Abstract
The objective of this work was to summarise and evaluate the evidence showing that physical activity is a protector factor as regards falls in older people. Relevant studies were identified through a systematic search in the MEDLINE and Cochrane Library, under the keywords of accidental fall/numerical data and risk factors, and with the bibliographies of retrieved papers. The combined odds ratio (OR) [95% confidence interval] for physical activity was 0.75 [0.64, 0.88] with moderate heterogeneity (I 2 = 33%). For fall injury, it was 0.59 [0.47, 0.74] and, for falls in general, it rose to 0.94 [0.76, 1.17] with nil heterogeneity. The combined OR for sedentary factors was 1.14 [1.10, 1.82] with moderate heterogeneity (I 2 = 36%). Regular physical activity in daily life yields significant reduction in falls in older people, especially falls with injuries.
Similar content being viewed by others
Introduction
A fall is defined as an event in which the participant unintentionally comes to rest on the ground or at a lower level [1]. Falls have become a major public health problem for industrialised countries with an ageing population [2, 3]. Several studies [4, 5] have estimated that one third of the population over 65 years and one half of people over 85 years of age experience one or more falls per year. Fall consequences may be traumatic, psychological, economic and/or social. Accidental falls are the first cause of accidental death in this age range [6], and when they do not result in death, they constitute one of the main causes of invalidity and are often synonymous with loss of autonomy and institutionalisation.
It is well-known that the aetiology of falling is multifactorial and those falls risk factors are quite numerous. Many studies [7–18] have attempted to determine the risk factors and their relative impact on actual falls. A combination of these risk factors has led to predicting the degree of risk of falls in older people. Among them, potential protective factors such as physical activity and detrimental factors such as sedentary behaviour recurrently appear. Therefore, prevention and rehabilitation programmes should take these modifiable factors into consideration and thereby help to reduce the magnitude of fall risk.
Meta-analyses on drugs [19–23], muscle weakness [24], balance impairment [25], sociodemographic items [26] and fall risk in older persons have all been carried out. That said, the only meta-analysis performed on exercises aimed at preventing falls is quite recent and dealt only with randomised controlled trials (RCTs) [27]. The main conclusion was that an exercise programme can reduce fall rates in older people with a pooled estimate rate ratio (RR) of 0.83 [0.75, 0.91]. So far, no meta-analyses have been performed on sedentary behaviour. Meta-analysis restricted to RCTs is usually preferred to meta-analysis of observational studies [28] because it provides the most accurate and non-biased results, the least likely to be contested by potential confounders [29]. Nevertheless, for practical and ethical reasons (e.g. imposed sedentary behaviour), RCTs are generally not feasible and observational studies have been largely preferred. Follow-up studies of older people have been organised in which their living habits, including physical activity, have been documented. Despite the problems with observational studies, meta-analyses can help to draw out some generalisations and conclusions and are, therefore, necessary in order to compare their conclusions with those from meta-analysis of RCTs.
The purpose of this study is to synthesise the findings of published observational studies and to determine whether physical activity and sedentary behaviour can modify fall risks in persons over 60 years. The procedures consist of (1) performing a meta-analysis to estimate the degree of statistical association between physical activity and falls and between sedentary behaviour and falls and (2) exploring the sources of heterogeneity.
Methods
Literature search strategy
The original articles published from 1966 through 2007 in English and French were identified through a systematic search on the biomedical electronic base MEDLINE and the Cochrane Library. During this first step, the key words in the thesaurus were ‘accidental fall/numerical data’ and ‘risk factors’. The second step consisted of a manual search for the articles cited within the previously identified publications.
Study inclusion criteria
Two readers independently selected and reviewed all the abstracts of articles derived from the electronic search.
-
Study inclusion criteria:
-
Participants were aged 60 years and more, either living in their own homes, institutionalised or hospitalised;
-
‘Falls’ were in daily life, including any fall, recurrent falls and injurious falls;
-
All the different types of studies, whether observational or interventional, were taken into consideration.
-
-
First step of exclusion criteria:
-
Participants were aged under 60 years;
-
Accidental falls in road accident, falls from ladders, scaffolding and cliffs;
-
Samples involving a cohort suffering from serious neuromuscular disease or specific disease (e.g. osteoporosis, Parkinson’s disease, dementia);
-
Letters to the editor, commentaries, editorials and meta-analysis were not considered.
