomal dominant disorder caused by an abnormal expansion of CAG repeats (≥ 33) in the Ataxin 2 (ATXN2) gene on 12q24.12 [23]. The age at onset is usually in the fourth decade, and gait ataxia is the initial symptom in 87% of cases [22]. In addition to cerebellar dysfunction, extrapyramidal signs such as bradykinesia, postural/resting tremor, and focal/segmental dystonia as well as reduced saccadic velocity are frequently observed in SCA2 [23, 28]. MRI shows cerebellar and brainstem atrophy. Hot cross bun sign can be observed in 25.7–29.4% of the patients with SCA2 (Fig. 4) [25, 29, 30]. Decreased striatal uptake of DAT tracers on PET/SPECT has been reported in symptomatic SCA2 with parkinsonism, consistent with nigrostriatal dysfunction secondary to substantia nigra degeneration [30]. Furthermore, signal loss on neuromelanin-sensitive MRI in the substantia nigra and locus ceruleus has been reported in SCA2, although its diagnostic performance for differentiation from other hereditary spinocerebellar degenerations remains unclear [31].
A 33-year-old woman with SCA2. T2-weighted axial image a and FLAIR coronal image b show severe cerebellar atrophy (arrows). The hot cross bun sign is also observed (a, white arrowhead). Decreased melanin deposition in the bilateral substantia nigra c and locus ceruleus d is present on neuromelanin images (black arrowheads)
SCA3/MJD
SCA3/MJD is an autosomal dominant disorder caused by an abnormal expansion of CAG repeats (≥ 45) in the Ataxin 3 (ATXN3) gene on 14q32.12 [32]. The mean age at onset is the middle 30 s, and gait ataxia is the initial symptom in 85% of cases [22]. Highly specific clinical features of SCA3/MJD include bulging eyes and action-induced facial and lingual fasciculations. The bulging eyes reflect upper eyelid retraction and are not due to eyeball protrusion as seen in thyroid ophthalmoplegia [33]. Atrophy has been reported on MRI over a wide range of regions, including the cerebral cortex, thalamus, basal ganglia, cerebellum, and brainstem (Fig. 5). However, atrophy is initially observed in the cerebellum and brainstem and eventually extends supratentorially [34]. Atrophy of the basal ganglia is observed in patients with long disease duration (> 10 years) [34]. The hot cross bun sign is present in 1.3% of patients [29]. Hyperintensity on proton density-weighted images of the internal segment of the globus pallidus can be a clue to differentiate SCA3/MJD from DRPLA, which shows hyperintensity in the external segment of the globus pallidus.
A 41-year-old man with SCA3/MJD. Proton-weighted axial images show hyperintensity bands in the bilateral medial segments of the globi pallidi (a, black arrowheads) and an incomplete hot cross bun sign (b, white arrowhead). T1-weighted sagittal image shows an atrophy of the brainstem and cerebellum (c)
SCA6
SCA6 is an autosomal dominant disorder caused by an abnormal expansion of CAG repeats (20–33) in the CACNA1A gene on 19p13.13 [35]. Anticipation has not been observed in SCA6 [35]. The mean age of onset is between 43 and 52 years, and gait ataxia is the initial symptom in 76% of cases [22]. The incidence of downbeat positioning nystagmus (84%) is much higher in SCA6 than in other forms of SCA [36]. Other diseases with CACNA1A gene mutation include episodic ataxia type 2 and familial hemiplegic migraine 1 (Fig. 6); some patients with SCA6 show clinical overlap with these diseases. MRI shows progressive cerebellar atrophy including the dentate nuclei (Fig. 6) [37]. Normal T2 hypointensity in the dentate nuclei may be absent in SCA6 [37]. The absent T2 hypointensity in the dentate nuclei in SCA6 may be attributable to the decreased iron deposition, as indicated by quantitative susceptibility mapping studies [38, 39].
A 64-year-old woman with SCA6 (a, b) and a 50-year-old woman with familial hemiplegic migraine type 1 (c). T2-weighted axial image shows the absence of T2 hypointensity in the bilateral dentate nuclei (a, white arrowheads). The hot cross bun sign is absent (a). Pure cerebellar atrophy is observed on T1-weighted sagittal images in both patients (b, c)
SCA7
SCA7 is an autosomal dominant disorder caused by an abnormal expansion of CAG repeats (≥ 34) in the Ataxin 7 (ATXN7) gene on 3p14.1 [40]. SCA7 is characterized by cerebellar ataxia with progressive vision impairment due to retinal degeneration. This combination of symptoms is pathognomonic for SCA7; however, because of the extremely excessive anticipation, affected pediatric patients may develop the symptoms before their parents or grandparents [40]. Furthermore, the genetic diagnosis of pediatric patients can be a pre-onset diagnosis for one of their parents. In addition to the retina, an abnormal aggregation of ATXN7 is found in the cerebral cortex, basal ganglia, thalamus, midbrain, pons, medulla oblongata, and cerebellum [41]. In infantile cases, which progress more rapidly and have a poorer prognosis, abnormal protein aggregation leading to cellular degeneration is not limited to neural tissues but also involves non-neural tissues, including the anterior pituitary lobe, stomach, pancreas, adrenal glands, kidneys, intestines, cardiovascular tissues, and skeletal muscles [41]. On MRI, atrophy of the cerebellum and pons, and T2 hyperintensity of the middle cerebellar peduncles is occasionally observed (Fig. 7) [42, 43]. The hot cross bun sign is rare in patients with SCA7 [29].
SCA17
SCA17, also known as Huntington disease-like 4 (HDL4), is an autosomal dominant disorder caused by an abnormal expansion of CAG repeats (41–66) in the TATA-binding protein (TBP) gene on 6q27 [44]. The mean age at onset is 34.6 years. Cerebellar ataxia and psychiatric symptoms are often the initial clinical manifestations of SCA17, followed by involuntary movements such as chorea and dystonia, parkinsonism, dementia, and pyramidal tract signs [44]. On MRI, atrophy of the cerebellum and caudate nucleus may be present, not only after disease onset, but also in pre-mutation carriers (Fig. 8) [45]. Significantly reduced glucose metabolism on 18F-FDG-PET in the caudate nucleus has been reported in symptomatic patients with SCA17 [45]. Differential diagnoses include autosomal dominant hereditary disorders with choreatic movements (i.e., Huntington disease, HDL1, HDL2, SCA1, SCA2, SCA3/MJD, DRPLA, neuroferritinopathy, and benign hereditary chorea) [23, 44].
