Abstract
Purpose
To assess and compare the clinical effectiveness of percutaneous intradiscal ozone therapy in patients affected by lumbar disc herniation, with and without history of COVID-19 infection.
Materials and Methods
After the rising of COVID-19 pandemics in Italy, 47 consecutive percutaneous intradiscal ozone therapies were performed on patients with low back pain and/or sciatic pain due to lumbar disc herniation. Among these, 19 had suffered from COVID-19 and successively recovered with no residual symptoms, while the remaining 28 had not previously been affected by COVID-19 and were not convalescent. Oswestry Disability Index (ODI) was administered before the treatment and at 1-month and 3-month follow-up in order to assess the clinical outcome.
Results
The two groups were similar in terms of patient age (p-value 0.54), treated levels (p-value 0.26) and pre-procedure ODI (p-value 0.33). Technical success was achieved in all cases. In patients previously affected by COVID-19, mean ODI decrease was 11.58 ± 9.51 (35.72%) at 1-month follow-up and 20.63 ± 9.87 (63.63%) at 3-month follow-up. In patients never affected by COVID-19, mean ODI decrease was 20.93 ± 10.53 (58.73%) at 1-month follow-up and 22.07 ± 11.36 (61.92%) at 3-month follow-up. Eventually, clinical success was registered in 84.21% (16/19) of patients with history of COVID-19 infection and in 85.71% (24/28) of patients with no history of COVID-19 infection. No major complication was registered.
Conclusions
In case of lumbar disc herniation treated with percutaneous intradiscal ozone therapy, patients previously affected by COVID-19 showed a significantly longer recovery time.
Similar content being viewed by others
Introduction
Low back pain (LBP) is a common clinical, public health and socioeconomic problem affecting patients worldwide [1]. More than half adults all over the world suffer from LBP at some point of their life with different degrees of symptom severity, and many cases have LBP associated with sciatic symptoms [2]. However, only few patients develop LBP related to degenerative joints and disc disease [3]. The mechanism of lumbar pain is yet to be properly understood and is likely to be multifactorial, with both mechanical and inflammatory factors [4]. At present, pain is seen as the result of irritation and chemical inflammation of peripheral nerves due to the surrounding intervertebral discs compression [5], throughout the release of inflammatory cytokines, which make the nerve root oversensitive to mechanical compression itself [6]. As is known, musculoskeletal disorders (MSDs) involving muscles, tendons, joints, and spinal discs lead to decreased work effectiveness and quality of life [7, 8]. The prevalence of these disorders may vary on the base of individual habits and lifestyle modifications. In this connection, the onset of the COVID-19 pandemics has forced governments to establish social restrictions to prevent its spread [9]. Mandatory home isolation with prolonged sitting and insufficient physical activity caused higher risk of MSD, in particular lumbar pain [10]. Moreover, loneliness and social isolation increased the perceived pain [11], especially in patients who have been affected by COVID-19.
Therefore, the aim of this study is to assess and compare clinical outcome and recovery time in patients with and without history of COVID-19 infection, and treated with percutaneous intradiscal ozone therapy for lumbar disc herniation.
Material and methods
Ethics statements
Institutional review board approval for this study was waived because the studied procedure is ordinarily performed in our institution and is not considered experimental. Appropriate written informed consent was collected before every procedure. All data were retrospectively collected by a dedicated data manager. The authors declare that they have no conflict of interest. No funding was received to support this study.
Patients population
After the rising of COVID-19 pandemics in Italy, 47 consecutive percutaneous intradiscal ozone therapies were performed on patients with LBP and/or sciatic pain due to lumbar disc herniation. Among these, 19 had suffered from COVID-19 1-to-3-month before the procedure and successively recovered with no residual symptoms, while the remaining 28 had not previously been affected by COVID-19 and were not convalescent. Among patients previously affected by COVID-19, only 3 were hospitalized for mild dyspnea and discharged after a maximum period of 7 days. Oswestry Disability Index (ODI) was administered before the treatment and at 1-month and 3-month follow-up in order to assess the clinical outcome.