-
-
Second step of exclusion criteria:
-
Excluding all studies not considering sedentary behaviour and physical activity;
-
Excluding interventional studies.
-
To avoid duplication of data when the same group of aged persons was investigated in several publications, only the study reporting the most recent data was retained. Disagreements on study inclusion were settled subsequent to discussion with a third party.
Data extraction and study characteristics
Each reader gathered information on half of the studies. Data from a quarter of them were independently extracted by each of the two readers in order to evaluate the degree of inter-reader concordance. Discordances were resolved by consensus. Few extraction mistakes (6.4%) were observed, and double extraction on all studies did not prove necessary.
The following data were gathered:
-
Name of the first author
-
Date and journal of publication, impact factor 2007 of the journal
-
Schema of study: exposed or non-exposed cohort, case–control or cross-sectional
-
Number of subjects
-
Number of fallers
-
For observational cohort studies: prospective or retrospective collection, consecutive series, random sampling
-
For observational case–control studies: cases and controls derived from a comparably sourced population, matched or random sampling
-
For cross-sectional studies: consecutive recruitment or random sampling
Demographics
Definition of the population included minimum and maximum age, mean and standard deviation.
Evaluation criteria
-
Definition of the fall: an isolated incident, more than a single fall, duration and collection of the ‘falling’ event
-
Definition of risk factors and categories among the following: iatrogenic, medical histories, extrinsic, physical and sociodemographic
-
For quantitative variables:
-
Number of fallers with risk factor for falls
-
Number of fallers without risk factor for falls
-
Number of non-fallers with risk factor for falls
-
Number of non-fallers without risk factor for falls
-
-
For qualitative variables:
-
Mean and standard deviation in the group of fallers
-
Mean and standard deviation in the group of non-fallers
-
-
Order of data gathering on the risk factor(s) with regard to falls: risk factor for falls evaluated before a fall, at time of fall or after a fall
Methodological quality assessment
Two readers assessed the quality of each study included according to a validated scale [30] derived from the recommendations of Cook in 1992 [31]. This scale provides a level of proof in accordance with the methodology, study power, randomisation, population, data collection and biases. Level 1 of proof coding in #1 is synonymous with established scientific proof, level 2 coding in #2 denotes scientific assumption and levels 3 and 4 coding in #3 and #4 refer to a low degree of scientific proof.
Statistical analysis
The quantitative variables are expressed by the mean, standard deviation, median and extreme values. The qualitative variables are described in terms of the number of individuals and the corresponding percentages. The analyses were carried out with SAS software, version 9.1 (SAS Inc., Cary, NC, USA).
Two meta-analyses were completed, one on physical activity and one on sedentary behaviour. Outcomes were analysed using fixed-effect models. The degree of effect of physical activity and sedentary behaviour on falls risk was measured with the odds ratio (OR) with a 95% confidence interval (CI). Fixed-effect meta-analysis was conducted through the Mantel–Haenszel method [32].
Heterogeneities between studies’ results were assessed with standard methods, in particular the chi-square test [33] and the I 2 statistic [34]. A value of I 2 <25% led to the conclusion that heterogeneity might be low, between 25% and 50% that it was moderate and 50% to 75% that it was high [34]. In case of moderate or high heterogeneity, estimation of level of proof was conducted. Sources of heterogeneity were also examined (samples, intervention, judgement criteria). Stratified analysis on these sources and sensitivity analysis in function of methodological quality were carried out. We also used Begg’s funnel plots [35, 36] to detect possible publication bias.
All meta-analyses were conducted with Review Manager 5 (RevMan), version 5.0.14. We defined a statistical test with a p value lower than 0.05 as significant.
Results
Study selection
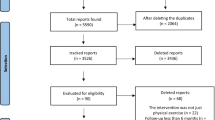
The computerised search allowed our team to identify 3,747 indexed articles published from 1966 through 2007 (Fig. 1). Two thousand and six did not meet the inclusion criteria, and 1,222 did not deal with risk factors for falls (e.g. consequences of the fall, prevention of falls). Thirteen meta-analyses, 142 overviews of the literature, 34 letters, 6 editorials, 2 commentaries, 4 reports, 1 scientific correspondence and 10 doublets were likewise eliminated from consideration, thereby leaving only 307 original articles. Using a manual search, 36 references were added. At the end of the initial selection step, only 343 studies had consequently been chosen for further consideration. Due to missing information (e.g. absence of number of fallers/non-fallers with or without risk factors, absence of standard deviation), the final analysis included only 177 articles. Among them, 17 studies presented data concerning physical activity (Table 1) and 8 pertained to sedentary behaviour (Table 2).
