Abstract
Background
There is a well-documented association between carpal tunnel syndrome (CTS) and thumb carpometacarpal (CMC) arthritis, and these conditions commonly coexist. We have observed that patients who have previously undergone thumb basal joint arthroplasty (BJA) seem rarely to present subsequently with CTS. Our hypothesis is that BJA decreases the pressure within the carpal tunnel.
Methods
Twenty-eight patients (6 with coexistent CTS) undergoing BJA were enrolled in the study. The pressure within the carpal tunnel immediately before and after BJA was measured using a commercially available pressure monitor device (Stryker STIC; Kalamazoo, MI). In patients with concomitant CTS undergoing both BJA and carpal tunnel release (CTR), the pressure was measured after BJA but prior to release of the transverse carpal ligament.
Results
The pressure within the carpal tunnel decreased after BJA in all patients. There were 3 patients with stage II arthritis, 15 patients with stage III arthritis, and 10 patients with stage IV arthritis. The mean pressure prior to BJA among all patients was 23.9 mmHg and decreased to 11.0 mmHg after BJA. Patients with concomitant CTS had a mean pre-BJA pressure of 26.5 mmHg, which decreased to 7.3 mmHg after BJA.
Conclusions
BJA decompresses the carpal tunnel and decreases the pressure within. In patients with concomitant CTS, the BJA alone (without additional release of the transverse carpal ligament) decreases the carpal tunnel pressure. Further study is warranted to determine the need for discrete release of the transverse carpal ligament in patients with CTS who are undergoing BJA.
Level of Evidence
Level II, diagnostic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Carpal tunnel syndrome (CTS) and thumb carpometacarpal (CMC) arthritis are common conditions seen by hand surgeons. There is a well-documented association between these conditions, with the rate of concomitant CTS and CMC arthritis reported to be as high as 43 % [4]. The precise etiology of this association is not known. It may be that because these conditions are common, we see these together clinically by coincidence. Alternatively, it has been suggested by several authors that the arthritic process at the basal joint of the thumb results in mechanical alterations in the shape, size, and volume of the carpal tunnel all of which may contribute to the development of CTS [2, 6, 9].
Despite this high prevalence of concomitant CTS and CMC arthritis, it has been our anecdotal experience that patients who have undergone basal joint arthroplasty (BJA) do not seem to present with CTS in the future. Although this has never been discretely studied or documented, removal of the trapezium (a portion of the rigid bony wall of the carpal tunnel) during BJA and secondary decompression of the carpal tunnel may be protective against the development of CTS. Several studies support an anatomic basis for this. Goldfarb et al.[6] demonstrated using MRI that the volume of the carpal tunnel increases after ligament reconstruction with tendon interposition (LRTI), and Cassidy et al.[1] demonstrated in a cadaver study that trapezial excision decreased the pressure within the carpal tunnel.
The purpose of the present study was to evaluate, in vivo, the pressure within the carpal tunnel in patients with CMC arthritis and the extent to which the pressure in the carpal tunnel changes after BJA. Our hypothesis is that BJA decreases the pressure within the carpal tunnel.
Materials and Methods
An institutional review board approval was obtained, and patients were consented for the study. We prospectively enrolled patients undergoing isolated, primary BJA or concomitant BJA and carpal tunnel release (CTR) for the study. Informed consent was obtained. Patients were diagnosed with CMC arthritis based on an evaluation of history, physical examination findings including tenderness at the CMC joint and crepitus and/or pain with CMC grind, and radiographic studies demonstrating osteoarthritic changes at the CMC joint of the thumb. Patients were considered for BJA after failure of nonoperative treatment modalities including splints, anti-inflammatories, therapy, and/or corticosteroid injections. The duration of nonoperative treatment and specific nonoperative regimen was at the discretion of the treating physician.
