Abstract
To evaluate the possible prognostic significance of the development of peripheral consolidations at chest x-ray in COVID-19 pneumonia, we retrospectively studied 92 patients with severe respiratory failure (PaO2/FiO2 ratio < 200 mmHg) that underwent at least two chest x-ray examinations (baseline and within 10 days of admission). Patients were divided in two groups based on the evolution of chest x-ray toward the appearance of peripheral consolidations or toward a greater extension of the lung abnormalities but without peripheral consolidations. Patients who developed lung abnormalities without peripheral consolidations as well as patients who developed peripheral consolidations showed, at follow-up, a significant worsening of the PaO2/FiO2 ratio but a significantly lower mortality and intubation rate was observed in patients with peripheral consolidations at chest x-ray. The progression of chest x-ray toward peripheral consolidations is an independent prognostic factor associated with lower intubation rate and mortality.
Similar content being viewed by others
Introduction
Portable chest x-ray (CXR) is widely used for the follow-up of lung abnormalities in coronavirus disease-19 (COVID-19). The most common CXR lung abnormalities in COVID-19 are lung consolidations, ground glass opacities (GGO) and reticular opacities [1,2,3,4,5,6]. One particular feature of COVID-19 pneumonia is the high frequency of peripheral lung involvement, often mimicking other inflammatory processes such as organizing pneumonia or eosinophilic pneumonia [1, 7, 8]. Chest computed tomography (CT) studies have shown peripheral involvement in 33–86% of patients, characterized by GGO in the early stages and greater prevalence of consolidations in more advanced stages [9,10,11]. Such peripheral lung involvement can be readily identified in CXR, especially when characterized by consolidations. CXR studies have reported 40–63% of exclusive involvement of the peripheral zone [3,4,5]. Although some studies have evaluated the prognostic significance of chest CT or CXR findings, they mainly took into consideration the total extent of the disease rather than a specific characteristic [6, 12, 13].
In this study, we evaluated the characteristics of patients who developed CXR peripheral consolidation and the possible prognostic significance of such finding.
Patients and methods
Patients
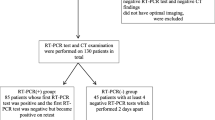
This was a retrospective study of patients admitted to our sub-intensive respiratory unit from September to December 2020 with SARS-CoV-2 infection confirmed by real-time RT-PCR on nasopharyngeal swab. The inclusion criteria were as follows: (1) patients with severe disease (defined by a PaO2/FiO2 ratio < 200 mmHg at nadir); (2) patients who underwent at least two CXR’s (one at admission and the second within 10 days of admission); (3) patients with lung abnormalities involving > 50% of the lung parenchyma or with peripheral consolidations in at least one of the two CXR’s. The study was conducted in compliance with the Declaration of Helsinki, with the approval of the local ethic committee.
We divided the patients based on the presence or absence of peripheral consolidations at baseline or follow-up CXR. Among the patients admitted in the study period, we arbitrarily selected the first 46 patients of the two groups among those that fulfilled the inclusion criteria. No patient was excluded for any reason after being considered in the first batch of 46 per group.
To investigate the prognostic significance of the appearance of peripheral consolidations on CXR in patients hospitalized for severe respiratory failure due to bilateral SARS-CoV-2 pneumonia we analyzed two clinically relevant outcomes, death within the hospitalization and the need for endotracheal intubation (ETI).
Chest x-ray
All patients underwent digital anteroposterior bedside CXR at full inspiration using a portable radiography unit at admission and within 10 days of admission. In an initial training set, 25 CXR’s were reviewed independently by two experienced thoracic radiologists (FC and UG) and also observed by two clinical pulmonologists (FN and VP). The remaining CXR’s were independently evaluated by the pulmonologists; results were compared, and when disagreement was found, final decisions were determined by consensus.
The finding considered in the evaluation of CXR were the presence and extension of reticular alterations, GGO and consolidations. CXR alterations were defined according to the Fleischner Society’s nomenclature [14]:
-
reticular alterations, as innumerable small linear opacities;
-
GGO, as areas of increased lung opacity, within which the margins of pulmonary vessels may be indistinct;
-
consolidation, as an increase in lung opacity that obscures the margins of the vessels and airway walls.