SBMA
SBMA, also known as Kennedy’s disease, is an X-linked gradually progressive neuromuscular disorder caused by an abnormal expansion of CAG repeats (≥ 38) in the androgen receptor gene [46]. The mean age of onset is the mid-40 s, and the most common symptoms are weakness, tremor, and cramping [46]. SBMA is characterized by androgen insensitivity including sexual dysfunction, gynecomastia, and testicular atrophy, which may be apparent before motor involvement. Furthermore, bulbar manifestations, including dysarthria, nasal speech, and tongue atrophy, can present early in the disease course. Unlike amyotrophic lateral sclerosis, which most often mimics SBMA, upper motor neuron signs are usually absent [46]. Skeletal MRI and CT show fat infiltration in bulbar and limb muscles (Fig. 9) [47]. Miyata et al. reported that facial nerve atrophy and a small cochlear nerve to facial nerve ratio could be observed in the early stage of SBMA [48].
Loss-of-function repeat disorders
Loss-of-function repeat disorders include the following diseases: FXS, fragile XE syndrome (FRAXE), and Friedreich’s ataxia (FRDA). Patients with these diseases have unstable triplet repeat expansions in non-protein-coding regions of genes; the expansion is in the 5’ untranslated region in FXS and FRAXE, whereas the expansion is in the first intron in FRDA [49]. The expanded repeat causes transcriptional silencing (loss-of-function) of the genes in these diseases [49].
FXS
FXS is an X-linked disorder caused by an abnormal expansion of CGG repeats (> 200) in the FMR1 gene on Xq27.3 [50]. The worldwide estimated prevalence of FXS is 1:5,000–7,000 males and 1:4,000–6,000 females; further, FXS is the second cause of intellectual disability after Down syndrome [51]. In FXS, severe and less severe intellectual disabilities are usually evident in males and females, respectively, with characteristic facial features such as large ears and elongated face, large testicles (boys), learning disabilities, and behavioral abnormalities (autism spectrum disorder and attention deficit/hyperactivity disorder) occurring frequently [50]. Other than facial, central nervous system (CNS), neuropsychiatric, musculoskeletal (e.g., joint laxity and flat feet), cardiovascular (e.g., mitral valve prolapse and aortic dilatation), and eye (e.g., refractive errors and strabismus) manifestations, as well as gastrointestinal reflux may occur [51]. Brain MRI shows caudate enlargement, which is specific for FXS in contrast to other neurodevelopmental disorders and can be observed within the first 3 years of life (Fig. 10) [52]. Other FMR1-related disorders include FXTAS and fragile X-associated primary ovarian insufficiency [50].
FRAXE
FRAXE is an X-linked disorder caused by an abnormal expansion of CCG repeats (> 250) in the fragile X mental retardation 2 gene on Xq28 [53]. The estimated prevalence of FRAXE is 1:50,000–100,000 males [54]. Affected patients show mild (intelligence quotient 50–70) to borderline (intelligence quotient 70–85) mental retardation associated with learning disability, communication deficits, attention problems, hyperactivity, and autistic behavior [53]. Physical features characteristic of FXS are absent in FRAXE [50]. Although characteristic neuroimaging features of FRAXE have not yet been established, no abnormal finding has been reported in several cases [55, 56].
FRDA
FRDA is an autosomal recessive disorder resulting from an abnormal expansion of GAA repeats (≥ 66) in the Frataxin (FXN) gene on 9q21.11 [57]. The prevalence of FRDA is 2–4:100,000 persons, and is the most common inherited ataxia in Europe, the Middle East, South Asia, and North Africa; nevertheless, FRDA has not been documented in Southeast Asians, sub-Saharan Africans, or Native Americans [57]. Typically, the disease onset occurs around puberty, and patients present with gait and limb ataxia, dysarthria, dysphagia, and scoliosis, and are wheelchair-bound by 10–15 years after onset. About two-thirds of the patients develop hypertrophic cardiomyopathy, and up to 30% have diabetes mellitus [57]. Neuropathological abnormalities occur predominantly in the dorsal root ganglia, dorsal horn of the spinal cord, cerebellar dentate nuclei, spinocerebellar tract, and corticospinal tract [58]. On MRI, atrophy is observed in the white matter of the midbrain, pons, medulla oblongata, and cerebellar peduncles, cerebellar lobules I–IV, and precentral gyrus (Fig. 11). Cases with early disease onset show an early degeneration of the cerebellar motor areas (lobules I–IV and VIIIb) and cerebellar peduncles [58]. The duration and severity of the disease correlate with atrophy of the dentate nucleus, brainstem, and superior and inferior cerebellar peduncles [58]. Differential diagnoses of FRDA include diseases involving pediatric cerebellar ataxia and dorsal funiculus degeneration, such as ataxia with vitamin E deficiency, abetalipoproteinemia, posterior column ataxia with retinitis pigmentosa, and ataxia-oculomotor apraxia type 1 [57, 59].
A 22-year-old man with Friedreich’s ataxia. T2-weighted axial image a and T1-weighted sagittal image b show atrophy of the cerebellum and brainstem (arrows). T2-weighted sagittal image shows diffuse spinal atrophy (c). T2-weighted axial image shows hyperintensity in the bilateral dorsolateral funiculi (d, arrowheads)
RNA gain-of-function disorders
RNA gain-of-function disorders include the following diseases: myotonic dystrophy type 1 (DM1) and FXTAS. Expanded CTG repeats in the 3’ non-coding region of the dystrophia myotonica-protein kinase (DMPK) gene in DM1 cause an aggregation of CUG transcripts, which interfere with the regulatory splicing activities of MBNL1 and CELF1 RNA-binding proteins, leading to a misregulation of the alternative splicing of several transcripts [60]. In FXTAS, 55–200 CGG repeats (compared with > 200 CGG repeats in FXS) in the 5’ untranslated region and increased expressions of the CGG-expanded transcripts are considered deleterious in neurons and glia, although the mechanisms have not been fully understood [49].
DM1
DM1 is an autosomal dominant muscular dystrophy caused by an abnormal expansion of CTG repeats (≥ 50) in the DMPK gene on 19q13.32 [61]. DM1 can be classified based on the following five phenotypes: congenital (onset at birth to 4 weeks of age), infantile (onset between 4 weeks and 10 years of age), juvenile (onset between 10 and 20 years of age), adult/classical (onset between 20 and 40 years of age), and late-onset/mild (onset > 40 years of age) [62]. Anticipation typically occurs in the maternal transmission of DM1, and the length of CTG repeats decreases from congenital to late-onset forms [61, 62]. Congenital DM1 occurs almost exclusively via maternal transmission, and is characterized by hypotonia, respiratory failure, facial dysmorphisms (e.g., tent-shaped upper lips and a carp mouth), and mental retardation [63]. Previous studies have suggested that infantile and juvenile forms should be considered as a CNS disease rather than a muscular or systemic disease [63]. Patients with infantile and juvenile DM1 mainly develop signs of CNS dysfunction, such as mental retardation, psychopathological manifestations, fatigue, and daytime somnolence; in contrast, muscle weakness most often remains mild or may be absent during childhood or adolescence [63]. The adult form is characterized by distal muscle weakness, myotonia, facial abnormalities (“hatchet” appearance), respiratory failure, cataracts, bolding, insulin insensitivity, and cardiac arrhythmia [64]. On MRI, atrophy of the cerebral cortex; ventricular enlargement; T2-weighted hyperintensity of the frontal, insular, and temporal pole white matter; and atrophy of the masticatory muscles have been reported mostly in adults (Fig. 12) [65]. However, some reports have suggested that hyperintensity near the triangular portion of the lateral ventricles on T2WI may be characteristic of congenital and infantile forms (Fig. 13) [66].