Study characteristics
Physical activity
The 17 studies concerning physical activity (Table 1) were published from 1988 to 2007. The median number of subjects was 387 (40–1,158). There were seven cross-sectional studies (41%), two case–control studies (12%) and eight cohort studies (47%), of which one was retrospective. Seven studies (41%) were at level 2, two studies (12%) were rated at level 3, while eight (47%) were of insufficient level of proof (#4). Fourteen studies included both men and women and 3 were limited to women.
Sedentary factors
The eight studies concerning sedentary factors (Table 2) were published from 1993 to 2006. The median number of subjects included was 541 [40–1,526]. The studies were all observational. Among them, there were four cross-sectional studies (50%), two case–control studies (25%) and only two cohort studies (25%). Two studies (25%) were at level 2, two studies (25%) were rated at level 3, while four (50%) were of insufficient level of proof (#4). Six studies included both men and women and two were limited to women.
Meta-analyses
Physical activity
Seventeen studies considered physical activity (Table 1); the OR was 0.71 [0.63, 0.80] with I 2 = 29% (χ 2 = 22.4, df = 16, p = 0.13) (Table 3). A sensitivity analysis was performed in function of methodological quality (Fig. 2); only nine studies with good or moderate quality were kept. The OR was 0.75 [0.64, 0.88] with I 2 = 33% (χ 2 = 11.91, df = 8, p = 0.16).
Stratified analyses (Table 3) were performed to calculate the OR in function of fall type. For any falls [9, 37–42], the OR was 0.94 [0.76, 1.17] and, for traumatic falls [43, 44], 0.59 [0.47, 0.74]. Follow-up on falls was generally performed over 12 months; only one study collected falls during a period <12 months [43] and one did not indicate period length [44]. The OR for the minimum 12-month follow-up was 0.94 [0.76, 1.17]. Stratified analysis on mean population age revealed an OR of 1.05 [0.80, 1.38] for the mean age of 60 to 80 years [9, 37, 40, 42] and an OR of 0.68 [0.51, 0.91] for subjects with a mean age over 80 years [38, 39, 41, 44].
Heterogeneity was moderate (27% to 33%) and became nil subsequent to subgroup analyses. An evaluation of the sources of heterogeneity was performed and, whatever the stratified analyses were, two studies [43, 44] remained separated from the others on account of judgement criteria (fall injury) or length of follow-up (<12 months), either or both of which might have caused this moderate heterogeneity.
The asymmetric funnel plot (Fig. 3) suggests publication bias. An empty surface appears in the left part of the graphic, signifying that negative small studies were not included in our systematic study or were not published.
Logistic regression model analyses were completed in 11 studies [9, 37, 38, 40, 42–48]. Among them, three carried out regression analysis with the data chosen and did not include exercises [37, 46, 48]. Some considered all risk factors that were associated with falls in the univariate analysis, i.e. variables revealing significant differences between the groups (non-fallers versus fallers). But frequently, physical activity was not a significant variable in the first analyses [9, 38, 40, 42, 45] and was not included in the logistic regression model. Nevertheless, two studies revealed a significant difference in univariate analysis and, therefore, considered exercises in their model [43, 44]; the adjusted OR obtained was 0.6 [0.4, 0.8] for Herndon et al. in 1997 and 0.49 [0.29, 0.83] for Peel et al. in 2006.
Sedentary factors
The OR, concerning sedentary factors and calculated with the results of the eight selected studies (Table 2), was 1.37 [1.14, 1.64] with I 2 = 66% (χ 2 = 20.57, df = 7, p = 0.004). Sensitivity analysis was carried out in order to separate good or moderate quality studies (#1–3) from poor quality studies (#4) (Fig. 4). The significant OR obtained were, respectively, 1.41 [1.10, 1.82] and 1.32 [1.03, 1.70] with I 2 = 36% (χ 2 = 4.72, df = 3, p = 0.19) and I 2 = 81% (χ 2 = 15.8, df = 3, p = 0.001).