Patients were also evaluated clinically for concomitant carpal tunnel syndrome using standard history and physical exam findings, including the criteria reported by Graham [7]: numbness in the median nerve territory, nocturnal symptoms, thenar atrophy, positive Phalen’s, loss of 2-point discrimination, or a positive Tinel’s. Patients in whom carpal tunnel was suspected on the basis of the above had nerve conduction studies.
Patients with inflammatory arthritis, a history of previous carpal tunnel release, prior BJA undergoing revision, or history of other previous surgery that could have altered the anatomy of or violated the carpal tunnel were excluded.
There were 28 patients (21 female and 7 male). The average age of the patients was 63 years (range 46–79 years old). Based on the classification system of Eaton and Littler [3], there were 3 patients with stage II arthritis, 15 patients with stage III arthritis, and 10 patients with stage IV.
The specific surgical technique of BJA was based on the preference of the treating surgeon. One of us performs a dorsal approach with complete trapeziectomy and abductor pollicis longus suspensionplasty using a suture anchor in the base of the index metacarpal (KL). Two of us (AI and PB) perform a Wagner approach followed by complete trapeziectomy, harvest of the entire flexor carpi radialis in the forearm with dissection to the base of the index metacarpal, then passage of the tendon through bur holes at the base and dorsum of metacarpal. The tendon is then sewn to itself and anchovied and placed into the trapezial void. In patients requiring concomitant carpal tunnel release, a standard open carpal tunnel release was performed.
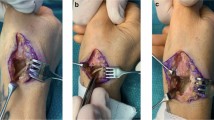
Measurement of the carpal tunnel pressure was performed using a Stryker Intra-Compartmental Pressure Monitor (STIC; Stryker, Kalamazoo, MI). This device is a commonly used and well-accepted device for measuring compartment pressures.
Pre-BJA pressure measurement was obtained by inserting the STIC device at a location 1 cm proximal to the wrist crease and ulnar to the palmaris longus (PL) tendon (or in line with the ring finger, if the PL was absent). The device was zeroed prior to insertion and was advanced at an angle of 30–45° until it touched the floor of the carpal tunnel. The device was then withdrawn 0.5 cm, and the pressure recorded. If necessary, a small volume of saline was injected to clear the tip of the needle as recommended by the manufacturer, and pressure was measured once the reading stabilized. Measurement was obtained with the wrist in a neutral position and with the tourniquet deflated. BJA was then performed. After completion of the BJA, and with the tourniquet again deflated, the carpal tunnel pressure was remeasured using the same technique. If a concomitant CTR was to be performed, the post-BJA measurement was performed prior to the CTR. Sterile technique was maintained at all times.
Results
The mean pressure prior to BJA among all patients was 23.9 mmHg (range 14–49 mmHg) and decreased to 11.0 mmHg (range 2–32 mmHg) after BJA (P < .01). In patients undergoing concomitant CTR for CTS (n = 6), the mean pressure prior to BJA was 26.5 mmHg and decreased (prior to the CTR) to 7.3 mmHg after BJA (P < .01). In patients without CTS (n = 22), the mean pressure prior to BJA was 23.2 mmHg and decreased to 12.0 mmHg after BJA (P < .01).
Discussion
Carpal tunnel syndrome and thumb CMC arthritis are reported to commonly coexist. There has been no definitive explanation for this association, though the basic pathophysiologic abnormality resulting in CTS is an increase in pressure in the carpal tunnel [5].
Several authors have suggested mechanisms by which CMC arthritis could influence the development of CTS. Melone et al.[9] suggested that the inflammatory process associated with CMC arthritis may spread directly to the flexor tenosynovium in the carpal tunnel, resulting in CTS. Anatomically, the primary insertion of the transverse carpal ligament (TCL) on the radial side is the trapezial ridge [8]. As has been suggested by several investigators [2, 4, 6], it is plausible that alterations in peri-trapezial anatomy as a result of the arthritic process could increase the carpal tunnel pressure.