Ozone generator and administration technique
A commercially available oxygen/ozone generator (Medical 99 IR, Multiossigen s.r.l., Gorle, Italy) was used to generate the desired concentration of the oxygen/ozone mixture. The ozone administration was performed in sterile conditions, after proper disinfection of the lumbar region. No local anesthesia was used in the puncture site before the procedure. With patients laid in the prone position, ozone was injected through a sterile 22-gauge 15-cm-long Chiba needle (Cook Medical, Bloomington, IN) previously placed in the intervertebral space under imaging guidance. In our department, imaging guidance was performed using fluoroscopy or computed tomography (CT), on the base of operator preference and technique room availability. Previous studies showed how fluoroscopic guidance reduces operative time and radiation exposure in comparison with CT guidance for intradiscal ozone therapy [12, 13]. Ozone was collected with a polypropylene 10-mL syringe, and 5 mL of ozone/oxygen mixture at 30 µg/mL concentration rate was injected into the disc. Afterward, additional 5 mL of ozone/oxygen mixture at similar concentration rate was injected into the soft paravertebral tissues in the surroundings of the nerve root, together with a 2-mL solution containing 1mL of Depo-Medrol 40mg/mL and 1 mL of Lidocaine Hydrochloride 20mg/mL. Oral antibiotic therapy was prescribed for 5 days, starting from the day before the procedure. Additional taking of paracetamol was recommended in case of exacerbated pain. No other pre-operation and/or post-operation medications were administered to patients. After the procedure, patients were discharged within two hours and invited to avoid strenuous activities for at least 2 days.
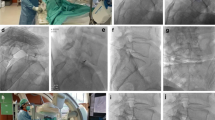
Fluoroscopy-guided procedure
The patient laid in the prone position on a digital subtraction angiography (DSA) operating table (Allura Xper FD20, Philips Medical, Eindhoven, NL). At first, the lateral projection was obtained and alignment of the endplates of the involved disc space was performed through cranial and caudal angulations of the C-arm to clearly open the disc space. Then, the C-arm was rotated at an angle of around 30°, so that the facet joint superimposed on the posterior third of the disc space produces the so-called Scotty dog appearance. In general, the puncture site is around 8cm away from the vertebral spinous process line. The needle tip was placed in the center of the disc under DSA, with insertion along the ‘security triangle’ through the posterior-lateral pathway. In the oblique projection, the needle was inserted just anterior and lateral to the superior articular process of the inferior vertebra (i.e., ‘Scotty dog’ ear) at the direction of the X-ray beam. The position of the needle tip was confirmed in the center of the disc by both posterior–anterior and lateral fluoroscopy images, and the administration was started.
CT-guided procedure
The patient laid in the prone position on a CT sliding table (Aquilion Prime SP, Toshiba Medical Systems Europe, Zoetermeer, NL). Three-mm slice-thickness CT sections, parallel to the edge of the vertebra, were obtained for intervention planning. In the following, the needle was advanced through the soft tissues to the nucleus pulposus, with an extraspinal lateral approach by the same side of major pain. CT scans were used to monitor the advancing needle. With the needle tip well positioned, the administration was started. In case of puncture site at the level of L5-S1, a pillow was used to increase the lumbosacral angle. A post-procedural CT scan was performed to show the distribution of gas after the injection.
Outcome measures
Patients underwent a 1-month and 3-month follow-up in order to determine the effectiveness of the procedure. Oswestry Low Back Pain Disability Questionnaire [14] was administered to all patients on the day of the procedure, after 1-month and 3-month follow-up. ODI is a percentage score, calculated on the base of a 10-item questionnaire, one item for pain and the other items to assess the pain impact on daily life activities such as personal care, lifting, walking, sitting, standing, sleeping, sexual life (if applicable), social life, and traveling. The response to treatment was considered binary in accordance with literature recommendations [15, 16]: it was categorized as successful (responders) in case of reduction in the preoperative ODI values of at least 30% during follow-up; unsuccessful (non-responders) if otherwise. Patients unable to return the questionnaire were interviewed on telephone. Recovery time was established on the base of follow-up ODI results and the related decrease.
Statistical analysis
The statistical analysis was performed with MATLAB statistical toolbox version 2008 (MathWorks, Natick, MA, USA) for Windows at 32 bit. All data were analyzed as numbers and percentage for qualitative variables and mean and range for quantitative variables. Chi-squared test for qualitative variables and Student’s t test for quantitative variables were used to compare the groups’ characteristics. Tests with p-value (p) < 0.05 were considered significant.
Results
Table 1 shows the demographics of the patient population and the disc herniation characteristics, respectively.