Stratified analyses (Table 3) were also conducted in accordance with fall types. Fall collection was carried out during 12 months or more in three studies, and in one, it was <12 months [49]. The significant OR obtained for the follow-up of 12 months or more was 1.32 [1.01, 1.72]. No studies included populations living in institutions and none dealt with traumatic falls. The significant OR calculated with stratified analysis in function of mean age was 1.50 [1.12, 2.01] for a mean age between 60 and 80 years.
Heterogeneity was high prior to sensitivity analysis (66%), moderate (36%) for studies with good or moderate methodological quality and quite high (81%) for studies with poor methodological quality. After subgroup analyses, it diminished (0%) when length of follow-up was 12 months and more and increased (52%) when the mean age of population was 60 to 80 years.
As in our previous meta-analysis, the asymmetric funnel plot (Fig. 5) suggests publication bias. An empty surface appears in the left part of the graphic, meaning that negative small studies are not included in our systematic study or are not published.
When the authors completed logistic regression model [40] or multivariate analysis of fall risk [50], this factor was not considered or did not appear to be a significant risk factor for falls.
Discussion
This systematic review and meta-analysis indicates that physical activity constitutes a protector factor for falls in persons aged over 60 years. Physically active older adults are less at risk of falling (OR of 0.75 [95% CI of 0.64, 0.88]) than those who are physically inactive or sedentary (OR of 1.41 [95% CI of 1.10, 1.82]). These results were confirmed in stratified analysis, especially for fall injury, ambulatory people and people with a mean age over 80 years as regards meta-analysis of physical activity.
For physical activity, the main finding in our study is consistent with previous meta-analysis on RCTs [27], which provides strong evidence that exercise programmes can reduce fall rates in older people (RR of 0.83 [95% CI of 0.75, 0.91]). In previous meta-analysis, programmes including balance exercise were more effective in fall prevention than those including walking exercises. However, this result is peculiar since falls occur also in dynamic balance.
Surprisingly, when excluding articles dealing only with injurious falls, physical activity did not have any significant preventive effect. Therefore, physical exercise may protect less as regards number of falls than as regards degree of injury entailed; it is possible that those who have lower physical activity might have lower muscle mass and thus are more susceptible to injury when falling occurs. Similarly, no significant reduction of the number of fallers was found when the follow-up was 12 months or more. It may be doubtful that older people practise exercises all year, maintaining a sufficient degree of intensity, frequency and duration. It is also possible that this meta-analysis of observational study fails to precisely estimate the impact of physical activity on falls.
It was convincingly demonstrated and highlighted that exercise load is a highly important variable [27, 51]. Exercise programmes would be more effective if they would be more intense, with a high frequency (twice weekly) and especially if the length of the programme would exceed 25 weeks. Such length should be considered as the minimal amount of time necessary for physiological adaptations in older people. In all the studies included in our meta-analysis, the amount of physical activity was only globally estimated through questionnaires and no precise indication of exercise load was reported. The quality of the exercise descriptions in term of intensity, duration and type are not precise enough to perform a proper analysis. It was not known whether the subjects regularly practised physical activities and for how long they engaged in regular physical activity. The length of involvement could possibly exceed the 25 theoretical weeks and exercises actually performed in daily life (or not).
The finding that physical activity diminished the risk of falls in older people can be explained by changing or reducing other known risk factors. Exercises can heighten or maintain balance [52, 53], gait (e.g. walking speed [53], walking efficiency [54]), muscle strength [24] (e.g. ankle strengthening [53], physical strength [55]) and can also slow down physical deterioration in older people residing in nursing homes [53]. To develop an effective fall prevention or rehabilitation programme, it is essential to know the relative shares of the factors likely to prevent or reduce fall risks. In any event, physical activity is particularly low in older age groups but it can be of particular help in older people, and that is why sustained training has been highly recommended in fall prevention programmes [27, 55–57].
Sedentary behaviour has been reported to be a strong factor influencing the health of ageing subjects, and it is also likely to have an impact on the risk of falls. The OR for sedentary behaviour was not quite as high as we might have expected. Nevertheless, it is significant and as important as are other fall risk factors, such as drugs. The unadjusted OR estimated for nine medication classes [21] (i.e. antihypertensive agents, diuretics, β blockers, sedatives and hypnotics, neuroleptics and antipsychotics, antidepressants, benzodiazepines, narcotics, non-steroidal anti-inflammatory drugs) are all lower than 2, similar to our results concerning sedentary factors. For muscle weakness [24], especially lower extremity, the OR seems to be somewhat higher (1.76 [1.31, 2.37]). This is also the case with balance impairment [25], for which overall fall risk was calculated at 1.98 [1.60, 2.46]. The last two factors appear to increase the risk of a fall to a greater degree than medication, and they may be limited by sustained physical training.