In an effort to further describe the nature of the relationship between CMC arthritis and CTS, Goldfarb et al. [6] performed an MRI study evaluating the volume of the carpal tunnel in seven patients undergoing LRTI, three of whom had CTS and were undergoing concomitant CTR. They found no difference in preoperative carpal tunnel volume (as measured by MRI) between the four patients without CTS and the three patients who had CTS. Postoperatively, they noted a 7 % increase in carpal tunnel volume in the patients undergoing LRTI alone and a 24 % increase in volume in those patients who required both an LRTI and CTR.
Gelberman et al. [5] used a wick catheter to measure carpal tunnel pressures in patients with and without CTS and found a mean pressure of 2.5 mmHg in patients without CTS and a mean of 32 mmHg in patients with CTS. The mean preoperative carpal tunnel pressure in our patients without evidence of CTS was 18.8 mmHg. Although there may be some differences between our studies attributable to measurement technique, based on a comparison between these data, it appears that the baseline carpal tunnel pressure in patients with CMC arthritis is higher than that in the general population. This presumably means that in patients with CMC arthritis, there is less of an increase in pressure necessary to reach the pressure threshold to develop CTS.
The primary purpose of our study was to assess the extent to which the carpal tunnel pressure decreases with BJA, and we found that carpal tunnel pressures decreased in all patients after BJA. Cassidy et al [1] used a cadaver model of CTS to measure changes in the carpal tunnel pressure after trapeziectomy. They inflated a balloon within the carpal tunnels of four cadaver limbs to a mean pressure of 33 mmHg. After performing a trapeziectomy, they found that the pressure within the carpal tunnel decreased by a mean of 7 mmHg. The carpal tunnel pressure did not return to baseline (0 mmHg) until the remainder of the TCL was released from the scaphoid tubercle, which was performed through the same incision as the trapeziectomy. The results of our study are similar in that in no case did the carpal tunnel pressure decrease to 0 after BJA. Based on our data, we agree with the findings of Cassidy et al. and conclude that trapeziectomy alone, without additional release of the TCL, is insufficient to fully decompress the carpal tunnel. On the other hand, nine of our patients had post-BJA pressures of 5 mmHg or less. Additionally, in contrast to the 7 mmHg decrease in pressure found by Cassidy et al., the mean change in pressure after BJA alone in patients with CTS in our study was 19.2 mmHg. It is possible that this decrease in pressure seen with BJA alone would be sufficient to relieve the symptoms in a patient with associated CTS, but further study is necessary to determine this. Also, we had more women than men in our study. It is possible that, given differences in ligamentous laxity and/or soft tissue compliance, the magnitude of pressure changes and the clinical effect of this change between women and men would differ.
We found that the pressure in patients with CTS decreased more (Δ19.2 mmHg) compared to patients without CTS (Δ11.1 mmHg). We do not have a definitive explanation for this difference; however, we feel this is likely due to the greater initial pressure within the carpal tunnel in patients with concomitant CTS.
Another purpose of our study was to determine whether there may be an anatomic basis for our observation that patients with previous BJA rarely seem to develop CTS in the future. We found that the mean pressure in the carpal tunnel after BJA decreased to 11.0 mmHg. While this remains higher than the baseline level of the general population as measured by Gelberman et al., it is notably lower than the pre-BJA level in our patients with CMC arthritis. After BJA and with the trapezium (which normally forms one portion of the firm wall of the carpal tunnel) removed, it is possible that a greater increase in pathologic compression would be necessary to bring the pressure in the carpal tunnel back up to a level sufficient to cause carpal tunnel symptoms. Without the bony wall of the trapezium, it may be difficult for this increase in pressure to occur. Further study on the incidence of CTS after BJA, and/or long-term follow-up measurements of the carpal tunnel pressure in patients after BJA, would be helpful to confirm this theory.