After the rising of COVID-19 pandemic in Italy, 47 consecutive percutaneous intradiscal ozone therapies for disc herniation were performed in our interventional department on patients aging from 24 to 78 years (mean age 52.11 years; standard deviation: 14.37). Thirty-one of them (57.66%) were male; 16 (42.34%) were female. All cases were retrospectively reviewed.
At the time of the procedure, 19 patients reported a previous COVID-19 disease with no residual symptoms (Group A), while the remaining 28 had never suffered from this infection (Group B). These groups were similar in terms of patient age (p-value 0.39): the average age was 52.11 ± 14.37 years (range 24–78 years) for Group A and 54.89 ± 15.62 years (range 26–78 years) for Group B.
Overall, the mean duration of symptoms before treatment was 3.78 ± 2.14 months (range 1–8 months). Most patients presented with sciatica (24/47, 51.06%), few (4/47, 8.51%) mainly suffered of lumbalgia, and the remaining 19/47 (40.43%) complained of both lumbalgia and sciatica.
The most common level of the treated disc herniation was L4-L5 (35/47, 72.34%) both among patients in Group A (15/19) and among those in Group B (19/28). L5-S1 was treated overall in 12/47 patients (4 in Group A and 8 in Group B). L3-L4 level was treated in 1 patient in each group. No statistical difference was found in the distribution of treated levels between the two groups of patients (p-value 0.26), nor in side of the herniation (p-value 0.44), nor in the disc lesion morphology (p-value 0.29).
Outcomes are listed in Table 2. Technical success of 100% was registered in both groups. According to Oswestry Low Back Pain Disability Questionnaire, the mean pre-procedure ODI score was 32.42 ± 8.53 for patients with previous COVID-19 infection and 35.64 ± 12.41 for the remaining patients, with no significant difference between the two groups. The mean 1-month follow-up ODI score was 20.84 ± 8.55 for Group A and 14.71 ± 7.74 for Group B, with significant statistical difference between them (p-value 0.014). The mean reduction and percentages of symptoms improvement for ODI at 1-month follow-up were 11.58 (36.72%) and 20.93 (58.73%) for patients in Group A and in Group B, respectively. A significant difference was found in the clinical outcome between the two groups at 1-month follow-up (p-value 0.003). Differently, the 3-month follow-up evaluation showed no statistical difference in the mean ODI reduction of the two groups: the mean 3-month follow-up ODI score was 11.68 ± 7.16 for Group A and 13.14 ± 8.06 for Group B (p-value 0.53), and the ODI mean reduction was 20.63 (63.64%) for Group A and 22.07 (63.69%) for Group B (p-value 0.66).
At 3-month follow-up, the clinical success was observed in 16/19 (84.21%) patients with reported previous COVID-19 infection and in 24/28 (85.71%) patients with no history of pandemic disease. No statistical difference was found in the clinical outcome between the two groups (p-value 0.43). The procedure was overall well-tolerated. In this study, there was no major complication such as disc infection, nerve and/or vascular injury.
Discussion
The pathogenesis of disc herniation is not fully understood. Nerve compression and chronic inflammation are supposed to be the cause of pain, which could disappear if the inflammatory response decreases, even with the persistence of protrusion [17]. Oxygen/ozone chemonucleolysis is a minimally invasive intervertebral disc therapy, commonly used for the treatment of disc herniation in the last decades [18]. As many other minimally invasive techniques [19,20,21,22], it is an imaging-guided procedure. In particular, it is based on the imaging-guided administration of an oxygen/ozone medical mixture at nontoxic concentrations (5–40 μg of O3 per ml of oxygen), prepared using ozone generators, which can adjust ozone concentration as required [18, 23]. LBP and/or sciatic pain is generally dominated through a single-session treatment of intradiscal ozone injection with concomitant periradicular infiltration of the oxygen/ozone mixture, steroid and local anesthetic, as the combined injection of these materials has proved to reach a better outcome in comparison with the use of ozone or steroid alone [16, 24].