A 56-year-old man with DM1. T2-weighted axial images (a, b) show hyperintensity with atrophy in the white matter of the bilateral subcortical insular and temporal lobes (arrows). Subcortical white matter hyperintensity is also found in the bilateral temporal poles (b, white arrowheads). Part of the T2 hyperintensity areas shows cystic changes on FLAIR coronal image (c, black arrows). Severe atrophy of the bilateral temporalis and masseter muscles with fat replacement is observed on T1-weighted axial image (d, arrowheads)
An 11-year-old boy with congenital DM1. T2-weighted axial images (a–c) show hyperintensity in the white matter of the bilateral frontal lobes (a, white arrows), trigone of the bilateral temporal lobes (b, black arrows), and the bilateral temporal poles (c, white arrowheads). Atrophy of the bilateral temporalis muscles is observed (c, black arrowheads)
FXTAS
FXTAS is an X-linked disorder triggered by an abnormal expansion of CGG repeats (55–200) in the FMR1 gene on Xq27.3 [50]. The mean age at onset of tremor and/or ataxia in men is 61.6 years [67]. Clinically, FXTAS is characterized by cerebellar ataxia, intention tremor, parkinsonism, cognitive decline, and peripheral neuropathy [67]. The severity of tremors and ataxia strongly correlates with the length of CGG repeats. Parkinsonism is generally mild and the effect of dopaminergic medications is limited. On MRI, the middle cerebellar peduncles (MCP) show hyperintensity on T2WI (MCP sign) in approximately 60 and 13% of affected men and women, respectively (Fig. 14) [67]. Other imaging findings of FXTAS include moderate to severe brain atrophy and non-specific white matter lesions. Although the paravermal FLAIR hyperintensity (paravermal sign) was reported as a characteristic sign for NIID and FXTAS [18], this sign can be also found in DRPLA, as mentioned above [6, 62]. Imaging overlap also occurred with hyperintensity on diffusion-weighted imaging (DWI) along the corticomedullary junctions, which was initially considered pathognomonic for NIID, although it can also be found in FXTAS, OPML, and OPDM [6, 68]. Furthermore, evidence has been accumulating that genetic analysis is essential to differentiate FXTAS from NIID, due to both clinical and imaging overlaps as well as ubiquitin- and p62-positive intranuclear inclusions on skin biopsies in either disease[69,70,71].
A 79-year-old man with FXTAS. DWI shows hyperintensity bands along the corticomedullary junction (a, arrows). ADC map (b) and T2-weighted axial images (c) show diffuse white matter hyperintensity with atrophy. The middle cerebellar peduncle sign (d, white arrowheads) and hot cross bun sign (d, black arrow) are observed on T2-weighted axial image. FLAIR coronal images show the middle cerebellar peduncle sign (e, white arrowheads) and paravermal hyperintensity (f, black arrowheads)
PolyA disorders
PolyA disorders include the following diseases: cleidocranial dysplasia (CCD), holoprosencephaly type 5 (HPE5), oculopharyngeal muscular dystrophy (OPMD), ARX mutation-associated syndromes, blepharophimosis-ptosis-epicanthus inversus syndactyly, mental retardation with growth hormone deficiency, congenital central hypoventilation (Haddad syndrome), hand–foot–genital syndrome, and synpolydactyly [72]. Although the mechanism of polyA disorders remains unclear, it is considered to result from an unequal crossing between mispaired alleles and duplication during replication [73]. Unlike polyQ disorders, which generally exhibit neurological disorders with a wide range of phenotypes and repeat expansion lengths among patients, the polyalanine tract expansions in polyA disorders are generally smaller and more stable when transmitted between generations [73].
CCD
CCD is an autosomal dominant disorder resulting from an abnormal expansion of GCN repeats (20–27) in the RUNX2 gene on 6p21.1 [74]. CCD is characterized by the triad of delayed closure of the cranial sutures, hypoplastic or aplastic clavicles (Fig. 15), and dental abnormalities. Affected patients often have other skeletal problems including pes planus, genu valgum, scoliosis, and osteoporosis [74]. Intelligence is usually normal. On head and neck CT, wide open sutures, patent fontanelles, Wormian bones, arrested pneumatization of the paranasal sinuses, hypoplastic mid-facial region, relatively prognathic mandible, high-arched palate, and tooth abnormalities (impacted, crowned, and supernumerary) can be observed (Fig. 15) [74, 75].
HPE5
HPE5 is an autosomal dominant congenital disorder caused by an abnormal expansion of GCN repeats (16–25) in the ZIC2 gene on 13q32.3 [72]. The incidence of each type of holoprosencephaly in HPE5 is as follows: alobar (30%), semilobar (45%), lobar (15%), middle interhemispheric variants (8%), and microform (2%) [76]. Compared to other HPE types, patients with HPE5 have a more subtle common facial phenotype consisting of bitemporal narrowing, upslanting palpebral fissures, flat nasal bridge, short nose with anteverted nares, broad and deep philtrum, and a subjective appearance of large ears [77]. Other than holoprosencephaly, hydrocephalus and neural tube defects can be observed in 12% and 4% of patients with HPE5, respectively [77].
OPMD
OPMD is an autosomal dominant late-onset muscular dystrophy caused by an abnormal expansion of GCN repeats (12–17) in the PABPN1 gene on 14q11.2 [78]. The mean age at onset is 48 years; nevertheless, younger age at onset is often observed in patients with longer GCN expansions. OPMD is characterized by slowly progressive ptosis, dysphagia, and proximal limb muscle weakness. On CT and MRI, fatty replacements of the muscles are identified in almost all symptomatic patients, and the tongue, soleus muscle, and adductor magnus muscle are the most commonly involved sites (Fig. 16) [79]. Brain abnormalities may be absent in OPMD [6]. Diseases manifesting as myopathy, ptosis, and dysarthria/dysphagia (including OPDM, DM1, mitochondrial neurogastrointestinal encephalopathy disease, as well as vocal cord and pharyngeal dysfunction with distal myopathy) can be clinical differential diagnoses of OPMD [78].