The strengths of our study include that we used a commercially available and accepted device to measure the in vivo pressure within the carpal tunnel and that we utilized a consistent measurement technique among all patients. There are several potential weaknesses to our study. Although the presence of coexistent CTS and CMC arthritis has been reported to be quite high, in our study, only 21 % (6/28) patients undergoing BJA had concomitant, clinically evident, CTS. It is possible that with a greater number of patients in this subgroup, the results would differ. We feel this is unlikely, however, as we noted a consistent decrease in the carpal tunnel pressure in all patients. Also, it is possible that there were errors in measurement or that the needle was not positioned within the carpal tunnel. We did not use imaging to confirm the needle placement, but used a well-accepted approach for localizing the carpal tunnel and a standard measurement technique. It is possible that the volume of saline infused to clear the needle tip, the level at which it was zeroed, or the angle of insertion varied from case to case, and this may have influenced the results. Again, we think this is unlikely to have had a significant effect given the consistency of our findings. Finally, the investigators were not blinded to the presence or absence of CTS or blinded to whether the measurement was pre- or post-BJA. While this may have introduced some degree of bias into the measurements, given the nature of the device itself and the digital readout pressure display, there is little room for subjectivity. Finally, we are not able to conclude definitively whether BJA alone is sufficient to relieve symptoms of CTS in patients with both CMC arthritis and CTS.
In conclusion, we found that the baseline pressure within the carpal tunnel in patients with CMC arthritis is higher than what would be expected in the general population and that these patients may therefore have a lower threshold for the development of CTS. The pressure in the carpal tunnel decreases after BJA alone. Further investigation is necessary to determine whether this decrease in pressure is sufficient to relieve CTS symptoms, and at this time in patients with both CMC arthritis and CTS, we recommend discrete release of the TCL in addition to BJA. The decrease in pressure and decompression of the carpal tunnel during BJA may be protective against the development of CTS in the future.
References
Cassidy C, Glennon PE, Stein AB, et al. Basal joint arthroplasty and carpal tunnel release through a single incision: an in vitro study. J Hand Surg [Am]. 2004;29:1085–8.
Crosby EB, Linscheid RL, Dobyns JH. Scaphotrapezial trapezoidal arthrosis. J Hand Surg [Am]. 1978;3:223–34.
Eaton RG, Littler JW. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg Am. 1973;55:1655–66.
Florack TM, Miller RJ, Pellegrini VD, et al. The prevalence of carpal tunnel syndrome in patients with basal joint arthritis of the thumb. J Hand Surg [Am]. 1992;17:624–30.
Gelberman RH, Hergenroeder PT, Hargens AR, et al. The carpal tunnel syndrome. A study of carpal canal pressures. J Bone Joint Surg Am. 1981;63:380–3.
Goldfarb CA, Kiefhaber TR, Stern PJ, et al. The relationship between basal joint arthritis and carpal tunnel syndrome: an MRI pilot study. J Hand Surg [Am]. 2003;28:21–7.
Graham B. The value added by electrodiagnostic testing in the diagnosis of carpal tunnel syndrome. J Bone Joint Surg Am. 2008;90:2587–93.
Hepinstall MS, Yang SS. Indirect decompression of the carpal tunnel during basal joint arthroplasty of the thumb. J Hand Surg [Am]. 2008;33:1057–62.
Melone CP, Jr., Beavers B, Isani A. The basal joint pain syndrome. Clin Orthop Relat Res. 1987:58–67.
Conflict of Interest
Kevin Lutsky is a consultant for Synthes. Pedro Beredjiklian has stock/stock options in Tornier, Inc. and receives payments for development of educational presentations including service on speakers’ bureaus for TriMed, Inc. and gives expert testimony for malpractice/work compensation. Asif Ilyas is a consultant for Wright Medical Technology, gives expert testimony, is a paid author for Jaypee Medical Publishers, and receives payment for educational presentations. These are financial disclosures that have no bearing on this study; authors did not receive any financial compensation for this study.
Statement of Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 [1].
Statement of Informed Consent
Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Lutsky, K., Ilyas, A., Kim, N. et al. Basal joint arthroplasty decreases carpal tunnel pressure. HAND 10, 403–406 (2015). https://doi.org/10.1007/s11552-014-9724-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-014-9724-9