This meta-analysis has shown certain limitations. First, our methodology excluded numerous studies on account of unavailable data because we needed to calculate the ORs using the same method for all participants. Second, like in most meta-analyses, publication bias was such that unpublished studies were not sought after. Thirdly, the difference between sedentary behaviour and physical activity could be not clear. Therefore, we experienced in some cases great difficulties to decide where to include some of published works whether in the table for ‘physical activity’ (Table 1) or in the table related to ‘sedentary behaviour’ studies (Table 2). For instance, under studies including physical activity (Table 1), one study [46] considered physical activity as ‘any walking, including walking the dog at least 10 times in the previous 12 months’. On the other hand, under limited activity (Table 2), we included one work [58] in which the subjects were ‘underactive’. Those are the reasons why relatively few studies are included in these two meta-analyses, and they also explain a limited but real publication bias.
In conclusion, physical activity practised by older people would be an indicator of a lower risk of fall, especially as regards injurious fall. However, we could not draw any cause–effect relationship. It is possible that people who are healthier and do not tend to fall choose to do physical activity and not the opposite. However, our results are similar to those found in RCT studies and our sedentary behaviour study indicated that the latter had a negative impact close to that of the major classes of medicine used by older people. Given the high number of participants (7,343 for physical activity and 4,279 for sedentary behaviour), these results may be generalised to the entire population of elders, including men and women, whether they be living in an institution or in the community. To prevent falls, caregivers should support and motivate this category of subjects to regularly engage in practice physical exercises and follow recommendations of the American College of Sports Medicine [59].
References
Hauer K, Becker C, Lindemann U, Beyer N (2006) Effectiveness of physical training on motor performance and fall prevention in cognitively impaired older persons: a systematic review. Am J Phys Med Rehabil 85(10):847–857
Rubenstein LZ, Josephson KR, Robbins AS (1994) Falls in the nursing home. Ann Intern Med 121(6):442–451
van Weel C, Vermeulen H, van den Bosch W (1995) Falls, a community care perspective. Lancet 345(8964):1549–1551
Dargent-Molina P, Bréart G (1995) Epidémiologie des chutes et des traumatismes liés aux chutes chez les aux chutes chez les personnes âgées. Rev Epidemiol Sante Publique 43(1):72–83
Hausdorff JM, Rios DA, Edelberg HK (2001) Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil 82(8):1050–1056
Robitaille Y, O’Loughlin J (1990) Épidémiologie de la chute chez les personnes âgées. L’année gérontologique 145–155
Prudham D, Evans JG (1981) Factors associated with falls in the elderly: a community study. Age Ageing 10(3):141–146
Blake AJ, Morgan K, Bendall MJ, Dallosso H (1988) Falls by elderly people at home: prevalence and associated factors. Age Ageing 17(6):365–372
Tinetti ME, Speechley M, Ginter SF (1988) Risk factors for falls among elderly persons living in the community. N Engl J Med 319(26):1701–1707
Downton JH, Andrews K (1991) Prevalence, characteristics and factors associated with falls among the elderly living at home. Aging (Milano) 3(3):219–228
O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S (1993) Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol 137(3):342–354
Graafmans WC, Ooms ME, Hofstee HM, Bezemer PD, Bouter LM, Lips P (1996) Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol 143(11):1129–1136
Dolinis J, Harrison JE, Andrews GR (1997) Factors associated with falling in older Adelaïde residents. Aust N Z J Public Health 21(5):462–468
Cesari M, Landi F, Torre S, Onder G, Lattanzio F, Bernabei R (2002) Prevalence and risk factors for falls in an older community-dwelling population. J Gerontol A Biol Sci Med Sci 57(11):M722–M726
Avdic D, Pecar D, Mujic-Skikic E (2004) Risk factors of fall in elderly people. Bosn J Basic Med Sci 4(4):71–78