A 76-year-old woman with OPMD. T1-weighted sagittal image a and coronal image b show fat infiltration of the tongue (arrows). No significant abnormal finding is found in the brain (c: FLAIR axial image). Atrophy of the bilateral extensor muscles in the lower extremities is observed on non-enhanced CT (d, e, arrowheads)
ARX mutation-associated syndromes
A high degree of phenotypic heterogeneity has been observed in patients with ARX mutation-associated syndromes, and these syndromes can be divided into those with and without brain malformations [80]. ARX mutation-associated syndromes with brain malformations include the following X-linked polyA diseases: infantile epileptic-dyskinetic encephalopathy, infantile spasms, and Partington syndrome [80].
ARX mutation-associated infantile epileptic-dyskinetic encephalopathy is characterized by severe mental retardation, early-onset infantile spasms, and severe generalized dystonia that has a progressive course in the first years of life before reaching a plateau [80]. An expansion of the first of the four polyA tracts is observed in this phenotype. Brain MRI shows multiple small foci with cerebrospinal fluid intensity within the posterior inferior regions of the basal ganglia, with mildly enlarged ventricles [80]. PolyA expansion is found in the second polyA tract in ARX mutation-associated infantile spasms and Partington syndrome (X-linked mental retardation, seizures, and mild distal dystonia), and these diseases have not been associated with brain abnormalities on neuroimaging examinations.
TRDs with unknown mechanisms
TRDs with unknown mechanisms include the following diseases: SCA8, SCA12, Huntington disease-like 2 (HDL2), NIID, OPML, and OPDM.
SCA8
SCA8 is an autosomal dominant disorder caused by an abnormal expansion of CTG/CAG repeats in the ATXN8 or ATXN8OS gene on 13q21 [81]. The typical age at disease onset is in the third to fifth decade. Patients with SCA8 exhibit slowly progressive cerebellar ataxia and a characteristic drawn-out slowness of speech. Because of low penetrance, it is sometimes challenging to diagnose SCA8 based on the family history. On MRI, global cerebellar atrophy is observed, whereas the brainstem is usually spared (Fig. 17) [82, 83]. However, the pathological significance of the increased number of triplet repeats in SCA8 has been questioned recently, given that an abnormal expansion of the triplet repeats in SCA8 has been observed in both normal controls and autopsy-confirmed multiple system atrophy [84, 85]. Roda et al. suggested that the ATXN8 or ATXN8OS gene should not be evaluated in isolation as a candidate gene for spinocerebellar degenerative disease [86].
SCA12
SCA12 is an autosomal dominant disorder triggered by an abnormal expansion of CAG repeats (51–78) in the PPP2R2B gene on 5q32 [87]. The mean age at onset is 34 years, and intention tremor is the most common initial presentation in SCA12. The manifestations are variable including mild cerebellar dysfunctions, tremor, gait dysfunction, pyramidal and extrapyramidal signs as well as cognitive and behavioral disturbances. MRI shows mild to moderate atrophy of the cerebellum (with vermis predominance) and cerebral cortex as well as ventriculomegaly with or without subcortical white matter changes [87]. Cerebellar atrophy (34.7%), cerebral atrophy (16.3%), or concurrent cerebral and cerebellar atrophy (34.7%) can be observed [88]. The brainstem usually shows no degenerative changes.
HDL2
HDL2 is an autosomal dominant disorder resulting from an abnormal expansion of CTG repeats (≥ 40) in the JPH3 gene on 16q24.2 [89, 90]. The mean age at onset is 41 years [91]. HDL2 is characterized by manifestations such as chorea, dementia, and oculomotor abnormalities; moreover, patients later exhibit a rigid and bradykinetic state with worsening dystonia [89]. Patients with HDL2 generally present with greater expression of a parkinsonism, less dysarthria, and relatively preserved oculomotor function compared to those with Huntington disease, although no significant difference in the incidence of chorea was reported between HDL2 and Huntington disease [89]. On MRI, atrophy of the caudate nuclei and putamina was frequently observed in HDL2, similar to Huntington disease [91]. Hyperintense putaminal rims on T2WI have been described in patients with HDL2 [92]. Anderson et al. reported that thalamic volume was significantly smaller in patients with HDL2 than in those with Huntington disease [93].
NIID
NIID, an autosomal dominant, slowly progressive neurodegenerative disorder, is caused by an abnormal expansion of CGG repeats (≥ 66) in the NOTCH2NLC gene on 1q21.2 [6, 90]. Traditionally, NIID has the following three forms, depending on the age of onset: infantile, juvenile, and adult forms; in addition, NIID can be divided into sporadic or familial forms [94]. However, it should be noted that CGG repeats in NOTCH2NLC gene have been mainly reported in adult patients in Japanese and Chinese descent. Sikora et al. reported that CGG repeats in NOTCH2NLC gene was rare in the European patients with NIID [95]. Furthermore, Jedlickova et al. reported that CGG repeats were not expanded and skin biopsy was negative in an infantile patient with NIID [96] Clinically, key phenotypic features of infantile-onset NIID include the following: although the early development is normal, the disease onset is abrupt and the progression is rapid; initial symptoms almost always involve unsteady gait associated with cerebellar dysfunction; and in the later stage, cerebellar decline, progressive pseudobulbar or bulbar palsy, peripheral neuropathy, hypotonia, and severe psychosocial regression are observed [97]. The most common causes of death in patients with NIID include respiratory infection and respiratory failure. Sporadic adult-onset NIID is almost always characterized by dementia (94.7%) and frequent autonomic impairment resulting in miosis and bladder dysfunction. In contrast, familial adult-onset NIID is characterized by muscle weakness (100%), followed by sensory disturbance, miosis, bladder dysfunction, and dementia [94].
On MRI, abnormal hyperintensity bands on DWI along the corticomedullary junction are characteristic of adult-onset NIID, although other diseases (i.e., FXTAS, OPML, and OPDM) may also demonstrate this sign (Fig. 18) [90, 91]; in addition, the frequency of this sign in infantile- and juvenile-onset NIID is unclear. The paravermal FLAIR hyperintensity (paravermal sign) is frequently observed in NIID [19]. It is worth noting that paravermal sign can appear before other imaging findings and be the only neuroimaging clue to NIID diagnosis [98,99,100]. The MCP sign can also be observed in NIID. Acute encephalopathy with cortical swelling, hyperintensity on T2WI, DWI, and apparent diffusion coefficient maps with contrast enhancement have been reported in adult-onset NIID, thereby mimicking mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes [101, 102]. In infantile-onset NIID, early-onset cerebellar atrophy is observed [97].
