Abstract
The purpose of this study was to compare the prognostic value of chest X-ray (CXR) and chest computed tomography (CT) in a group of hospitalized patients with COVID-19. For this study, we retrospectively selected a cohort of 106 hospitalized patients with COVID-19 who underwent both CXR and chest CT at admission. For each patient, the pulmonary involvement was ranked by applying the Brixia score for CXR and the percentage of well-aerated lung (WAL) for CT. The Brixia score was assigned at admission (A-Brixia score) and during hospitalization. During hospitalization, only the highest score (H-Brixia score) was considered. At admission, the percentage of WAL (A-CT%WAL) was quantified using a dedicated software. On logistic regression analyses, H-Brixia score was the most effective radiological marker for predicting in-hospital mortality and invasive mechanical ventilation. Additionally, A-CT%WAL did not provide substantial advantages in the risk stratification of hospitalized patients with COVID-19 compared to A-Brixia score.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ten months after the start of coronavirus disease (COVID-19) vaccination planning, the diffusion and virulence of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) are progressively decreasing in many parts of the world. On October 21, 2021, the number of new SARS-CoV2 infections in Italy was 3794, with 22 new admissions to intensive care units (ICUs), and 36 new deaths. There was a decrease in new infections by 90.7%, in new admissions to ICU by 63.3% for new admissions to ICUs, and in new deaths by 93.5% as compared to the peak of incidence observed on November 13, 2020 during the second wave of COVID-19 in Italy [1, 2].
Despite the progressive reduction in hospitalization and fatality rates in patients with COVID-19, ICU admissions and deaths are still observed [1]. Additionally, with the progressive lowering of temperatures in the coming months, an increase in new COVID-19 cases is anticipated.
Chest X-ray (CXR) and chest computed tomography (CT) are the most commonly used imaging techniques for the management (diagnosis, hospitalization, and follow-up) of patients with COVID-19 [3,4,5], and several authors have found that both modalities are useful predictors of patient outcome [6,7,8,9,10,11,12]. Recently, Sverzellati et al. [13] found that, in a simulated triage setting, the use of r-CXR (coronal image reconstructed from thin-section CT scan) in cases suspected of having COVID-19 was safe and helped optimizing both the use of radiology resources and patient management. However, to the best of our knowledge, the performance of CXR and chest CT for predicting adverse outcomes, such as invasive mechanical ventilation (IMV) and COVID-19 related mortality, has not yet been compared in the same cohort of hospitalized patients with COVID-19. Therefore, the aim of the present study was to retrospectively compare the prognostic value of CXR and chest CT at admission and during hospitalization in a group of patients with COVID-19.
Materials and methods
To compare the prognostic value of CXR and chest CT, we selected a cohort of patients with COVID-19, as confirmed by real-time polymerase chain reaction (RT-PCR), admitted to our hospital during the second wave (from October, 2020 to February, 2021) and for whom information on adverse outcomes (using IMV and in-hospital mortality) was available. We enrolled only patients from the second wave of COVID-19 because during the first wave, we almost exclusively used CXR because of the high pre-test probability of the disease.
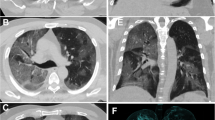
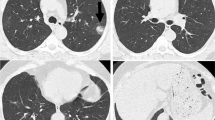
For the analysis, we selected only hospitalized patients who underwent both CXR and chest CT at admission (time interval between the two imaging modalities not exceeding 24 h). For each patient, CXR and chest CT performed at admission and CXRs performed during hospitalization were considered for the study. Each frontal chest projection was independently evaluated by a thoracic radiologist with 16 years of experience in thoracic imaging (A.B.), who ranked the pulmonary involvement of the disease based on a dedicated 18-point severity scale (the Brixia score) previously described by Borghesi and Maroldi [6]. On chest CT, the well-aerated lung (WAL) was quantified using a dedicated three-dimensional software (Syngo CT Pulmo 3D, Siemens Healthcare GMBH) by applying a method similar to that previously described by Colombi et al. [11]. The software-based calculation of the CT percentage of WAL at admission (A-CT%WAL) was independently performed by a radiology resident (S.G.) with three years of experience in thoracic imaging and one year of experience in using the software.
The data are presented as numbers (%) or as mean ± standard deviation for normally distributed data or as median and interquartile range (IQR) for non-normally distributed data. Relationships between adverse outcomes (using IMV and in-hospital mortality) and A-Brixia score (the score assigned on CXR at admission), H-Brixia score (the highest score assigned on CXRs during hospitalization), and A-CT%WAL were tested using univariate and multivariable logistic regression analyses. The predictive power of A-Brixia score, H-Brixia score, and A-CT%WAL was expressed as the area under the curve (AUC). Statistical analysis was conducted using MedCalc® Statistical Software version 20.009 (MedCalc Software Ltd, Ostend, Belgium). Statistical significance was set at p values < 0.05.