Morris M, Osborne D, Hill K, Kendig H, Lundgren-Lindquist B, Browning C et al (2004) Predisposing factors for occasional and multiple falls in older Australians who live at home. Aust J Physiother 50(3):153–159
Reyes-Ortiz CA, Al Snih S, Loera J, Ray LA, Markides K (2004) Risk factors for falling in older Mexican Americans. Ethn Dis 14(3):417–422
Sieri T, Beretta G (2004) Fall risk assessment in very old males and females living in nursing homes. Disabil Rehabil 26(12):718–723
Leipzig RM, Cumming RG, Tinetti ME (1999) Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc 47(1):30–39
Leipzig RM, Cumming RG, Tinetti ME (1999) Drugs and falls in older people: a systematic review and meta-analysis: II. Cardiac and analgesic drugs. J Am Geriatr Soc 47(1):40–50
Woolcott JC, Richardson JK, Wiens MO, Patel B, Marin J, Khan KM et al (2009) Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med 169(21):1952–1960
Bloch F, Thibaud M, Dugué B, Brèque C, Rigaud AS, Kemoun G (2011) Psychotropic drugs and falls in the elderly people: updated literature review and meta-analysis. J Aging Health 23(2):329–346
Bloch F, Thibaud M, Dugué B, Brèque C, Rigaud AS, Kemoun G (2010) Laxatives as a risk factor for iatrogenic falls in elderly subjects: myth or reality? Durgs Aging 27(11):895–901
Moreland JD, Richardson JA, Goldsmith CH, Clase CM (2004) Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc 52(7):1121–1129
Muir SW, Berg K, Chesworth B, Klar N, Speechley M (2010) Quantifying the magnitude of risk for balance impairment on falls in community-dwelling older adults: a systematic review and meta-analysis. J Clin Epidemiol 63(4):389–406
Bloch F, Thibaud M, Dugué B, Brèque C, Rigaud AS, Kemoun G (2010) Episodes of falling among elderly people: a systematic review and meta-analysis of social and demographic pre-disposing characteristics. Clinics 65(9):895–903
Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC (2008) Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc 56(12):2234–2243
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283(15):2008–2012
Sibbald B, Roland M (1998) Understanding controlled trials. Why are randomised controlled trials important? BMJ 316:201
ANAES (Agence Nationale d’Accréditation et d’Evaluation en Santé) (2000) Guide d’analyse de la littérature et gradation des recommandations
Cook DJ, Guyatt GH, Laupacis A, Sackett DL (1992) Rules of evidence and clinical recommendations on the use of antithrombotic agents. Chest 102:305S–311S
Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 22:719–748
Egger M, Smith GD, Altman DG (2001) Systematic reviews in health care: meta-analysis in context. BMJ Books, London
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analysis. BMJ 327(7414):557–560
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088–1099
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Brauer SG, Burns YR, Galley P (2000) A prospective study of laboratory and clinical measures of postural stability to predict community-dwelling fallers. J Gerontol A Biol Sci Med Sci 55(8):M469–M476
Covinsky KE, Kahana E, Kahana B, Kercher K, Schumacher JG, Justice AC (2001) History and mobility exam index to identify community-dwelling elderly persons at risk of falling. J Gerontol A Biol Sci Med Sci 56(4):M253–M259
Liu BA, Topper AK, Reeves RA, Gryfe C, Maki BE (1995) Falls among older people: relationship to medication use and orthostatic hypotension. J Am Geriatr Soc 43(10):1141–1145
Luukinen H, Koski K, Kivela SL, Laippala P (1996) Social status, life changes, housing conditions, health, functional abilities and life-style as risk factors for recurrent falls among the home-dwelling elderly. Public Health 110(2):115–118
Maki BE, Holliday PJ, Topper AK (1994) A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. J Gerontol 49(2):M72–M84
Teno J, Kiel DP, Mor V (1990) Multiple stumbles: a risk factor for falls in community-dwelling elderly: a prospective study. J Am Geriatr Soc 38(12):1321–1325
Herndon JG, Helmick CG, Sattin RW, Stevens JA, DeVito C, Wingo PA (1997) Chronic medical conditions and risk of fall injury events at home in older adults. J Am Geriatr Soc 45(6):739–743
Peel NM, McClure RJ, Hendrikz JK (2006) Health-protective behaviours and risk of fall-related hip fractures: a population-based case–control study. Age Ageing 35(5):491–497