A 59-year-old woman with NIID. T2-weighted axial image shows hyperintensity in the white matter with atrophy (a, arrows). DWI shows hyperintensity bands along the corticomedullary junction (b, arrowheads). The paravermal FLAIR hyperintensity, which can be frequently observed in NIID, is not present in this case (not shown)
OPML
OPML is an autosomal dominant disorder caused by an abnormal expansion of CCG repeats in the LOC642361/NUTM2B-AS1 gene on 10q22.3 [6]. Given that OPML has only recently been reported, the available clinical and radiological information is limited. Frequent clinical findings of OPML include ptosis, restricted eye movements, dysphagia, dysarthria, and diffuse limb muscle weakness. On MRI, brain atrophy, T2 hyperintensity in the white matter, and DWI hyperintensity bands along the corticomedullary junction have been reported [92]. Furthermore, FLAIR hyperintensity in the paravermal area was observed in our case (Fig. 19).
A 60-year-old woman with OPML. T2-weighted axial image shows hyperintensity in the white matter with atrophy (a, white arrows). DWI shows hyperintensity bands along the corticomedullary junction (b, white arrowheads). FLAIR coronal image also shows paravermal hyperintensity (c, black arrowheads). Atrophy and fat infiltration of the bilateral masticator muscles are observed on T2-weighted axial image (d, black arrows). The same case with different MRI slides was evaluated in a prior study [6]
OPDM
OPDM is an autosomal dominant or autosomal recessive disorder caused by an abnormal expansion of CGG repeats in the LRP12, GIPC1, NOTCH2NLC, and RILPL1 genes on 8q22.3, 19p13.12, 1q21.2, and 12q24.31, respectively. The mean age at onset is 22 years [103]. OPDM is characterized by adult-onset ptosis, ophthalmoplegia, weakness of facial and distal limb muscles, dysphagia, and dysarthria. Muscle biopsy shows myopathic changes with rimmed vacuoles. Durmus et al. reported frequent early respiratory involvement while the patients were still ambulant in OPDM, which was considered atypical for other myopathies [103]. On MRI, patients with OPDM secondary to NOTCH2NLC gene mutation (a common causative genetic mutation in NIID) may show DWI hyperintensity bands along the corticomedullary junction and the MCP sign [68], whereas OPDM secondary to LRP12 gene mutation did not show any abnormal signal intensities or atrophic changes in the case presented by Ishiura et al. [93] as well as 32 case series by Kumutpongpanich et al. [104]
Conclusion
We reviewed the clinical and neuroimaging features of TRDs. Although therapies for TRDs mainly focused on alleviating symptoms, recent advances in genetic research offer hope for the development of curative therapies. The pre-onset prediction of TRD in at-risk individuals is also becoming possible. Therefore, an early diagnosis of TRDs through clinical and imaging approaches is important and may contribute to appropriate medical interventions for patients and their families.
References
Liang K-C, Tseng JT, Tsai S-J, Sun HS. Characterization and distribution of repetitive elements in association with genes in the human genome. Comput Biol Chem Elsevier BV. 2015;57:29–38.
Subramanian S, Mishra RK, Singh L. Genome-wide analysis of microsatellite repeats in humans: their abundance and density in specific genomic regions. Genome Biol. 2003;4:R13.
Paulson H. Repeat expansion diseases. Handb Clin Neurol. 2018;147:105–23.
La Spada AR, Wilson EM, Lubahn DB, Harding AE, Fischbeck KH. Androgen receptor gene mutations in X-linked spinal and bulbar muscular atrophy. NatureSpringer Sci Bus Media LLC. 1991;352:77–9.
Verkerk AJ, Pieretti M, Sutcliffe JS, Fu YH, Kuhl DP, Pizzuti A, et al. Identification of a gene (FMR-1) containing a CGG repeat coincident with a breakpoint cluster region exhibiting length variation in fragile X syndrome. Cell Elsevier BV. 1991;65:905–14.
Ishiura H, Shibata S, Yoshimura J, Suzuki Y, Qu W, Doi K, et al. Noncoding CGG repeat expansions in neuronal intranuclear inclusion disease, oculopharyngodistal myopathy and an overlapping disease. Nat Genet. 2019;51:1222–32.
Guyenet SJ, La Spada AR. Triplet repeat diseases. In Reviews in Cell Biology and Molecular Medicine, R.A. Meyers (Ed.). 2006.
Hannan AJ. Tandem repeats mediating genetic plasticity in health and disease. Nat Rev Genet. 2018;19:286–98.
Stoyas CA, La Spada AR. The CAG-polyglutamine repeat diseases: a clinical, molecular, genetic, and pathophysiologic nosology. Handb Clin Neurol. 2018;147:143–70.
Caron NS, Wright GEB, Hayden MR. Huntington Disease GeneReviews®. Seattle: University of Washington; 2020.
Pringsheim T, Wiltshire K, Day L, Dykeman J, Steeves T, Jette N. The incidence and prevalence of Huntington’s disease: a systematic review and meta-analysis. Mov Disord Wiley. 2012;27:1083–91.
Roos RAC. Huntington’s disease: a clinical review. Orphanet J Rare Dis Springer Nature. 2010;5:40.
Cannella M, Gellera C, Maglione V, Giallonardo P, Cislaghi G, Muglia M, et al. The gender effect in juvenile Huntington disease patients of Italian origin. Am J Med Genet B Neuropsychiatr Genet Wiley. 2004;125B:92–8.
Wijeratne PA, Garbarino S, Gregory S, Johnson EB, Scahill RI, Paulsen JS, et al. Revealing the timeline of structural MRI changes in premanifest to manifest Huntington disease. Neurol Genet. 2021;7: e617.
Niccolini F, Politis M. Neuroimaging in Huntington’s disease. World J Radiol. 2014;6:301–12.
Veneziano L, Frontali MDRPLA. GeneReviews®. Seattle: University of Washington; 2016.
Le Ber I, Camuzat A, Castelnovo G, Azulay J-P, Genton P, Gastaut J-L, et al. Prevalence of dentatorubral-pallidoluysian atrophy in a large series of white patients with cerebellar ataxia. Arch Neurol Am Med Assoc (AMA). 2003;60:1097–9.
Sugiyama A, Sato N, Kimura Y, Fujii H, Shigemoto Y, Suzuki F, et al. The cerebellar white matter lesions in dentatorubral-pallidoluysian atrophy. J Neurol Sci Elsevier BV. 2020;416:117040.
Sugiyama A, Sato N, Kimura Y, Maekawa T, Enokizono M, Saito Y, et al. MR imaging features of the cerebellum in adult-onset neuronal intranuclear inclusion disease: 8 cases. AJNR Am J Neuroradiol. 2017;38:2100–4.
Padilha IG, Nunes RH, Scortegagna FA, Pedroso JL, Marussi VH, Rodrigues Gonçalves MR, et al. MR imaging features of adult-onset neuronal intranuclear inclusion disease may be indistinguishable from fragile X–associated tremor/ataxia syndrome. AJNR Am J Neuroradiol Ame Soc Neuroradiol (ASNR). 2018;39:E100–1.