Results
According to the study inclusion criteria, we enrolled 106 consecutive patients (76 men and 30 women) with a mean age of 67.5 ± 13.8 years. Of the included patients, 14 (13.2%) died and 20 (18.9%) required IMV. The median values of the A-Brixia score, H-Brixia score, and A-CT%WAL were 4 (IQR, 2–4), 7 (IQR, 4–10), and 74.5% (IQR, 56–84%), respectively. The relationships between adverse outcomes and the A-Brixia score, H-Brixia score, and A-CT%WAL on logistic regression analyses are listed in Tables 1 and 2. The H-Brixia score was the most effective radiological marker for predicting in-hospital mortality (AUC, 0.877) and IMV (AUC, 0.856). Particularly, in multivariable analysis (using a stepwise approach), only the H-Brixia score was an independent predictive marker for adverse outcomes (Tables 1 and 2). Based on receiver operating characteristic curves, the optimal cutoff value for the H-Brixia score was 8 points with a sensitivity for in-hospital mortality and IMV of 92.9% and 85.0%, respectively (Figs. 1 and 2). Additionally, using the DeLong test, the AUC of A-Brixia score and A-CT%-WAL for predicting adverse outcomes did not show a significant difference (p > 0.415).
Discussion
Chest imaging modalities, specifically CXR and chest CT, play a key role in the management of patients with COVID-19. In February 2021, the World Health Organization (WHO) published a simple guide on the use of chest imaging techniques in patients with confirmed or suspected COVID-19[3]. For symptomatic patients with COVID-19, the WHO recommends chest imaging in addition to clinical and laboratory examinations to decide between patient discharge and hospitalization or to identify patients requiring specific therapeutic management [3].
However, one of the most challenging questions about chest imaging in symptomatic patients with COVID-19 is which imaging modalities between CXR and chest CT are the most effective for improving risk stratification of infected patients and predicting disease progression. Until now, the answer to this question remains unresolved as the published data on chest imaging lack a comparative analysis of the prognostic value of CXR and chest CT.
Although it is well known that chest CT is the most sensitive imaging technique for the detection of lung abnormalities, and quantitative CT analysis provides useful information for predicting disease progression [11, 12], CXR has several advantages for the management of hospitalized patients with COVID-19 [5, 6, 14]. The main advantage is the possibility of using CXR as a diagnostic tool to monitor (“day by day”) the course of the disease, especially in the most critically affected patients [5, 6, 14].
In our study cohort of hospitalized patients with COVID-19, we found that in the multivariable analysis, the H-Brixia score (the highest score assigned on CXRs during hospitalization) was the only independent predictor of adverse outcomes in hospitalized patients with COVID-19. In particular, the H-Brixia score exhibited excellent power in predicting in-hospital mortality and the need for IMV (Figs. 1 and 2). We also found that, at admission, chest CT with the quantitative assessment of the extent of WAL (A-CT%WAL) did not provide substantial advantages in the risk stratification of COVID-19 patients compared to CXR with semiquantitative assessment of the disease severity (A-Brixia score) (Tables 1 and 2). Therefore, similar to the study of Sverzellati et al. [13], we can state that in symptomatic patients with COVID-19 (confirmed by RT-PCR), chest CT should not be considered the first-line imaging modality to evaluate the extent of pulmonary involvement and decide between discharge and hospitalization because its prognostic power does not differ substantially from that of CXR.
Obviously, chest CT remains the most suitable radiological modality for confirming or excluding COVID-19 pneumonia, specifically in symptomatic patients with clinical suspicion of COVID-19 not confirmed by RT-PCR [3, 4, 15, 16]. In addition, chest CT remains the method of choice for confirming or excluding thoracic complications and sequelae of COVID-19, such as pulmonary embolism and fibrosis [17, 18].
The main limitations of our study include the retrospective design of the analysis and the relatively small sample size (106 patients). Another limitation is that the prognostic value of chest CT was evaluated only at admission because chest CT was performed in a limited number of patients during hospitalization, specifically when a pulmonary embolism was suspected.
In conclusion, this study confirmed that the H-Brixia score is an excellent marker for predicting adverse outcomes in hospitalized patients with COVID-19. Additionally, this study showed that at admission, the prognostic value of chest CT is not superior to that of CXR. These results are of great importance and will help both radiologists and clinicians in choosing the appropriate imaging modalities for management of symptomatic patients with COVID-19.