However, during the COVID-19 pandemic, loneliness and social isolation due to physical distancing measures and travel restrictions have physically and mentally affected health worldwide [25,26,27,28]. These conditions are commonly reputed as great determinants of health and quality of life [29] as well as measures of psychological disorders, like depression [30], and other physical problems, such as cardiovascular diseases [31] and increased blood pressure [32]. Moreover, social isolation and loneliness are also well-known psychosocial risk factors for the exacerbation of pain [33, 34]. The English Longitudinal Study of Ageing (ELSA) epidemiological study established that loneliness leads to higher prevalence of musculoskeletal pain [35]. In accordance, other studies showed that loneliness is strongly associated with pain exacerbation [33, 36, 37] and that social isolation is likely to amplify the perception of pain [34]. Therefore, the psychological stress and the physical isolation due to COVID-19 pandemic surely contributed to the onset of pain [38] and had a large impact on patients with chronic back pain and low tolerance to psychological stress [38,39,40]. Also, this condition should be described in radiological examination reports to best explain radiological findings and avoid medico-legal implications [41].
This study aimed to investigate how COVID-19 infection influences the perception of pain due to disc herniation in patients undergoing intradiscal ozone therapy. So far, authors have investigated several aspects of the oxygen/ozone intradiscal therapy. However, a comparison of LBP perception after intradiscal ozone therapy in patients with and without previous COVID-19 infection has never been performed, to our knowledge. Indeed, an advanced research on pubmed using the combination of the terms ‘intradiscal ozone’ and ‘low back pain’ and/or ‘COVID-19’ gave no pertinent result.
Patients in our series were sorted in two groups on the base of previous COVID-19 infection, and the clinical outcome was assessed and compared using the Oswestry Low Back Pain Disability Questionnaire to measure clinical impairment before the treatment and after 1-month and 3-month follow-up. A statistical significant difference was found between the two groups at 1-month follow-up: In particular, the clinical success rate was significantly lower in patients previously affected by COVID-19, with an average ODI decrease of almost half the mean decrease in patients never affected by COVID-19 (11.58 ± 9.51 versus 20.93 ± 10.53, p-value = 0.003). Differently, this range markedly reduces at 3-month follow-up and no significant difference in mean ODI decrease is detected at this time (20.63 ± 9.87 versus 22.07 ± 11.36, p-value = 0.66). In other words, patients with the history of COVID-19 infection had a slower improvement of disability symptoms, with similar clinical outcome of other patients at 3-month follow-up. Overall, the final outcome in our series (84.21% for patients previously affected by COVID-19; 85.71% for other patients) was slightly superior in comparison with the previous published paper by Ezeldin et al. [42], in which a 6-months follow-up outcome showed an improvement of disability symptoms in 76% of patients. These authors registered a mean ODI score reduction of 15.64 points, which resulted significantly lower than the ODI decrease in our study (21.66 ± 10.66). On the other hand, Gallucci et al. [16] reported an even lower success rate (74%) in patients treated with a combination of intradiscal and intraforaminal injections of oxygen/ozone, steroid and local anesthesia. Another paper by Andreula et al. [43] showed a satisfactory therapeutic outcome in 78.3% of patients receiving an intradiscal (4 mL) and periganglionic (8 mL) injection of oxygen/ozone mixture followed by periganglionic injection of steroids and anesthetic, with a poorer outcome if the solution of steroids and anesthetic was waived (70.3%). In this study, no distinction was made between different types of disc herniations, as proposed by Muto et al. in a paper published in 2008 [44]: In particular, this author reported a success rate of 75–80% for soft disc herniation, 70% for multiple-disc herniations, and 55% for failed back surgery syndrome. Thereby, our overall success rate at 3-month follow-up was similar to what registered by Muto for soft disc herniation. Unfortunately, it was not possible to properly compare our results with previously published papers using a clinical outcome scoring other than the Oswestry Disability Questionnaire, such as Oder [45] and Lu [46]. The first reported successful treatment in 620 subjects with reduction of pain measured by means of VAS score with excellent results in one-third of the patients (reduction from 8 to <3). The latter measured the therapeutic outcome according to the modified Macnab criteria [47] (excellent efficacy in 63.8% of patients, good/fair in 27.6%, poor in 8.6%), with a total effective rate (excellent/good/fair) of 91.4%, slightly superior than ours.