Opal P, Ashizawa T. Spinocerebellar Ataxia Type 1. GeneReviews®. Seattle: University of Washington; 2017.
Globas C, du Montcel ST, Baliko L, Boesch S, Depondt C, DiDonato S, et al. Early symptoms in spinocerebellar ataxia type 1, 2, 3, and 6. Mov Disord Wiley. 2008;23:2232–8.
Pulst SM. Spinocerebellar Ataxia Type 2. GeneReviews®. Seattle: University of Washington; 2019.
Nigri A, Sarro L, Mongelli A, Castaldo A, Porcu L, Pinardi C, et al. Spinocerebellar ataxia type 1: one-year longitudinal study to identify clinical and MRI measures of disease progression in patients and presymptomatic carriers. Cerebellum Springer Sci Bus Media LLC. 2022;21:133–44.
Chen H-C, Lee L-H, Lirng J-F, Soong B-W. Radiological hints for differentiation of cerebellar multiple system atrophy from spinocerebellar ataxia. Sci Rep. 2022;12:10499.
Wang Y, Koh K, Takaki R, Shindo K, Takiyama Y. Hot cross bun sign in a late-onset SCA1 patient. Neurol Sci Springer Nature. 2016;37:1873–4.
Namekawa M, Honda J, Shimazaki H. “Hot cross bun” sign associated with SCA1. Intern Med Jpn Soc Intern Med. 2015;54:859–60.
Jhunjhunwala K, Netravathi M, Purushottam M, Jain S, Pal PK. Profile of extrapyramidal manifestations in 85 patients with spinocerebellar ataxia type 1, 2 and 3. J Clin Neurosci Elsevier BV. 2014;21:1002–6.
Lee Y-C, Liu C-S, Wu H-M, Wang P-S, Chang M-H, Soong B-W. The, “hot cross bun” sign in the patients with spinocerebellar ataxia. Eur J Neurol Wiley. 2009;16:513–6.
Mascalchi M, Vella A. Neuroimaging biomarkers in SCA2 gene carriers. Int J Mol Sci MDPI AG. 2020;21:1020.
Nakamura K, Sugaya K. Neuromelanin-sensitive magnetic resonance imaging: a promising technique for depicting tissue characteristics containing neuromelanin. Neural Regen Res Medknow. 2014;9:759–60.
Paulson H, Shakkottai V. Spinocerebellar Ataxia Type 3. GeneReviews®. Seattle: University of Washington; 2020.
Moro A, Munhoz RP, Arruda WO, Raskin S, Teive HAG. Clinical relevance of “bulging eyes” for the differential diagnosis of spinocerebellar ataxias. Arq Neuropsiquiatr FapUNIFESP (SciELO). 2013;71:428–30.
Wan N, Chen Z, Wan L, Tang B, Jiang H. MR imaging of SCA3/MJD. Front Neurosci Front Media SA. 2020;14:749.
Casey HL, Gomez CM. Spinocerebellar Ataxia Type 6. GeneReviews®. Seattle: University of Washington; 2019.
Yabe I, Sasaki H, Takeichi N, Takei A, Hamada T, Fukushima K, et al. Positional vertigo and macroscopic downbeat positioning nystagmus in spinocerebellar ataxia type 6 (SCA6). J Neurol Springer Sci Bus Media LLC. 2003;250:440–3.
Stefanescu MR, Dohnalek M, Maderwald S, Thürling M, Minnerop M, Beck A, et al. Structural and functional MRI abnormalities of cerebellar cortex and nuclei in SCA3, SCA6 and Friedreich’s ataxia. Brain. 2015;138:1182–97.
Sugiyama A, Sato N, Kimura Y, Fujii H, Maikusa N, Shigemoto Y, et al. Quantifying iron deposition in the cerebellar subtype of multiple system atrophy and spinocerebellar ataxia type 6 by quantitative susceptibility mapping. J Neurol Sci Elsevier BV. 2019;407:116525.
Deistung A, Jäschke D, Draganova R, Pfaffenrot V, Hulst T, Steiner KM, et al. Quantitative susceptibility mapping reveals alterations of dentate nuclei in common types of degenerative cerebellar ataxias. Brain Commun Oxford University Press (OUP). 2022;4:fcab306.
La Spada AR. Spinocerebellar Ataxia Type 7. GeneReviews®. Seattle: University of Washington; 2020.
Seidel K, Siswanto S, Brunt ERP, den Dunnen W, Korf H-W, Rüb U. Brain pathology of spinocerebellar ataxias. Acta Neuropathol Springer Sci Bus Media LLC. 2012;124:1–21.
Kim M, Ahn JH, Mun JK, Choi EH, Kim JS, Youn J, et al. Extracerebellar signs and symptoms in 117 Korean patients with early-stage spinocerebellar Ataxia. J Clin Neurol Korean Neurological Association. 2021;17:242–8.
Yoshida S, Kikuchi A, Tateyama M, Aoki M. T2-hyperintensity of the middle cerebellar peduncles in a patient with SCA7. Intern Med. Jap Soc Inter Med. 2013;52:1433–4.
Toyoshima Y, Onodera O, Yamada M, Tsuji S, Takahashi H. Spinocerebellar Ataxia Type 17. GeneReviews®. Seattle: University of Washington; 2019.
Brockmann K, Reimold M, Globas C, Hauser TK, Walter U, Machulla H-J, et al. PET and MRI reveal early evidence of neurodegeneration in spinocerebellar ataxia type 17. J Nucl Med Soc Nucl Med. 2012;53:1074–80.
Grunseich C, Fischbeck KH. Spinal and bulbar muscular atrophy. Neurol Clin. 2015;33:847–54.
Klickovic U, Zampedri L, Sinclair CDJ, Wastling SJ, Trimmel K, Howard RS, et al. Skeletal muscle MRI differentiates SBMA and ALS and correlates with disease severity. Neurol Ovid Technol (Wolters Kluwer Health). 2019;93:e895-907.
Miyata M, Kakeda S, Hashimoto T, Korogi Y, Adachi H. The facial nerve atrophy with spinal and bulbar muscular atrophy patients (SBMA): Three case reports with 3D fast imaging employing steady-state acquisition (FIESTA). J Neurol Sci Elsevier BV. 2019;406:116461.
Nakamori M, Thornton C. Epigenetic changes and non-coding expanded repeats. Neurobiol Dis Elsevier BV. 2010;39:21–7.
Hunter JE, Berry-Kravis E, Hipp H, Todd PK. FMR1 Disorders. GeneReviews®. Seattle: University of Washington; 2019.