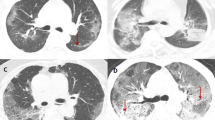
We have defined the extension of the lung abnormalities using a cut-off of 50% of lung fields and we have assigned a score of 1 if the lung abnormalities were extended less than 50% of the lung fields and a score of 2 if they were extended more than 50% of the lung fields. We have defined peripheral zones as areas beyond 2 cm from the lobar bronchial structures as far as visible [15]. We divided the patients on the basis of the presence or absence of peripheral consolidations at baseline or follow-up CXR (Fig. 1a–d).
Classification of chest x-ray. a Score 1, no peripheral consolidations: reticulations and GGO extended less than 50% of the lung fields, without peripheral consolidations. b Score 2, no peripheral consolidations: reticulations and GGO extended more than 50% of the lung fields, without peripheral consolidations. c Score 1 + peripheral consolidations: reticulations, GGO and consolidations extended less than 50% of the lung fields, presence of peripheral consolidations. d lung abnormalities (reticulations, GGO and consolidations) extended more than 50% of the lung fields, presence of peripheral consolidations. GGO ground-glass opacities
Statistical analysis
Data analysis was performed with SPSS software, version 25. Data were expressed as mean ± standard deviation or median [interquartile range] for normally distributed and non-normally distributed variables, respectively. Comparison between patient groups were performed with unpaired t-test and Mann–Whitney test as appropriate. Paired data were compared with paired t-test and paired Wilcoxon test. Multivariate logistic analysis was used to identify significant variables in predicting mortality. Two-side p values below 0.05 were considered statistically significant.
Results
A total of 92 patients was considered, mean age 70 ± 10 years; 78% were males.
Tables 1 and 2 describe the patients characteristics and the chest x-ray findings at hospital admission. The median time between onset of symptoms and the hospital admission was 6 days. Patients had a severe respiratory failure per inclusion criteria, lymphopenia with normal white blood cells, increased value of C-reactive protein (CRP) and procalcitonin (PCT). In 80% of cases PCT was < 0.55 ng/mL, commonly considered the threshold to suspect bacterial superinfection in COVID-19 [16]. Table 2 describes the chest x-ray findings at hospital admission. According to the onset of symptoms, we subdivided the chest x-ray in the 4 stages described in the literature [17, 18]: stage 1 (0–4 days), stage 2 (5–8 days), stage 3 (9–13 days) and stage 4 (≥ 14 days). Most patients (54.3%) were admitted to the hospital in stage 2 and had little extension of the lung abnormalities (70.7% had a score 1 of chest x-ray). Only 12% had peripheral consolidations, none of them in stage 1.
Patients repeated chest x-ray after a median time of 6.2 days. Table 3 shows demographic and laboratory findings at baseline and follow-up and the rate of negative outcome of patients subdivided in two groups according the presence of peripheral consolidations at follow-up.
Patients with peripheral consolidations were younger. Both groups had severe baseline respiratory failure that further worsened at follow-up, but with no significant difference between them. Both groups had similar neutrophil and lymphocyte count at baseline but at follow-up patients without peripheral consolidations had an increase in neutrophils and a strong reduction of lymphocytes. Furthermore, while the patients with peripheral consolidations had a reduction of CRP and PCT value at follow-up, those without peripheral consolidations showed a persistence of high values of these inflammatory markers. In particular, 30% of patients in the second group had a PCT value > 0.55 ng/mL, that is suspect for bacterial super-infection, albeit non diagnostic. The corresponding figure for patients in the first group was 6%.
Finally, we observed a significantly lower mortality and intubation rate in patients with peripheral consolidations at CXR (Table 3).
We performed a multivariate logistic analysis to investigate a composite outcome that combines mortality and the need for ETI and using age, baseline CRP, CRP Δ, lymphocytes Δ, PCT > 0.55 ng/mL at follow-up and the presence of peripheral consolidations at CXR as covariates. The presence of peripheral consolidations at CXR was an independent predictor of better prognosis (Table 4).