All mentioned papers report a clinical outcome higher than what registered for patients with previous COVID-19 infection in our series at 1-month follow-up. A possible explication of this fact is that pain symptoms were related at least in part to COVID-19. In the last year, many study investigated the impact of COVID-19 pandemic on MSD. An investigation on the prevalence of MSD among Polish Territorial Army soldiers during the COVID-19 pandemic revealed that the most common problem was LBP, followed by neck and knee pain [48]. In their study of the Royal Norwegian Navy, Morken et al. [49] observed that 85% of these soldiers had experienced MSD, and also in this series the most common MSD was in the lower back, shoulders, and neck. Moreover, the authors noticed that civilians had even higher prevalence of MSD than military personnel, thus meaning that isolation and physical distancing measures due to COVID-19 pandemic caused an overall stronger perception of MSD pain in the whole population. However, results in our series clearly indicate that the previous COVID-19 infection significantly influences the effectiveness of percutaneous intradiscal ozone therapy at 1-month follow-up and lengthens the mean recovery time. A common clinical feature of COVID-19 is myalgia, defined as muscle aches and pain [50]. Anyway, emerging data suggest that patients may fail to fully recover after acute COVID-19 disease infection and report symptoms persisting for weeks or months. Those patients have been termed ‘long haulers’ or described as having ‘long-COVID’ [51], and fatigue is a dominant feature. The term ‘fatigue’ has several meanings, including that experienced by people as part of daily life or the one caused by a disease. When complaining of fatigue, patients may actually be referring to weakness, dyspnea, difficulties in concentration, somnolence, or low mood. The subjective experience of fatigue (as with pain) is associated to other concomitant brain processes, such as perceptions, emotions, and cognitions [52]. In this context, the dilated recovery time of some patients in our series (Group A) may be partially explicated as the consequence of increased pain perception in people previously affected by COVID-19 infection.
The primary limitation of this study is the retrospective design. A larger population would be advisable to confirm our results. On the contrary, a potential strength of this paper is the attention paid on COVID-19 pandemic impact on LBP due to herniated disc treated with percutaneous intradiscal ozone therapy.
In conclusion, patients with previous COVID-19 infection with no residual symptoms show a longer recovery time after intradiscal ozone therapy for LBP due to disc herniation, in comparison with patients never affected by COVID-19, with similar clinical outcome after 3-month follow-up.
References
Freynhagen R, Baron R, Gockel U, Tölle TR (2006) PainDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin 22(10):1911–20. https://doi.org/10.1185/030079906X132488 (PMID:17022849)
Kaki AM, El-Yaski AZ, Youseif E (2005) Identifying neuropathic pain among patients with chronic low-back pain: use of the leeds assessment of neuropathic symptoms and Signs pain scale. Reg Anesth Pain Med 30(5):422–8. https://doi.org/10.1016/j.rapm.2005.05.013 (PMID:16135345)
Cohen SP, Williams S, Kurihara C, Griffith S, Larkin TM (2005) Nucleoplasty with or without intradiscalelectrothermal therapy (IDET) as a treatment for lumbar herniated disc. J Spinal Disord Tech 18(Suppl):S119-24
Murphy K, Muto M, Steppan J, Meaders T, Boxley C (2015) Treatment of contained herniated lumbar discs with ozone and corticosteroid: a pilot clinical study. Can Assoc Radiol J 66(4):377–84. https://doi.org/10.1016/j.carj.2015.01.003 (PMID:26092159)
Miyoshi S, Sekiguchi M, Konno S, Kikuchi S, Kanaya F (2011) Increased expression of vascular endothelial growth factor protein in dorsal root ganglion exposed to nucleus pulposus on the nerve root in rats. Spine 36(1):E1–E6 (PMID:21243740)
Giurazza F, Guarnieri G, Murphy KJ, Muto M (2017) Intradiscal O2O3: rationale, injection technique, short- and long-term outcomes for the treatment of low back pain due to disc herniation. Can Assoc Radiol J 68(2):171–177. https://doi.org/10.1016/j.carj.2016.12.007 (PMID:28438284)