Ciaccio C, Fontana L, Milani D, Tabano S, Miozzo M, Esposito S. Fragile X syndrome: a review of clinical and molecular diagnoses. Ital J Pediatr. 2017;43:39.
Hagerman RJ, Berry-Kravis E, Hazlett HC, Bailey DB Jr, Moine H, Kooy RF, et al. Fragile X syndrome. Nat Rev Dis Primers. 2017;3:17065.
Gecz J. The FMR2 gene, FRAXE and non-specific X-linked mental retardation: clinical and molecular aspects. Ann Hum Genet. 2000;64:95–106.
Liu T, Wang FS, Cheah FSH, Gu Y, Shaw M, Law H-Y, et al. Simultaneous screening of the FRAXA and FRAXE loci for rapid detection of FMR1 CGG and/or AFF2 CCG repeat expansions by triplet-primed PCR. J Mol Diagn Elsevier BV. 2021;23:941–51.
Abrams MT, Doheny KF, Mazzocco MM, Knight SJ, Baumgardner TL, Freund LS, et al. Cognitive, behavioral, and neuroanatomical assessment of two unrelated male children expressing FRAXE. Am J Med Genet Wiley. 1997;74:73–81.
Sahoo T, Theisen A, Marble M, Tervo R, Rosenfeld JA, Torchia BS, et al. Microdeletion of Xq28 involving the AFF2 (FMR2) gene in two unrelated males with developmental delay. Am J Med Genet A Wiley. 2011;155A:3110–5.
Bidichandani SI, Delatycki MB. Friedreich Ataxia. GeneReviews®. Seattle: University of Washington; 2017.
Harding IH, Chopra S, Arrigoni F, Boesch S, Brunetti A, Cocozza S, et al. Brain structure and degeneration staging in friedreich ataxia: Magnetic resonance imaging volumetrics from the ENIGMA-ataxia working group. Ann Neurol Wiley. 2021;90:570–83.
Vedolin L, Gonzalez G, Souza CF, Lourenço C, Barkovich AJ. Inherited cerebellar ataxia in childhood: a pattern-recognition approach using brain MRI. AJNR Am J Neuroradiol Am Soc Neuroradiol (ASNR). 2013;34(925–34):S1-2.
Klein AF, Gasnier E, Furling D. Gain of RNA function in pathological cases: Focus on myotonic dystrophy. Biochimie Elsevier BV. 2011;93:2006–12.
Bird TD. Myotonic Dystrophy Type 1. GeneReviews®. Seattle: University of Washington; 2021.
De Antonio M, Dogan C, Hamroun D, Mati M, Zerrouki S, Eymard B, et al. Unravelling the myotonic dystrophy type 1 clinical spectrum: a systematic registry-based study with implications for disease classification. Rev Neurol (Paris) Elsevier BV. 2016;172:572–80.
Echenne B, Bassez G. Congenital and infantile myotonic dystrophy. Handb Clin Neurol. 2013;113:1387–93.
Turner C, Hilton-Jones D. The myotonic dystrophies: diagnosis and management. J Neurol Neurosurg Psychiatry BMJ. 2010;81:358–67.
Romeo V, Pegoraro E, Ferrati C, Squarzanti F, Sorarù G, Palmieri A, et al. Brain involvement in myotonic dystrophies: neuroimaging and neuropsychological comparative study in DM1 and DM2. J Neurol Springer Sci Bus Media LLC. 2010;257:1246–55.
Kuo H-C, Hsiao K-M, Chen C-J, Hsieh Y-C, Huang C-C. Brain magnetic resonance image changes in a family with congenital and classic myotonic dystrophy. Brain Dev Elsevier BV. 2005;27:291–6.
Leehey MA. Fragile X-associated tremor/ataxia syndrome: clinical phenotype, diagnosis, and treatment. J Investig Med. 2009;57:830–6.
Ogasawara M, Iida A, Kumutpongpanich T, Ozaki A, Oya Y, Konishi H, et al. CGG expansion in NOTCH2NLC is associated with oculopharyngodistal myopathy with neurological manifestations. Acta Neuropathol Commun Springer Sci Bus Media LLC. 2020;8:204.
Iwahashi CK, Yasui DH, An H-J, Greco CM, Tassone F, Nannen K, et al. Protein composition of the intranuclear inclusions of FXTAS. Brain Oxford University Press (OUP). 2006;129:256–71.
Ma L, Herren AW, Espinal G, Randol J, McLaughlin B, Martinez-Cerdeño V, et al. Composition of the intranuclear inclusions of fragile X-associated tremor/ataxia syndrome. Acta Neuropathol Commun Springer Sci Bus Media LLC. 2019;7:143.
Toko M, Ohshita T, Kurashige T, Morino H, Kume K, Yamashita H, et al. FXTAS is difficult to differentiate from neuronal intranuclear inclusion disease through skin biopsy: a case report. BMC Neurol Springer Sci Bus Media LLC. 2021;21:396.
Albrecht A, Mundlos S. The other trinucleotide repeat: polyalanine expansion disorders. Curr Opin Genet Dev Elsevier BV. 2005;15:285–93.
Chintalaphani SR, Pineda SS, Deveson IW, Kumar KR. An update on the neurological short tandem repeat expansion disorders and the emergence of long-read sequencing diagnostics. Acta Neuropathol Commun Springer Sci Bus Media LLC. 2021;9:98.
Machol K, Mendoza-Londono R, Lee B. Cleidocranial Dysplasia Spectrum Disorder. GeneReviews®. Seattle: University of Washington; 2017.
Patil PP, Barpande SR, Bhavthankar JD, Humbe JG. Cleidocranial dysplasia: a clinico-radiographic spectrum with differential diagnosis. J Orthop Case Rep. 2015;5:21–4.
Mercier S, Dubourg C, Garcelon N, Campillo-Gimenez B, Gicquel I, Belleguic M, et al. New findings for phenotype-genotype correlations in a large European series of holoprosencephaly cases. J Med Genet BMJ. 2011;48:752–60.
Solomon BD, Lacbawan F, Mercier S, Clegg NJ, Delgado MR, Rosenbaum K, et al. Mutations in ZIC2 in human holoprosencephaly: description of a novel ZIC2 specific phenotype and comprehensive analysis of 157 individuals. J Med Genet BMJ. 2010;47:513–24.
Trollet C, Boulinguiez A, Roth F, Stojkovic T, Butler-Browne G, Evangelista T, et al. Oculopharyngeal Muscular Dystrophy. GeneReviews®. Seattle: University of Washington; 2020.
Alonso-Jimenez A, Kroon RHMJM, Alejaldre-Monforte A, Nuñez-Peralta C, Horlings CGC, van Engelen BGM, et al. Muscle MRI in a large cohort of patients with oculopharyngeal muscular dystrophy. J Neurol Neurosurg Psychiatry BMJ. 2019;90:576–85.