References
Italian Ministry of Health. COVID-19–Situation in Italy. http://www.salute.gov.it/portale/nuovocoronavirus/homeNuovoCoronavirus.jsp. Accessed 21 Oct 2021
Borghesi A, Golemi S, Carapella N, Zigliani A, Farina D, Maroldi R (2021) Lombardy, Northern Italy: COVID-19 second wave less severe and deadly than the first? a preliminary investigation. Infect Dis (Lond) 53:370–375. https://doi.org/10.1080/23744235.2021.1884745
Akl EA, Blažić I, Yaacoub S et al (2021) Use of chest imaging in the diagnosis and management of COVID-19: a WHO rapid advice guide. Radiology 298:E63–E69. https://doi.org/10.1148/radiol.2020203173
Rubin GD, Ryerson CJ, Haramati LB et al (2020) The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the fleischner society. Radiology 296:172–180. https://doi.org/10.1148/radiol.2020201365
Borghesi A, Sverzellati N, Polverosi R et al (2021) Impact of the COVID-19 pandemic on the selection of chest imaging modalities and reporting systems: a survey of Italian radiologists. Radiol Med 126:1258–1272. https://doi.org/10.1007/s11547-021-01385-1
Borghesi A, Maroldi R (2020) COVID-19 outbreak in Italy: experimental chest X-ray scoring system for quantifying and monitoring disease progression. Radiol Med 125:509–513. https://doi.org/10.1007/s11547-020-01200-3
Borghesi A, Zigliani A, Golemi S et al (2020) Chest X-ray severity index as a predictor of in-hospital mortality in coronavirus disease 2019: a study of 302 patients from Italy. Int J Infect Dis 96:291–293. https://doi.org/10.1016/j.ijid.2020.05.021
Cozzi D, Albanesi M, Cavigli E et al (2020) Chest X-ray in new Coronavirus Disease 2019 (COVID-19) infection: findings and correlation with clinical outcome. Radiol Med 125:730–737. https://doi.org/10.1007/s11547-020-01232-9
Balbi M, Caroli A, Corsi A et al (2021) Chest X-ray for predicting mortality and the need for ventilatory support in COVID- 19 patients presenting to the emergency department. Eur Radiol 31:1999–2012. https://doi.org/10.1007/s00330-020-07270-1
Maroldi R, Rondi P, Agazzi GM, Ravanelli M, Borghesi A, Farina D (2021) Which role for chest x-ray score in predicting the outcome in COVID-19 pneumonia? Eur Radiol 31:4016–4022. https://doi.org/10.1007/s00330-020-07504-2
Colombi D, Bodini FC, Petrini M et al (2020) Well-aerated lung on admitting chest CT to predict adverse outcome in COVID-19 pneumonia. Radiology 296:E86–E96. https://doi.org/10.1148/radiol.2020201433
Francone M, Iafrate F, Masci GM et al (2020) Chest CT score in COVID-19 patients: correlation with disease severity and short-term prognosis. Eur Radiol 30:6808–6817. https://doi.org/10.1007/s00330-020-07033-y
Sverzellati N, Ryerson CJ, Milanese G et al (2021) Chest x-ray or CT for COVID-19 pneumonia? Comparative study in a simulated triage setting. Eur Respir J. https://doi.org/10.1183/13993003.04188-2020
Vancheri SG, Savietto G, Ballati F et al (2020) Radiographic findings in 240 patients with COVID-19 pneumonia: time- dependence after the onset of symptoms. Eur Radiol 30:6161–6169. https://doi.org/10.1007/s00330-020-06967-7
Larici AR, Cicchetti G, Marano R et al (2020) Multimodality imaging of COVID-19 pneumonia: from diagnosis to follow-up. A comprehensive review. Eur J Radiol 131:109217. https://doi.org/10.1016/j.ejrad.2020.109217
Borakati A, Perera A, Johnson J, Sood T (2020) Diagnostic accuracy of X-ray versus CT in COVID-19: a propensity-matched database study. BMJ Open 10:e042946. https://doi.org/10.1136/bmjopen-2020-042946
Borghesi A, Aggiusti C, Farina D, Maroldi R, Muiesan ML (2020) COVID-19 pneumonia: three thoracic complications in the same patient. Diagnostics (Basel) 10:498. https://doi.org/10.3390/diagnostics10070498
Baratella E, Ruaro B, Marrocchio C et al (2021) Interstitial lung disease at high resolution CT after SARS-CoV-2-related acute respiratory distress syndrome according to pulmonary segmental anatomy. J Clin Med 10:3985. https://doi.org/10.3390/jcm10173985
Funding
The author states that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the 2013 version of the Declaration of Helsinki. This study was notified to our local ethics committee as a retrospective analysis. Given the retrospective nature of this analysis, performed with data collected in an anonymous manner, and in accordance with the current legislation, the need for informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Borghesi, A., Golemi, S., Scrimieri, A. et al. Chest X-ray versus chest computed tomography for outcome prediction in hospitalized patients with COVID-19. Radiol med 127, 305–308 (2022). https://doi.org/10.1007/s11547-022-01456-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-022-01456-x