Wongwitwichote K, Jalayondeja W, Mekhora K, Jalayondeja C (2017) Physical activity, sitting time and work-related musculoskeletal disorders in computer workers. Jpn J Ergon 53:S450-3
Puig-Ribera A, Martínez-Lemos I, Giné-Garriga M, González-Suárez ÁM, Bort-Roig J, Fortuño J et al (2015) Self-reported sitting time and physical activity: interactive associations with mental well-being and productivity in office employees. BMC Public Health 15:1–10
Huang C, Wang Y, Li X et al (2020) Clinical feature of patients infected with 2019 novel coronavirus in Wuhan. China Lancet 395:497–506
Mattioli AV, Ballerini Puviani M, Nasi M, Farinetti A (2020) COVID-19 pandemic: the e_ects of quarantine on cardiovascular risk. Eur J Clin Nutr 74:852–855
Yamada K, Wakaizumi K, Kubota Y, Murayama H, Tabuchi T (2021) Loneliness, social isolation, and pain following the COVID-19 outbreak: data from a nationwide internet survey in Japan. Sci Rep 11(1):18643. https://doi.org/10.1038/s41598-021-97136-3 (PMID:34545110)
Somma F, Gatta G, Negro A et al (2022) Intradiscal ozone therapy: fluoroscopic guidance reduces operative time in comparison with CT guidance in patients with lumbar disc herniation. Radiol Med. https://doi.org/10.1007/s11547-022-01469-6 (PMID: 35290568)
Somma F, D’Agostino V, Negro A et al (2022) Radiation exposure and clinical outcome in patients undergoing percutaneous intradiscal ozone therapy for disc herniation: fluoroscopic versus conventional CT guidance. PLoS One 17(3):e0264767. https://doi.org/10.1371/journal.pone.0264767 (PMID:35290390)
Fairbank JC, Couper J, Davies JB, O’Brien JP (1980) The Oswestry low back pain disability questionnaire. Physiotherapy 66:271–273
Ostelo RW, Deyo RA, Stratford P et al (2008) Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine 33(1):90–4. https://doi.org/10.1097/BRS.0b013e31815e3a10 (PMID:18165753)
Gallucci M, Limbucci N, Zugaro L et al (2007) Sciatica: treatment with intradiscal and intraforaminal injections of steroid and oxygen-ozone versus steroid only. Radiology 242:907–913
Satoh K, Konno S, Nishiyama K et al (1999) Presence and distribution of antigen-antibody complexes in the herniated nucleus pulposus. Spine 24:1980–84
Andreula CF, Simonetti L, De Santis F et al (2003) Minimally invasive oxygen-ozone therapy for lumbar disk herniation. Am J Neuroradiol 24(5):996–1000
Fiore F, Stoia V, Somma F (2020) Surgical recurrence of solitary fibrous tumor of the pleura treated with microwave (MW) thermoablation: a case report. Thorac Cancer 11(2):443–446. https://doi.org/10.1111/1759-7714.13263
Somma F, Stoia V, D’Angelo R, Fiore F (2021) Imaging-guided radiofrequency ablation of osteoid osteoma in typical and atypical sites: long term follow up. PLoS One 16(3):e0248589. https://doi.org/10.1371/journal.pone.0248589.PMID:33735214;PMCID:PMC7971862
Somma F, Stoia V, Serra N, D’Angelo R, Gatta G, Fiore F (2019) Yttrium-90 trans-arterial radioembolization in advanced-stage HCC: the impact of portal vein thrombosis on survival. PLoS One. 14(5):e0216935
Somma F, D’Angelo R, Serra N, Gatta G, Grassi R, Fiore F (2015) Use of ethanol in the trans-arterial lipiodol embolization (TAELE) of intermediated-stage HCC: is this safer than conventional trans-arterial chemo-embolization (c-TACE)? PLoS One 10(6):e0129573
Bocci VA (2006) Scientific and medical aspects of ozone therapy. State of the art. Arch Med Res 37(4):425–35. https://doi.org/10.1016/j.arcmed.2005.08.006 (PMID:16624639)
Andreula C, Muto M, Leonardi M (2004) Interventional spinal procedures. Eur J Radiol 50:112–119
Smith BJ, Lim MH (2020) How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Res Pract 30:2–5
Banerjee D, Rai M (2020) Social isolation in Covid-19: the impact of loneliness. In. J Soc Psychiatry 66:525–527
Killgore WDS, Cloonan SA, Taylor EC, Dailey NS (2020) Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res 290:113117
Murayama H, Okubo R, Tabuchi T (2021) Increase in social isolation during the COVID-19 pandemic and its association with mental health: findings from the JACSIS 2020 study. Int J Environ Res Public Health 18:8238
Liu LJ, Guo Q (2007) Loneliness and health-related quality of life for the empty nest elderly in the rural area of a mountainous county in China. Qual Life Res 16:1275–1280