Discussion
The main purpose of this study was to investigate the prognostic significance of the appearance of peripheral consolidations on CXR in patients hospitalized for severe respiratory failure due to bilateral SARS-CoV-2 pneumonia. Our data show that in severe patients this type of radiographic response is associated with a better prognosis, with a significant reduction in the rate of intubation and mortality compared to patients who do not develop peripheral consolidations but go toward a greater extension of the lung abnormalities. While the development of peripheral consolidations is associated with clinical/laboratory characteristics suggestive of a better prognosis (lower age, higher lymphocyte count and lower CRP and PCT) it remained an independent predictor of good prognosis after controlling for such variables. This result is very important, especially in light of the fact that both groups of patients have the same baseline level of severity and the same worsening of respiratory failure within the first 10 days of hospitalization. Therefore, observing in such critical patients a radiographic evolution toward peripheral consolidations allows physicians to obtain important prognostic information. At the present time, CXR is the main radiologic tool for monitoring the progression of lung abnormalities in COVID-19, especially in critical patients admitted to sub-intensive and intensive care unit [19] and some studies have utilized a CXR scores to quantify the pulmonary involvement in COVID-19 and to predict the prognosis [2, 5, 6, 20, 21]. However, most such studies used scores that quantified the total extent of radiographic changes, without analyzing the prognostic significance of specific changes. An exception is represented by the study by Giraudo et al., which assessed the contribution of GGO and consolidations separately, attributing a worse prognosis to the latter. However, the consolidations described by Giraudo include all consolidations regardless of their localization [21].
We hypothesize that the same severity of respiratory failure in the two groups in our study is an expression of a greater impact on gas exchange of the consolidations (possibly due to the shunt effect), while the better prognosis in these patients is the expression of a less extensive disease. Further studies with chest CT scans associated with lung ultrasound or V/Q scan are warranted to further investigate this hypothesis. Indeed, as described in the work by Parra Gordo et al., which analyzed both CXR and computed tomography, the radiologic stage of peripheral consolidations would match with a moderate lung involvement with the pattern of organizing pneumonia, while the CXR stage characterized by diffuse pulmonary opacities would match with a severe lung involvement with radiologic pattern of diffuse alveolar damage [7]. In our study, both patient groups have a severity of respiratory failure corresponding to moderate-severe ARDS, and various studies show that ARDS with diffuse alveolar damage is associated with higher mortality than ARDS without diffuse alveolar damage [22, 23].
We found that the CXR evolution toward peripheral consolidations is associated with a lower age, a lower reduction of lymphocytes, a lower CRP and PCT value, features that have been previously shown to be associated with a better prognosis [12, 24,25,26,27,28]. On the contrary, we observed persistence of elevated value of CRP and PCT in the group of patients with lung abnormalities involving > 50% of the lung parenchyma but without peripheral consolidations. This observation might suggest that bacterial superinfection is responsible for the worst prognosis of patients without peripheral consolidations. However, some data in the literature show that PCT may be an indicator of disease severity in COVID-19 independent of bacterial superinfection [29]. Furthermore, all patients were treated with antibiotics per standard practice at the time, and in all patients with PCT > 0.55 antibiotic therapy was scaled up; therefore, it is not likely that the superinfection, when present, had a major impact in the outcome.
This study has limitations. First, it was retrospective. Second, we did not perform a correlation between CXR and CT findings, since in our center CXR was the main radiologic tool for monitoring the progression of lung abnormalities in COVID-19. Third, only 6 patients had a negative outcome (IOT or death) in the group of peripheral consolidations. Finally, another limitation of the present study is the use of portable CXR, that has lower quality compared to posteroanterior standard radiographs and in which evaluation of the left lower lobe is limited. However, this method has the advantages of limiting the movement of severe patients and to reduce environmental contamination.
In conclusion, according to our data, in severe COVID-19 patients the progression of CRX toward peripheral consolidations is an independent prognostic factor associated with lower intubation rate and mortality even in the presence of worsening respiratory failure; further studies are needed to confirm the significance of this finding and to understand the underlying pathophysiological and histopathological features.
Availability of data and materials
Data available on request from the authors.