Guerrini R, Moro F, Kato M, Barkovich AJ, Shiihara T, McShane MA, et al. Expansion of the first PolyA tract of ARX causes infantile spasms and status dystonicus. Neurol Ovid Technol (Wolters Kluwer Health). 2007;69:427–33.
Cleary JD, Subramony SH, Ranum LPW. Spinocerebellar Ataxia Type 8. GeneReviews®. Seattle: University of Washington; 2021.
Tazón B, Badenas C, Jiménez L, Muñoz E, Milà M. SCA8 in the Spanish population including one homozygous patient. Clin Genet Wiley. 2002;62:404–9.
Zeman A, Stone J, Porteous M, Burns E, Barron L, Warner J. Spinocerebellar ataxia type 8 in Scotland: genetic and clinical features in seven unrelated cases and a review of published reports. J Neurol Neurosurg Psychiatry BMJ. 2004;75:459–65.
Torrens L, Burns E, Stone J, Graham C, Wright H, Summers D, et al. Spinocerebellar ataxia type 8 in Scotland: frequency, neurological, neuropsychological and neuropsychiatric findings. Acta Neurol Scand Wiley. 2008;117:41–8.
Factor SA, Qian J, Lava NS, Hubbard JD, Payami H. False-positive SCA8 gene test in a patient with pathologically proven multiple system atrophy. Ann Neurol Wiley. 2005;57:462–3.
Roda RH, Schindler AB, Blackstone C. SCA8 should not be tested in isolation for ataxia. Neurol Genet Ovid Technologies (Wolters Kluwer Health). 2017;3:e150.
Srivastava A, Kumar D, Faruq M, Gundluru V. Spinocerebellar ataxia type 12: an update. Ann Mov Disord Medknow. 2019;2:48.
Ganaraja VH, Holla VV, Stezin A, Kamble N, Yadav R, Purushottam M, et al. Clinical, radiological, and genetic profile of spinocerebellar ataxia 12: a hospital-based cohort analysis. Tremor Other Hyperkinet Mov (N Y). 2022;12:13.
Anderson DG, Ferreira-Correia A, Rodrigues FB, Aziz NA, Carr J, Wild EJ, et al. Comparison of the Huntington’s disease like 2 and Huntington’s disease clinical phenotypes. Mov Disord Clin Pract Wiley. 2019;6:302–11.
Wallace SE, Bean LJH. Table. [genetic Disorders Caused by Nucleotide Repeat Expansions and contractions]. Seattle: University of Washington; 2021.
Anderson DG, Walker RH, Connor M, Carr J, Margolis RL, Krause A. A systematic review of the Huntington disease-like 2 phenotype. J Huntingtons Dis IOS Press. 2017;6:37–46.
Schneider SA, Marshall KE, Xiao J, LeDoux MS. JPH3 repeat expansions cause a progressive akinetic-rigid syndrome with severe dementia and putaminal rim in a five-generation African-American family. Neurogenetics Springer Sci Bus Media LLC. 2012;13:133–40.
Anderson DG, Haagensen M, Ferreira-Correia A, Pierson R, Carr J, Krause A, et al. Emerging differences between Huntington’s disease-like 2 and Huntington’s disease: A comparison using MRI brain volumetry. NeuroImage Clin Elsevier BV. 2019;21:101666.
Sone J, Mori K, Inagaki T, Katsumata R, Takagi S, Yokoi S, et al. Clinicopathological features of adult-onset neuronal intranuclear inclusion disease. Brain. 2016;139:3170–86.
Chen Z, Yan Yau W, Jaunmuktane Z, Tucci A, Sivakumar P, Gagliano Taliun SA, et al. Neuronal intranuclear inclusion disease is genetically heterogeneous. Ann Clin Transl Neurol Wiley. 2020;7:1716–25.
Jedlickova I, Pristoupilova A, Hulkova H, Vrbacka A, Stranecky V, Hruba E, et al. NOTCH2NLC CGG repeats are not expanded and skin biopsy was negative in an infantile patient with neuronal intranuclear inclusion disease. J Neuropathol Exp Neurol Oxford University Press (OUP). 2020;79:1065–71.
Sikora J, Jedlickova I, Pristoupilova A, Stranecky V, Honzik T. Genetic heterogeneity of neuronal intranuclear inclusion disease: what about the infantile variant? Ann Clin Transl Neurol. 2021;8:994–1001.
Tokimura R, Hashimoto Maeda M, Mitsutake A, Sakai S, Suzuki F, Sugasawa K, et al. Isolated paravermal hyperintensities in neuronal intranuclear inclusion disease. Neurolo Ovid Technol (Wolters Kluwer Health). 2022;98:938–9.
Sugiyama A, Takeda T, Koide M, Yokota H, Mukai H, Kitayama Y, et al. Coexistence of neuronal intranuclear inclusion disease and amyotrophic lateral sclerosis: an autopsy case. BMC Neurol Springer Sci Bus Media LLC. 2021;21:273.
Okamura S, Takahashi M, Abe K, Inaba A, Sone J, Orimo S. A case of neuronal intranuclear inclusion disease with recurrent vomiting and without apparent DWI abnormality for the first seven years. Heliyon Elsevier BV. 2020;6:e04675.
Liang H, Wang B, Li Q, Deng J, Wang L, Wang H, et al. Clinical and pathological features in adult-onset NIID patients with cortical enhancement. J Neurol Springer Sci Bus Media LLC. 2020;267:3187–98.
Ishihara T, Okamoto T, Saida K, Saitoh Y, Oda S, Sano T, et al. Neuronal intranuclear inclusion disease presenting with an MELAS-like episode in chronic polyneuropathy. Neurol Genet. 2020;6:e531.
Durmus H, Laval SH, Deymeer F, Parman Y, Kiyan E, Gokyigiti M, et al. Oculopharyngodistal myopathy is a distinct entity: clinical and genetic features of 47 patients. Neurology. 2011;76:227–35.
Kumutpongpanich T, Ogasawara M, Ozaki A, Ishiura H, Tsuji S, Minami N, et al. Clinicopathologic features of oculopharyngodistal myopathy with LRP12 CGG repeat expansions compared with other oculopharyngodistal myopathy subtypes. JAMA Neurol Am Med Assoc (AMA). 2021;78:853–63.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception. RK: wrote the original manuscript. MK, AM, MK, AB, YN, TM, and OA: edited the manuscript. RK, MK, and AM: conceptualized this study. RK, AM, MN, YN, and TM: collected the data. TM and OA: supervised. OA: validated this study. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kurokawa, R., Kurokawa, M., Mitsutake, A. et al. Clinical and neuroimaging review of triplet repeat diseases. Jpn J Radiol 41, 115–130 (2023). https://doi.org/10.1007/s11604-022-01343-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-022-01343-5