Erzen E, Cikrikci O (2018) The effect of loneliness on depression: a meta-analysis. Int J Soc Psychiatry 64:427–435
Sorkin D, Rook KS, Lu JL (2002) Loneliness, lack of emotional support, lack of companionship, and the likelihood of having a heart condition in an elderly sample. Ann Behav Med 24:290–298
Hawkley LC, Thisted RA, Masi CM, Cacioppo JT (2010) Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging 25:132–141
Wolf LD, Davis MC (2014) Loneliness, daily pain, and perceptions of interpersonal events in adults with fibromyalgia. Health Psychol 33:929–937
Karayannis NV, Baumann I, Sturgeon JA, Melloh M, Mackey SC (2019) The impact of social isolation on pain interference: a longitudinal study. Ann Behav Med 53:65–74
Smith TO, Dainty JR, Williamson E, Martin KR (2019) Association between musculoskeletal pain with social isolation and loneliness: analysis of the english longitudinal study of ageing. Br J Pain 13:82–90
Jaremka LM et al (2013) Loneliness predicts pain, depression, and fatigue: Understanding the role of immune dysregulation. Psychoneuroendocrinology 38:1310–1317
Powell VD et al (2021) Unwelcome companions: loneliness associates with the cluster of pain, fatigue, and depression in older adults. Gerontol Geriatr Med 7:2333721421997620
Karos K et al (2020) The social threats of COVID-19 for people with chronic pain. Pain 161:2229–2235
Clauw DJ, Hauser W, Cohen SP, Fitzcharles MA (2020) Considering the potential for an increase in chronic pain after the COVID-19 pandemic. Pain 161:1694–1697
Chaturvedi SK (2020) Health anxiety, health-related life events, and somatization during COVID-19 pandemic can increase chronic pain. Pain 161:2652
Pinto F, Capodieci G, Setola FR et al (2012) Communication of findings of radiologic examinations: medicolegal considerations. Semin Ultrasound CT MRI 33(4):376–8. https://doi.org/10.1053/j.sult.2012.01.014 (PMID: 22824126)
Ezeldin M, Leonardi M, Princiotta C et al (2018) Percutaneous ozone nucleolysis for lumbar disc herniation. Neuroradiology 60(11):1231–1241. https://doi.org/10.1007/s00234-018-2083-4
Andreula CF, Simonetti L, De Santis F et al (2003) Minimally invasive oxygen-ozonetherapy for lumbar disk herniation. Am J Neuroradiol 24(5):996–1000
Muto M, Ambrosanio G, Guarnieri G et al (2008) Low back pain and sciatica: treatment with intradiscal-intraforaminal O(2)-O(3) injection. Our Experience Radiol Med 113(5):695–706. https://doi.org/10.1007/s11547-008-0302-5 (PMID:18594765)
Oder B, Loewe M, Reisegger M et al (2008) CTguidedozone/steroid therapy for the treatment of degenerative spinaldisease: effect of age, gender, disc pathology and multi-segmentalchanges. Neuroradiology 50:777e85
Lu W, Li YH, He XF (2010) Treatment of large lumbar disc herniation with percutaneous ozone injection via the posterior-lateral route and inner margin of the facet joint. World J Radiol 2(3):109–12. https://doi.org/10.4329/wjr.v2.i3.109
Macnab I (1971) Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Jt Surg Amm 53:891–903
Grabara M, Sadowska-Krępa E (2021) Musculoskeletal disorders and the physical activity of territorial army soldiers during the COVID-19 pandemic. BMC Musculoskelet Disord 22(1):796. https://doi.org/10.1186/s12891-021-04654-2
Morken T, Magerøy N, Moen BE (2007) Physical activity is associated with a low prevalence of musculoskeletal disorders in the royal Norwegian navy: a cross sectional study. BMC Musculoskelet Disord. 8(1):56. https://doi.org/10.1186/1471-2474-8-56
Ramani SL, Samet J, Franz CK, Hsieh C, Nguyen CV, Horbinski C et al (2021) Musculoskeletal involvement of COVID-19: review of imaging. Skeletal Radiol 50(9):1763–1773
Baig AM (2020) Chronic COVID syndrome: need for an appropriate medical terminology for long-COVID and COVID long-haulers. J Med Virol 93:2555–6
Kuppuswamy A (2017) The fatigue conundrum. Brain 140:2240–5
Funding
The authors declare that they recieved no funding for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical standards
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Somma, F., Negro, A., D’Agostino, V. et al. COVID-19 and low back pain: previous infections lengthen recovery time after intradiscal ozone therapy in patients with herniated lumbar disc. Radiol med 127, 673–680 (2022). https://doi.org/10.1007/s11547-022-01500-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-022-01500-w