References
Jacobi A, Chung M, Bernheim A, Eber C (2020) Portable chest X-ray in coronavirus disease-19 (COVID-19): a pictorial review. Clin Imaging 64:35–42. https://doi.org/10.1016/j.clinimag.2020.04.001
Yasin R, Gouda W (2020) Chest X-ray findings monitoring COVID-19 disease course and severity. Egypt J Radiol Nucl Med. https://doi.org/10.1186/s43055-020-00296-x
Vancheri SG, Savietto G, Ballati F, Maggi A, Canino C, Bortolotto C, Valentini A, Dore R, Stella GM, Corsico AG, Iotti GA, Mojoli F, Perlini S, Bruno R, Preda L (2020) Radiographic findings in 240 patients with COVID-19 pneumonia: time-dependence after the onset of symptoms. Eur Radiol 30(11):6161–6169. https://doi.org/10.1007/s00330-020-06967-7
Ippolito D, Maino C, Pecorelli A, Allegranza P, Cangiotti C, Capodaglio C, Mariani I, Giandola T, Gandola D, Bianco I, Ragusi M, Franzesi CT, Corso R, Sironi S (2020) Chest X-ray features of SARS-CoV-2 in the emergency department: a multicenter experience from northern Italian hospitals. Respir Med 170:106036. https://doi.org/10.1016/j.rmed.2020.106036
Wong HYF, Lam HYS, Fong AHT, Leung ST, Chin TWY, Lo CSY, Lui MMS, Lee JCY, Chiu KWH, Chung TWH, Lee EYP, Wan EYF, Hung IFN, Lam TPW, Kuo MD, Ng MY (2020) Frequency and distribution of chest radiographic findings in patients positive for COVID-19. Radiology 296(2):E72–E78. https://doi.org/10.1148/radiol.2020201160
Borghesi A, Maroldi R (2020) COVID-19 outbreak in Italy: experimental chest X-ray scoring system for quantifying and monitoring disease progression. Radiol Med (Torino) 125(5):509–513. https://doi.org/10.1007/s11547-020-01200-3
Parra Gordo ML, Buitrago Weiland G, GrauGarcía M, ArenazaChoperena G (2021) Aspectos radiológicos de la neumonía COVID-19: evolución y complicaciones torácicas. Radiologia 63(1):74–88. https://doi.org/10.1016/j.rx.2020.11.002
Smith DL, Grenier JP, Batte C, Spieler B (2020) A characteristic chest radiographic pattern in the setting of the COVID-19 pandemic. Radiol: Cardiothorac Imaging 2(5):e200280. https://doi.org/10.1148/ryct.2020200280
Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, Cui J, Xu W, Yang Y, Fayad ZA, Jacobi A, Li K, Li S, Shan H (2020) CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology 295(1):202–207. https://doi.org/10.1148/radiol.2020200230
Ng MY, Lee EYP, Yang J, Yang F, Li X, Wang H, Lui MM, Lo CS, Leung B, Khong PL, Hui CK, Yuen KY, Kuo MD (2020) Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol Cardiothorac Imaging 2(1):e200034. https://doi.org/10.1148/ryct.2020200034
Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A (2020) Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. Am J Roentgenol 215(1):87–93. https://doi.org/10.2214/ajr.20.23034
Feng Z, Yu Q, Yao S, Luo L, Zhou W, Mao X, Li J, Duan J, Yan Z, Yang M, Tan H, Ma M, Li T, Yi D, Mi z, Zhao H, Jiang Y, He Z, Li H, Nie W, Liu Y, Zhao J, Luo M, Liu X, Rong P, Wang W, (2020) Early prediction of disease progression in COVID-19 pneumonia patients with chest CT and clinical characteristics. Nat Commun 11(1):4968. https://doi.org/10.1038/s41467-020-18786-x
Liang W, Liang H, Ou L, Chen B, Chen A, Li C, Li Y, Guan W, Sang L, Lu J, Xu Y, Chen G, Guo H, Guo J, Chen Z, Zhao Y, Li S, Zhang N, Zhong N, He J, (2020) Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients With COVID-19. JAMA Int Med 180(8):1081–1089. https://doi.org/10.1001/jamainternmed.2020.2033
Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J (2008) Fleischner society: glossary of terms for thoracic imaging. Radiology 246(3):697–722. https://doi.org/10.1148/radiol.2462070712
Timmerman R, McGarry R, Yiannoutsos C, Papiez L, Tudor K, DeLuca J, Ewing M, Abdulrahman R, DesRosiers C, Williams M, Fletcher J (2006) Excessive toxicity when treating central tumors in a phase II study of stereotactic body radiation therapy for medically inoperable early-stage lung cancer. J Clin Oncol 24(30):4833–4839. https://doi.org/10.1200/jco.2006.07.5937
Pink I, Raupach D, Fuge J, Vonberg RP, Hoeper MM, Welte T, Rademacher J (2021) C-reactive protein and procalcitonin for antimicrobial stewardship in COVID-19. Infection 49:935–943. https://doi.org/10.1007/s15010-021-01615-8
Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, Zheng C (2020) Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19). Radiology 295:715–721. https://doi.org/10.1148/radiol.2020200370