Buatois S, Gueguen R, Gauchard GC, Benetos A, Perrin PP (2006) Posturography and risk of recurrent falls in healthy non-institutionalized persons aged over 65. Gerontology 52(6):345–352
Faulkner KA, Redfern MS, Cauley JA, Landsittel DP, Studenski SA, Rosano C et al (2007) Multitasking: association between poorer performance and a history of recurrent falls. J Am Geriatr Soc 55(4):570–576
Huang HC (2004) A checklist for assessing the risk of falls among the elderly. J Nurs Res 12(2):131–142
Johnson CS (2003) The association between nutritional risk and falls among frail elderly. J Nutr Health Aging 7(4):247–250
Isberner F, Ritzel D, Sarvela P, Brown K, Hu P, Newbolds D (1998) Falls of elderly rural home health clients. Home Health Care Serv Q 17(2):41–51
Koepsell TD, Wolf ME, Buchner DM, Kukull WA, LaCroix AZ, Tencer AF et al (2004) Footwear style and risk of falls in older adults. J Am Geriatr Soc 52(9):1495–1501
van Peppen RP, Hendriks HJ, van Meeteren NL, Helders PJ, Kwakkel G (2007) The development of a clinical practice stroke guideline for physiotherapists in The Netherlands: a systematic review of available evidence. Disabil Rehabil 29(10):767–783
Ribeiro AS, Pereira JS (2005) Balance improvement and reduction of likelihood of falls in older women after Cawthorne and Cooksey exercises. Braz J Otorhinolaryngol 71(1):38–46
Schoenfelder DP, Rubenstein LM (2004) An exercise program to improve fall-related outcomes in elderly nursing home residents. Appl Nurs Res 17(1):21–31
Kemoun G, Thibaud M, Roumagne N, Carette P, Albinet C, Toussaint L et al (2010) Effects of a physical training programme on cognitive function and walking efficiency in elderly persons with dementia. Dement Geriatr Cogn Disord 29(2):109–114
Choi JH, Moon JS, Song R (2005) Effects of Sun-style Tai Chi exercise on physical fitness and fall prevention in fall-prone older adults. J Adv Nurs 51(2):150–157
Feder G, Cryer C, Donovan S, Carter Y (2000) Guidelines for the prevention of falls in people over 65. The Guidelines’ Development Group. BMJ 321(7267):1007–1011
Gillespie LD, Robertson MC, Gillespie WJ, Lamb SE, Gates S, Cumming RG et al (2009) Intervention for preventing falls in older people living in the community. Cochrane Database Syst Rev 15(2):CD007146
Brassington GS, King AC, Bliwise DL (2000) Sleep problems as a risk factor for falls in a sample of community-dwelling adults aged 64–99 years. J Am Geriatr Soc 48(10):1234–1240
American College of Sports Medicine, Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, Salem GJ et al (2009) American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc 41(7):1510–1530
Assantachai P, Praditsuwan R, Chatthanawaree W, Pisalsarakij D, Thamlikitkul V (2003) Risk factors for falls in the Thai elderly in an urban community. J Med Assoc Thai 86(2):124–130
Chan KM, Pang WS, Ee CH, Ding YY, Choo P (1997) Epidemiology of falls among the elderly community dwellers in Singapore. Singapore Med J 38(10):427–431
Lord SR, Ward JA, Williams P, Anstey KJ (1993) An epidemiological study of falls in older community-dwelling women: the Randwick falls and fractures study. Aust J Public Health 17(3):240–245
Toulotte C, Thevenon A, Watelain E, Fabre C (2006) Identification of healthy elderly fallers and non-fallers by gait analysis under dual-task conditions. Clin Rehabil 20(3):269–276
Ishizuka MA, Mutarelli EG, Yamaguchi AM, Jacob Filho W (2005) Falls by elders with moderate levels of movement functionality. Clinics 60(1):41–46
Murray KJ, Hill K, Phillips B, Waterston J (2005) A pilot study of falls risk and vestibular dysfunction in older fallers presenting to hospital emergency departments. Disabil Rehabil 27(9):499–506
Pajala S, Era P, Koskenvuo M, Kaprio J, Viljanen A, Rantanen T (2006) Genetic factors and susceptibility to falls in older women. J Am Geriatr Soc 54(4):613–618
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Thibaud, M., Bloch, F., Tournoux-Facon, C. et al. Impact of physical activity and sedentary behaviour on fall risks in older people: a systematic review and meta-analysis of observational studies. Eur Rev Aging Phys Act 9, 5–15 (2012). https://doi.org/10.1007/s11556-011-0081-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11556-011-0081-1