Mazzei MA, Guerrini S, Zanoni M, Franchi F, Valente S, Cusi MG, Frediani B, Volterrani L (2021) Novel coronavirus (COVID-19) pneumonia: portable chest X-ray or computed tomography? An Italian perspective. Lung India 38:S72–S73. https://doi.org/10.4103/lungindia.lungindia_453_20
American College of Radiology. ACR recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection. https://www.acr.org/Advocacy-and-Economics/ACR-Position-Statements/Recommendations-for-Chest-Radiography-and-CT-for-Suspected-COVID19-Infection
Toussie D, Voutsinas N, Finkelstein M, Cedillo MA, Manna S, Maron SZ, Jacobi A, Chung M, Bernheim A, Eber C, Coincepcion J, Fayad ZA, Gupta YS (2020) Clinical and chest radiography features determine patient outcomes in young and middle-aged adults with COVID-19. Radiology 297(1):E197–E206. https://doi.org/10.1148/radiol.2020201754
Giraudo C, Cavaliere A, Fichera G, Weber M, Motta R, Pelloso M, Tosato F, Lupi A, Calabrese F, Carretta G, Cattelan AM, De Conti G, Cianci V, Navalesi P, Plebani M, Rea F, Vettor r, Vianello A, Stramare R, (2020) Validation of a composed COVID-19 chest radiography score: the CARE project. ERJ Open Res 6(4):00359–02020. https://doi.org/10.1183/23120541.00359-2020
Cardinal-Fernández P, Bajwa EK, Dominguez-Calvo A, Menéndez JM, Papazian L, Thompson BT (2016) the presence of diffuse alveolar damage on open lung biopsy is associated with mortality in patients with acute respiratory distress syndrome. Chest 149(5):1155–1164. https://doi.org/10.1016/j.chest.2016.02.635
Cardinal-Fernández P, Lorente JA, Ballén-Barragán A, Matute-Bello G (2017) Acute respiratory distress syndrome and diffuse alveolar damage. new insights on a complex relationship. Ann Am Thorac Soc 14(6):844–850. https://doi.org/10.1513/AnnalsATS.201609-728P
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet 395(10229):1054–1062. https://doi.org/10.1016/s0140-6736(20)30566-3
Liu Y, Yang Y, Zhang C, Huang F, Wang F, Yuan J, Wang Z, Li J, Feng C, Zhang Z, Wang L, Peng L, Chen L, Qin Y, Zhao D, Tan S, Yin L, Xu J, Zhou C, Jiang C, Liu L (2020) Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci 63(3):364–374. https://doi.org/10.1007/s11427-020-1643-8
Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, Xhang L, Zhou X, Du C, Zhang Y, Song J, Wang S, Chao Y, Yang Z, Xu J, Zhou X, Chen D, Xiong W, Xu L, Zhou F, Jiang J, Bai C, Zheng J, Song Y (2020) Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Int Med 180(7):934–943. https://doi.org/10.1001/jamainternmed.2020.0994
Liu J, Liu Y, Xiang P, Pu L, Xiong H, Li C, Zhang M, Tan j, Xu Y, Song R, Song M, Wang L, Zhang W, Han B, Tang L, Wang X, Zhou G, Zhang T, Li b, Wang Y, Chen Z, Wang X et al (2020) Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J Transl Med. https://doi.org/10.1186/s12967-020-02374-0
Rui HU, Chaofei H, Shiyao P, Mingzhu Y, Xiang C (2020) Procalcitonin levels in COVID-19 patients. Int J Antimicrob Agents 56:106051. https://doi.org/10.1016/j.ijantimicag.2020.106051
Heer RS, Mandal AK, Kho J, Szawarski P, Csabi P, Grenshaw D, Walker IA, Missouris CG (2021) Elevated procalcitonin concentrations in severe COVID-19 may not reflect bacterial co-infection. Ann Clin Biochem 58(5):520–527. https://doi.org/10.1177/00045632211022380
Funding
No funds were received for this research project.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Novelli Federica and Pinelli Valentina. The radiographic score was discussed and agreed with the radiologists Chiesa Fabio e Giannoni Ugo. The first draft of the manuscript was written by Novelli Federica and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics approval
The study was conducted in compliance with the Declaration of Helsinki, with the approval of the local ethic committee.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data. The submission does not include images that may identify the person.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Novelli, F., Pinelli, V., Chiaffi, L. et al. Prognostic significance of peripheral consolidations at chest x-ray in severe COVID-19 pneumonia. Radiol med 127, 602–608 (2022). https://doi.org/10.1007/s11547-022-01487-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-022-01487-4